CHAPTER 34 Sauvé-Kapandji Procedure after Distal Radius Fractures
Injuries to the distal radioulnar joint (DRUJ) with a distal radius fracture can cause ulnar-sided wrist pain, decreased forearm rotation, instability of the ulna, and loss of function. Controversy exists as to the treatment of this disorder. Some of the options include distal ulna resection (Darrach procedure),1 hemi-resection and interposition arthroplasty,2 matched distal ulna resection,3 and the Sauvé-Kapandji procedure.4 Satisfactory outcomes have been achieved using all of these procedures.2,3,5–14 Limitations of these procedures can include diminished grip strength, instability of the wrist, rupture of extensor tendons, and ulnar carpal abutment. Consistently good results can be difficult to achieve in young, active patients.15 In this chapter we discuss the use of the Sauvé-Kapandji procedure for treatment of DRUJ derangement after distal radius fractures.
History
The first description of a pseudarthrosis of the ulna performed for distal radioulnar pathology was recorded by Lauenstein in 1887. In 1921, Baldwin described a similar procedure with fixation of the DRUJ. The first detailed description of a fusion of the DRUJ with resection of bone just proximal to the fusion site was published by Louis Sauvé and Mehmed Kapandji in 1936.4 Since this publication, there have been several modifications proposed by different authors but the name “Sauvé-Kapandji procedure” has remained.
Indications
Mikkelsen and colleagues8 used “chronic ulnar wrist pain after Colles’ fracture” as the indication for the Sauvé-Kapandji procedure. George and associates6 stated that “severe and persistent pain in the DRUJ” was the primary indication for the Sauvé-Kapandji procedure. Ulnar-sided wrist pain after distal radius fracture can be the result of a variety of conditions, including DRUJ arthritis, DRUJ instability, and ulnocarpal abutment, all of which are conditions that may be caused or compounded by a malunion of the distal radius. It is our practice to define the pathology and try to restore normal anatomy before proceeding to the Sauvé-Kapandji procedure. For example, ulnar-sided pain in a patient with a malunion of the distal radius, with no arthritis of DRUJ, is offered a corrective osteotomy of the radius. A patient with mild instability of the DRUJ and a radius in at least a neutral palmer tilt is offered an ulnar-shortening osteotomy. If the DRUJ is unstable and there is no arthritis, we will first offer a ligament reconstruction for the DRUJ. Our indications for the Sauvé-Kapandji procedure after distal radius fracture are very specific: (1) active, high-demand patient with DRUJ arthritis and (2) failed ulnar shortening or ligament reconstruction for DRUJ instability.
Contraindications
The only true contraindication is inadequate bone stock at the DRUJ. Relative contraindications include heavy smoking or medical conditions that might adversely affect bone healing. Patients should understand the limits of the procedure. The Sauvé-Kapandji procedure will not improve extension and flexion of the wrist but is excellent at restoring near-normal forearm rotation. Grip strength is improved but does not return to normal levels, and return to work rates have varied. Pain is generally significantly improved but is still mildly to moderately present with the extremes of activity.6–9,12,13
Surgical Technique
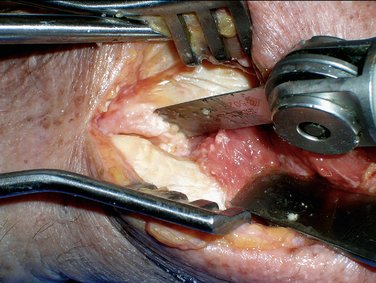
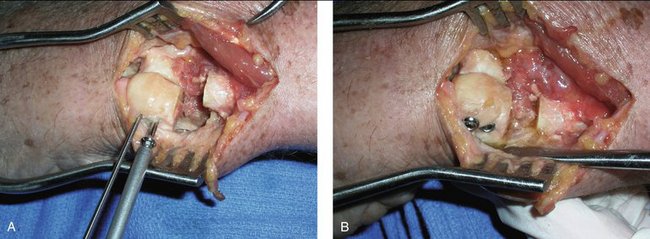
An incision is made between the fifth and sixth compartments to expose the distal portion of the ulna and the DRUJ (Fig. 34-1). Care should be taken to protect the dorsal sensory branch of the ulnar nerve. The joint capsule is elevated off of the DRUJ (Fig. 34-2). Reciprocal surfaces of the DRUJ are resected using a microsagittal saw (Fig. 34-3). The resulting space between the head of the ulna and the distal radius is measured (Fig. 34-4). A segment of bone of equivalent length is resected from the distal ulna to use as an intercalary graft (Fig. 34-5). The head of the ulna can be translated proximally to achieve ulnar-neutral variance (Fig. 34-6). When the head is in the desired position, additional ulna is resected to create a space of 10 mm (Fig. 34-7). The initial segment of resected ulna is placed between the head of the ulna and the radius and compressed with a tenaculum (Fig. 34-8). The head, graft, and radius are pinned with two cannulated wires spaced sufficiently apart to avoid impingement of the screw heads (Fig. 34-9). Wires are measured for the appropriate screw length. Partially threaded 4.0-mm screws are inserted to stabilize the DRUJ (Figs. 34-10 and Fig. 34-11).
Variations on the procedure have been described, including placing a portion of the pronator quadratus into the gap to encourage formation of a pseudarthrosis. Some authors have chosen to stabilize the proximal stump of the distal ulna with a distally based slip of the flexor carpi ulnaris or extensor carpi ulnaris.6,8,13,16
Results
No prospective, randomized trials have been performed to study the Sauvé-Kapandji procedure versus other methods of treatment for DRUJ derangement after distal radius fractures. We identified six articles in which the Sauvé-Kapandji procedure was used to treat DRUJ pathology after a distal radius fracture.6–1017
Indications ranged from persistent ulnar-sided wrist pain after distal radius fracture to salvage of a previously failed procedure. Most series have achieved excellent, reported near-normal forearm rotation (155 degrees arc), mild to moderate pain, unchanged wrist flexion-extension (arc of 80 to 120 degrees), an increased ability to return to work (few can return to 100% capacity of heavy labor work), and 85% satisfaction rating.4–18 The average Modified Wrist Score was 77, which correlated with a good result.6,7,9,10
Complications
The most commonly discussed complication of the Sauvé-Kapandji procedure is instability of the proximal stump. Different methods of stabilization have been proposed using either the pronator quadratus, a slip of the extensor carpi ulnaris tendon (distally based or proximally based), a slip of the flexor carpi ulnaris tendon, or imbrication of the adjacent tissues.6,8,13,16,19 More recently some surgeons have tried to control stump instability by using an ulnar head prosthesis seated in a cavity created in the remnant of the ulnar head.
1. Darrach W. Anterior dislocation of the head of the ulna. Ann Surg. 1912;56:802-803.
2. Bowers WH. Distal radioulnar joint arthroplasty: the hemiresection–interposition technique. J Hand Surg [Am]. 1985;10:169-178.
3. Watson HK, Ryu J, Burgess R. Matched distal ulnar resection. J Hand Surg [Am]. 1986;11:812-817.
4. Sauvé L, Kapandji M. Nouvelle technique de traitement chirurgical des luxations récidivantes isolées de l’extrémité inférieure du cubitus. J Chir (Paris). 1936;47:589-594.
5. Tulipan DJ, Eaton RG, Eberhart RE. The Darrach procedure defended, technique redefined and long-term follow-up. J Hand Surg [Am]. 1991;16:438-444.
6. George MS, Kiefhaber TR, Stern PJ. The Sauvé-Kapandji procedure and the Darrach procedure for the distal radio-ulnar joint dysfunction after Colles’ fracture. J Hand Surg [Br]. 2004;29:608-613.
7. Carter PB, Stuart PR. The Sauvé-Kapandji procedure for post-traumatic disorders of the distal radio-ulnar joint. J Bone Joint Surg [Br]. 2000;82:1013-1018.
8. Mikkelsen SS, Lindblad BE, Larsen ER, Sommer J. Sauvé-Kapandji operation for disorders of the distal radioulnar joint after Colles’ fracture. Acta Orthop Scand. 1997;68:64-66.
9. Jacobsen TW, Leicht P. The Sauvé-Kapandji procedure for posttraumatic disorders of the distal radioulnar joint. Acta Orthop Belg. 2004;70:226-230.
10. Lamey DM, Fernandez DL. Results of the modified Sauvé-Kapandji procedure in the treatment of chronic posttraumatic derangement of the distal radioulnar joint. J Bone Joint Surg Am. 1998;80:1758-1769.
11. Zimmerman R, Gschwentner M, Arora R, et al. Treatment of distal radioulnar joint disorders with a modified Sauvé-Kapandji procedure: long-term outcome with special attention to the DASH questionnaire. Arch Orthop Trauma Surg. 2003;123:293-298.
12. Low CK, Chew WYC. Results of Sauvé-Kapandji procedure. Singapore Med J. 2002;43:135-137.
13. Minami A, Iwasaki N, Ishikawa J, et al. Stabilization of the proximal ulnar stump in the Sauvé-Kapandji procedure by using the extensor carpi ulnaris tendon: long-term follow-up studies. J Hand Surg [Am].. 2006;31:440-444.
14. Gordon L, Levinsohn DG, Moore SV, et al. The Sauvé-Kapandji procedure for the treatment of post-traumatic distal radioulnar joint problems. Hand Clin. 1991;7:397-403.
15. Bain GI, Pugh DMW, MacDermid JC, et al. Matched hemiresection interposition arthroplasty of the distal radioulnar joint. J Hand Surg [Am]. 1995;20:944-950.
16. Field J, Majkowski RJ, Leslie IJ. Poor results of Darrach’s procedure after wrist injuries. J Bone Joint Surg Br. 1993;75:53-57.
17. Inagaki H, Nakamura R, Horii E, et al. Symptoms and radiographic findings in the proximal and distal ulnar stumps after the Sauvé-Kapandji procedure for treatment of chronic derangement of the distal radioulnar joint. J Hand Surg [Am]. 2006;31:780-784.
18. Sanders RA, Frederick HA, Hontas RB. The Sauvé-Kapandji procedure: a salvage operation for the distal radioulnar joint. J Hand Surg [Am]. 1991;16:1125-1129.
19. Rothwell AG, O’Neill L, Cragg K. Sauvé-Kapandji procedure for disorders of the distal radioulnar joint: a simplified technique. J Hand Surg [Am]. 1996;21:771-777.