Chapter 10 Scalp Reconstruction
The scalp represents one of the most visually homogenous and least anatomically complex regions of the head and neck. However, its unique characteristics and subtleties can often make reconstructive surgery in this area quite challenging. The scalp’s anatomy is unlike the anatomy in any other facial site, and this provides both benefits and drawbacks during reconstruction. The distribution of underlying muscle and the compartmentalization of the scalp by the galea are qualities that distinguish scalp anatomy. The presence of terminal hairs adds yet another unique feature that must be taken into consideration. Primary closures, flaps, and grafts can all be utilized to reconstruct the scalp, though their application techniques can be very different when compared to their uses on other parts of the face. The broad, inelastic nature of the galea, encompassing the scalp as a tendon-like sheath under constant tension, lends the scalp its relative immobility. As such, in comparison to facial skin, extensive undermining is often necessary during scalp reconstruction in order to achieve only small degrees of tissue movement. A thorough understanding of these aspects of the scalp is mandatory for attaining the best surgical outcome.1
SCALP SURGICAL ANATOMY
The scalp extends from the superior nuchal line posteriorly to the supraorbital rims anteriorly and is delineated by the pinnae bilaterally. The scalp is comprised of five layers: skin, subcutaneous connective tissue, galea, subaponeurotic loose areolar tissue, and pericranium. The skin is tethered to the underlying subcutaneous connective tissue and galea by muscle and fibrous bands. Local flaps commonly incorporate the outer three layers of the scalp, and flap undermining is easily performed through the subgaleal space, a relatively avascular plane.1
The galea consists of a thick membranous tendon (galea aponeurotica) that completely encases both the frontalis muscle anteriorly and the occipitalis muscle posteriorly. These muscles are joined in the midline by posterior and anterior extensions of the galea. The galea tightly wraps over the skull because of the antagonistic actions of the frontalis and occipitalis muscles. The temporoparietal muscles originate from the superficial temporal fascia and insert into the lateral border of the galea aponeurotica. Whereas the frontalis/galea/occipitalis are at the depth of the muscles of facial expression, the temporoparietalis is at the deeper level of the muscles of mastication. The subgaleal space lies over the pericranium on the crown of the scalp but extends over the temporoparietalis muscle laterally. This is important, as undermining should be performed in the relatively avascular subgaleal plane above the temporoparietalis muscle and under the frontalis and occipitalis muscles. The scalp areas associated with muscle and fascia exhibit greater mobility than the central regions that consist only of dense underlying galea. As such, more distensible flaps arise from the peripheral scalp, where the skin overlies the frontalis, occipitalis, and temporalis muscles (Figure 10.1).2
Blood vessels and sensory nerves traverse the scalp in a centripetal fashion through the subcutaneous connective tissue layer. The scalp’s abundant arterial supply is derived from the internal carotid system anteriorly (supraorbital and supratrochlear arteries) and from the external carotid system posteriorly (occipital, postauricular, and superficial temporal arteries). The extensive vascular anastomoses allow a single superficial temporal artery to provide sufficient blood supply to virtually the entire scalp; however, the midline scalp possesses a relative watershed zone where perfusion may be less predictable. The scalp lymphatic filtration system interlaces with medium-sized blood vessels in the subdermal and subcutaneous layers. Since the scalp lacks lymph nodes, there are no barriers to lymph flow. Lymph flows in a centrifugal pattern toward the parotid, occipital, preauricular, and postauricular areas.3
The ophthalmic branch of the fifth cranial (trigeminal) nerve provides sensation to the anterior scalp. The occipital nerve, a second cervical nerve derivative, supplies the posterior scalp. The auriculotemporal and maxillary nerves are responsible for sensation to the temple area while the great auricular nerve supplies the postauricular area.1 Infiltrating local anesthetic around the scalp’s periphery (through which all the sensory nerves traverse) can produce total scalp anesthesia.
EVALUATION OF THE SCALP DEFECT
The following questions need to be considered:
What is the depth of the wound? Is the wound through the skin, galea, or periosteum?
Some superficial wounds can appropriately heal by second intention and may even have hair regrowth if the depth of the wound does not extend below the level of the terminal hair bulbs. Most full-thickness wounds will require undermining in the subgaleal plane for tissue movement. Without an intact periosteum, a skin graft will not likely survive unless the underlying bone is burred to induce pinpoint bleeding.4
Is the defect surrounded by hair-bearing or glabrous skin?
BASIC RECONSTRUCTION CONCEPTS
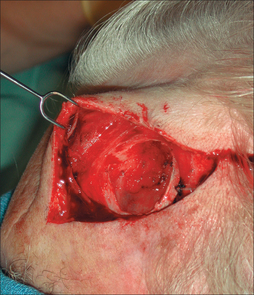
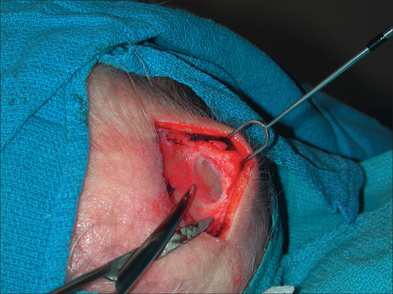
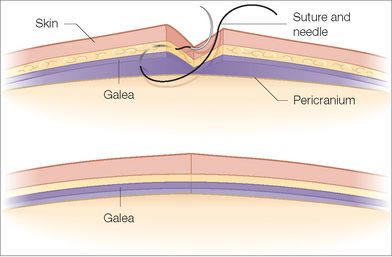
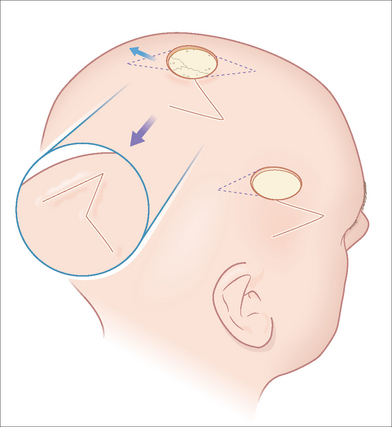
The scalp’s anatomy affords unique reconstructive advantages and disadvantages. The galea aponeurotica is the basis for this uniqueness. This stiff fascial layer is located beneath the subcutaneous connective tissue. Beneath it is the loose subaponeurotic connective tissue, also called the subgaleal space. This plane is relatively avascular, making it ideal for atraumatic undermining (Figure 10.2). Blunt dissection is all that is needed, and this can be achieved by scissor dissection or by simply using one’s gloved finger. This relative ease of undermining can be very deceptive, however, as the degree of additional movement afforded by wide undermining can be surprisingly small. For the best reconstructive outcome, the galea must be fully reapproximated. It is common for less experienced surgeons, particularly when confronted with very tense wounds, to not fully reapproximate the galea. In these cases, the final reapproximation of the wound’s edges involves stretching the overlying skin. The undesirable tension placed on the epidermal edges results in spread and inverted scars (Figure 10.3). It is therefore important that the galea be reapproximated by reaching underneath the leading edge of the defect and grabbing a large bite of galea with the suture needle (Figure 10.4). The strength of a properly realigned galea allows for minimal tension on the overlying skin, which leads to a more aesthetically appropriate scar.1 If proper wound eversion is not also present, the final scar will likely be less than ideal.
When confronted with an immobile scalp, the surgeon can enhance the movement of the scalp by performing a galeotomy. The classic galeotomy technique is accomplished by making linear scalpel incisions through the galea from within the essentially avascular subgaleal space. These incisions should be oriented parallel to the wound edge. The fenestrations expose overlying subcutaneous fat and allow the galea to effectively stretch. Galeotomies can be performed on large flaps without difficulty, as the skin is easily lifted to expose the flap’s undersurface. However, without special equipment such as scalp retractors, galeotomies are more difficult to perform during primary closures. In this setting, angling the scalpel blade to place fenestrations through the galea away from the wound edge is challenging because of limited exposure of the scalp’s undersurface. An electrosurgical apparatus set in the cutting mode can be utilized to reach farther back. The needle can be bent slightly upward to assist with this maneuver (Figure 10.5).
SECOND INTENTION HEALING
Dermatologic surgeons are accustomed to letting many wounds granulate. Second intention healing is indicated in patients who may not tolerate or desire extensive reconstructive surgery. Allowing the wound to heal by second intention can sometimes be the most appropriate wound management strategy for wounds on alopecic scalps. Often, the resultant scars are particularly cosmetically acceptable in these areas of the scalp where hair is absent.5
PRIMARY CLOSURE
Primary linear closure is often the best option for the reconstruction of smaller scalp wounds. The maximum defect diameter that can be closed by primary closure varies from patient to patient, but it is generally less than 3 cm (Figure 10.6). The surgeon can estimate whether a wound will close primarily by pushing on the sides of the defect. However, as mentioned earlier, this often overestimates the amount of actual tissue availability.
If the defect involves only the skin, the base of the wound should be deepened by removing the galea prior to closing the wound primarily. This deepening of the wound allows proper wide undermining in the subgaleal space. Wound closure tensions should be minimized, and galeotomies should be placed if appropriate. Spread scars resulting from unacceptably high wound closure tensions can be particularly noticeable in hair-bearing scalps because there is an absence of hair within the scars. Proper surgical technique can reduce this complication. Hair shafts on the scalp do not commonly grow at 90° angles to the skin. When appropriate, incisions in the scalp should be angled along the direction of hair growth in order to transect the fewest follicles. This will lead to more viable hair follicles at the scar’s edge. When bringing the wound edges together, the surgeon needs to initially reapproximate the galea in order to reduce tension on the overlying skin. It is helpful to use a suture such as 2-0 Vicryl (Ethicon Corp) on a PS-4 needle, as the smaller needle size facilitates grasping only the galea. One should not pass the suture needle through both the galea and dermis in one bite as this may lead to a more inverted wound. In fusiform elliptical closures, it may be helpful to place all the galeal sutures prior to tying them. Once in place, they can be tied starting from the ends of the wound so that the tension is reduced in the middle. The superficial skin can then be closed with staples, as they are occasionally easier to remove than sutures in hair-bearing regions. In the occipital scalp, however, sutures are occasionally preferred since staples tend to be less comfortable than sutures when they are compressed during sleep.
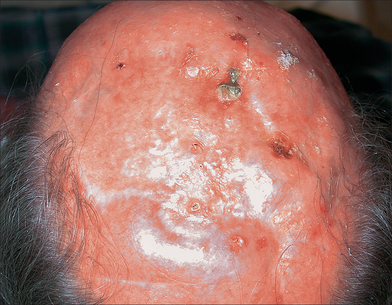
SPLIT-THICKNESS SKIN GRAFTS
Split-thickness skin grafting (STSG) is a convenient mode of reconstruction for larger defects on the scalp. Beyond the convenience, however, such grafts have a number of disadvantages. The cosmetic appearance of STSGs is often less than ideal because the grafts are typically depressed, shiny, and hairless (Figure 10.7). When healed, STSGs are often bound down to the underlying bone, and they therefore do not mimic the mobility of the normal scalp. The grafts are also sometimes quite fragile and susceptible to shearing forces. Often, a second intention scar has a better cosmetic appearance and is stronger than the STSG alternative.
The STSG does fill an important role in scalp reconstruction by allowing rapid coverage of larger surgical defects. The healing time of a STSG is typically less than the time required for a wound to granulate. In defects resulting from aggressive tumors, STSGs also allow for better tumor surveillance of the wound bed than flaps do. For the graft to survive, the recipient bed needs to be well vascularized. If the periosteum is absent, the vascularity of the underlying intact calvarium is insufficient to allow graft survival. In such cases, the outer table of the cranium needs to be burred to produce bleeding for graft nourishment. After burring the calvarium’s outer table, the STSG can then be placed in an immediate or delayed fashion. Delaying the graft placement enables the wound bed to partially granulate, potentially allowing for increased graft survival.
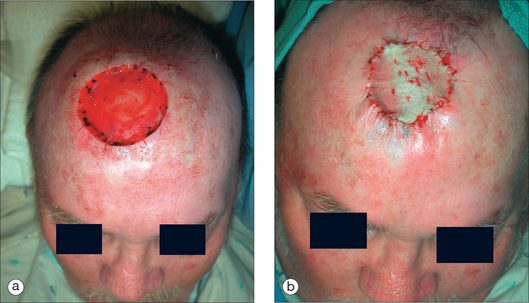
The defect size can also be slightly decreased by a purse-string closure prior to the application of the STSG. Although the amount of tissue movement produced by the purse-string closure is often relatively minimal, the diameter of the wound may be reduced by 10 to 30%. There are numerous variations to the purse-string technique. One method that works well on the scalp is the use of 2-0 Vicryl absorbable suture, where bites of the galea are taken in a circumferential fashion, tying the suture off within the wound so that it does not need to be removed at a later time. The STSG is then placed in the center of the remaining defect (Figure 10.8).4
FULL-THICKNESS SKIN GRAFTS
Because the Burow’s graft is typically quite small, the hair in the graft often survives, thereby restoring a cosmetically acceptable appearance. The advantage of this technique is that medium-sized defects that cannot not be closed primarily can be closed without the use of a larger flap. There is, however, a risk of graft failure, leading to an alopecic scar. If this does occur, the resulting scar can be excised at a later time when the surrounding tissue has relaxed and stretched through tissue creep.6
RANDOM PATTERN CUTANEOUS FLAPS
Regardless of classification schemes, flaps share common features that must be understood. The primary defect is the wound, often resulting from tumor removal, that is to be closed. The secondary defect is the defect created by the movement of the flap to close the primary defect. Secondary defects are more difficult to close in the relatively inelastic scalp. The primary motion is the predominant direction in which the flap is moved to close the primary defect. The secondary motion is the resultant motion on the surrounding skin caused by the primary motion. These concepts of primary and secondary motion (the effect of the flap on the surrounding skin) are very important in understanding the applications and limitations of local cutaneous flaps.7
Advancement Flaps
Pure advancement flaps are not commonly used in head and neck reconstruction because there is great limitation in the amount of tissue movement in a linear vector. In other words, wounds that cannot be closed in a simple linear manner will not often be amendable to closure using a unidirectional advancement flap, as the tension directions and magnitudes are essentially identical. One place where a traditional advancement flap is applicable is the upper forehead/frontal scalp region, where the flap’s incision lines can be hidden within the horizontal forehead creases that result from the repeated contraction of the frontalis muscle. The use of bilateral advancement flaps with the incisions placed along the forehead creases can nicely camouflage the inevitable scars. In order to minimize the standing cutaneous deformities that accompany tissue advancement, the incisions of the advancement flaps need to be long. The redundant Burow’s triangles can be removed to improve flap contour, but the required incisions will be perpendicular to the ideal horizontal incisions. Another technique that can reduce the “dog-ear” protrusions is the inward curving of the flap incisions to create wounds of unequal lengths. By doing so, the surgeon removes some of the dog-ear redundancy from the body of the flap instead of “pushing” the dog-ear laterally, where it must be excised vertically in order to achieve proper flap contour. One must make incisions into the body of the flap with care, as overzealous removal of tissue from these areas can compromise the flap’s vascular supply.8
A variation of the pure advancement flap, the O-to-T advancement flap is also useful on the upper forehead/frontal scalp region (Figure 10.9). The flap is particularly useful when the defect abuts the frontal hairline. The flap’s relaxing incisions are made bilaterally along the hairline, and the flap is elevated at the level of the subgaleal space, which in this case is underneath the frontalis muscle. For proper tension-free movement of the flap, the undermining needs to be extensive, and galeotomies are sometimes needed when tissue movement requirements are great. When the limbs of the O–T flap are advanced, a dog-ear redundancy will be present at the inferior aspect of the defect. This triangle is removed in a vertical direction to form the final incision lines in the shape of a “T.” Vertical scars on the forehead often spread less than horizontal scars and therefore remain aesthetically appropriate.
Rotation Flaps
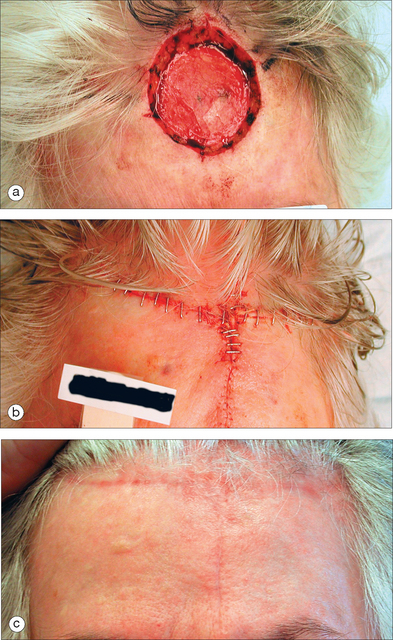
In medium to larger defects, a single rotation flap often recruits insufficient tissue to close the wound under sufficiently low tension, and the use of a double rotation flap, also called an O-to-Z closure, can be required (Figure 10.10). Defects on the crown of the scalp are especially amenable to this closure technique. The flap’s incisions should be made horizontal or parallel to the frontal hairline so that the scar does not extend on to the forehead. Although the two incisions are on the opposite sides of the defect, the arcs should curve in the same direction. In other words, they should both be designed to move either clockwise or counterclockwise. The two flaps are elevated then rotated from opposing directions, forming a “Z” shape (Figure 10.10).
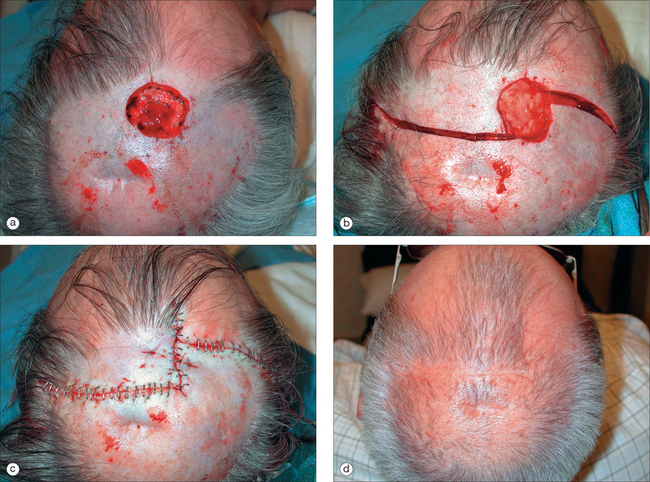
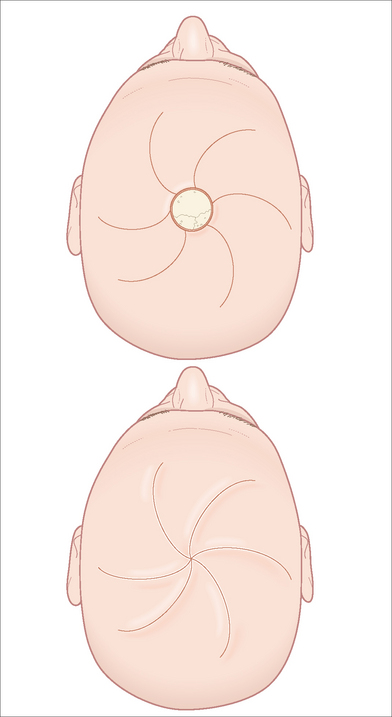
When the defect is large or the tissue is very inelastic, multiple rotation flaps may need to be used. The flaps’ incisions are placed equidistantly on the circumference of the circular defect with the arcs curving in the same direction. Multiple incisions can be placed, but three to six flaps are typically designed. The final appearance of the multiple rotation flaps is that of a pinwheel (Figure 10.11).9
Transposition Flaps
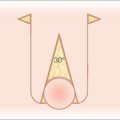
Transposition flaps are also called lifting flaps because the donor skin is lifted over intervening skin to fill the primary defect. These flaps are helpful in moving skin from a more mobile area such as the lateral scalp into a more immobile area such as the crown (Figure 10.12). The rhombic transposition flap and its variations are commonly used flaps in facial reconstructive surgery. The classic rhombic flap has the primary defect in the shape of a rhombus. The flap’s limb is projected at 120° from one of the corners of the defect, and the flap angle width is 60°. The disadvantage of this traditional flap design is that the transposition angle of 120° produces excess tension and a larger dog-ear removal. The DuFourmental and Webster variations of the rhombic flap are more practical techniques because the angles at the flap apices are smaller (60° and 30°, respectively), making the closure of the secondary defects much easier.10 When evaluating the suitability of a wound for a transposition flap repair, the skin around the defect is squeezed to see where there is maximal tissue laxity. In scalp reconstruction, tissue availability is typically located laterally. The origination of transposition flaps within loose skin will allow for easier closure of the secondary defect. After the flap is incised and lifted, the secondary defect is closed initially, which is in distinction to the technique typically used with sliding flaps. Initial closure of the secondary defect effectively “pushes” the flap into the primary defect and allows the flap to easily drape into the primary defect under minimal tension. A dog-ear will need to be removed opposite the secondary defect. Care must be taken not to make this incision across the flap’s base. Although the flap may be sutured under minimal tension, wide undermining of the defect is recommended in order to minimize the potential development of the trapdoor deformity. Transposition flaps typically trapdoor more than sliding flaps. Wide undermining of the flap’s recipient site allows the scar base to circumferentially contract, and may minimize the risk of flap protrusion during healing.11
1 Panje WR, Minor LB. Reconstruction of the scalp. In: Baker SR, Swanson NA, editors. Local flaps in facial reconstruction. St Louis, MO: Mosby; 1995:481-484.
2 Salache SJ, Bernstein G, Senkarik M. Scalp. In: Salache SJ, Bernstein G, Senkarik M, editors. Surgical anatomy of the skin. Norwalk, CT: Appleton & Lange; 1988:151-162.
3 Field LM. Scalp flaps. J Dermatol Surg Oncol. 1991;17:190-199.
4 Glogau RG, Haas AF. Skin grafts. In: Baker SR, Swanson NA, editors. Local flaps in facial reconstruction. St Louis, MO: Mosby; 1995:247-271.
5 Converse JM. The technique of closure of scalp defects. Clin Neurosurg. 1977;57:1011-1021.
6 Argenta LC. Controlled tissue expansion in facial reconstruction. In: Baker SR, Swanson NA, editors. Local flaps in facial reconstruction. St Louis, MO: Mosby; 1995:517-544.
7 Swanson NA. Basic techniques. In: Swanson NA, editor. Atlas of cutaneous surgery. Boston: Little, Brown; 1987:69-112.
8 Dzubow LM. Advancement flaps. In: Dzubow LM, editor. Facial flaps biomechanics and regional application. Norwalk, CT: Appleton & Lange; 1990:22-30.
9 Vecchione TR, Griffith L. Closure of scalp defects by using multiple flaps in a pinwheel design. Plast Reconstr Surg. 1978;62:74-80.
10 Bray DA. Rhombic flaps. In: Baker SR, Swanson NA, editors. Local flaps in facial reconstruction. St Louis, MO: Mosby; 1995:151-164.
11 Webster RC, Benjamin RJ, Smith RC. Treatment of “trapdoor deformity”. Laryngoscope. 1978;88:707-711.