Chapter 72 Risk Stratification for Sudden Cardiac Death
Sudden cardiac death (SCD) is defined as natural death from cardiac causes that occurs within 1 hour from the onset of symptoms. If unwitnessed, patients should have been seen alive within 24 hours preceding their death. Pre-existing heart disease may be known; nevertheless, SCD frequently affects persons with no previously recognized cardiovascular disorder.1 However, as documented by autopsy studies of 270 cases of SCD in individuals with no previously known heart disease, pathologic examination revealed structural abnormalities in 95%.2 The real incidence of SCD is difficult to establish, mainly because of the different definitions of SCD and the sources of data used in published reports. On the basis of the latest meta-analysis of reports published between 1980 and 2007, the estimated annual incidence of SCD in the United States varies from 180,000 to more 450,000 annually.3 SCDs account for approximately 50% of all cardiac deaths, and this proportion has remained constant despite the overall decline in cardiovascular death during the last decades.4,5 Recent decades have shown a steady decline in the total number of cardiac arrests, which is attributed mainly to a decrease in out-of-hospital ventricular fibrillation (VF). Nevertheless, survival after a cardiac arrest remains as low as 5%.5–8
Mechanisms of Sudden Cardiac Death
SCD may result from ventricular tachycardia (VT), VF, bradyarrhythmias, or pulseless electrical activity. Before the widespread use of implantable cardioverter-defibrillators (ICDs), data on the final arrhythmia leading to cardiac arrest could only be obtained from studies using Holter recordings, hospital telemetry, or both.9–13 The largest study to date on SCD episodes occurring while the patients were wearing a Holter monitor was published in 1989 by Bayes de Luna et al.12 Among 157 subjects, VT degenerating to VF was observed in 62% of cases, torsades de pointes in 13%, and primary VF in 8%. Only 17% of patients died from bradyarrhythmia. Conversely, the proportion of patients with bradyarrhythmia or electromechanical dissociation as a mechanism of SCD, as documented by Liu et al, may be higher in heart failure patients.13 This observation was later supported by the Metoprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure (MERIT-HF) trial, which showed that in heart failure patients, the mechanism of death depends on hemodynamic impairment. Patients with New York Heart Association (NYHA) heart failure class II to III are more likely die suddenly, whereas heart failure progression is responsible for the majority of those in NYHA class IV.14
Recent data based on electrocardiograms (ECGs), from implantable loop recorders in patients with prior myocardial infarction (MI) from the Cardiac Arrhythmias and Risk Stratification after Acute Myocardial Infarction (CARISMA) study confirmed that ventricular tachyarrhythmias were associated with SCDs, whereas bradyarrhythmia and electromechanical dissociation were predominantly observed in non-SCD and noncardiac deaths.15,16 The CARISMA study enrolled 312 patients with a recent acute MI (AMI) and left ventricular ejection fraction (LVEF) less than 40%. Terminal arrhythmias were recognized from loop recorders implanted 5 to 21 days after an AMI. During 2 years of follow-up, 26 patients died: 9 from SCDs, 10 from non-SCD cardiac causes, and 7 from noncardiac causes. Among those with SCD, VF was observed in 6 cases and bradyarrhythmia only in 1 (in 2 cases no rhythm was available for analysis). In contrast to previous Holter-based reports, initiation of VF (visible in 5 cases) was not preceded by VT in any of the cases. These data confirm that primary VF is the main mechanism of death in patients with prior MI and left ventricular dysfunction.
Multi-factorial Etiology of Sudden Cardiac Death: Impact on Risk Stratification
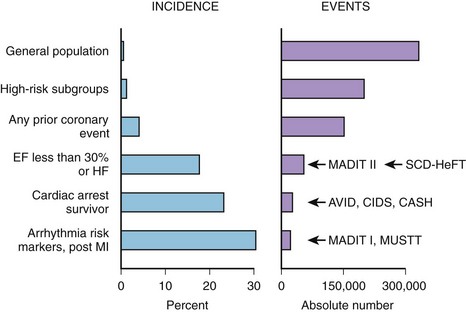
Coronary artery disease (CAD) remains the most common condition associated with SCD and is responsible for approximately 80% of cases.1 The highest risk of SCD is attributed to cardiac arrest survivors, and these patients are qualified for ICD implantation for secondary prevention of death. Indications for primary prevention of SCD are based on the underlying heart disease that was proven to increase the risk of arrhythmic events. Patients with prior MI and significantly depressed LVEF and those with heart failure or ventricular arrhythmia present with the highest incidence of SCD events.17,18 Nevertheless, as indicated by Myerburg et al in a review of the population impact of emerging ICD trials, the highest incidence of SCD is observed in survivors of out-of-hospital cardiac death and high-risk post-infarction subgroups, but the highest absolute number of SCD events occurs in large subgroups of patients at a somewhat lower risk, including patients with left ventricular dysfunction, congestive heart failure (CHF), or any prior coronary event (Figure 72-1).
The etiology of SCD is multi-factorial and involves a complex interplay among several elements, including genetic predisposition, cardiac condition, comorbidities, and environmental factors. Such a complex underlying etiology makes risk prediction of “unexpected” SCD events extremely complicated. The mechanisms of SCD include VT, VF, bradycardia, asystole, and pulseless electrical activity. Risk prediction is therefore focused mainly on predicting tachyarrhythmias, which can be prevented by ICD therapy. Life-threatening arrhythmias are preceded by a chain of events encompassing the complex interplay among the substrate, triggers, and modulators. Factors known to modulate and trigger arrhythmias include autonomic nervous system imbalance, transient ischemia, metabolic and electrolyte imbalance, transient volume overload of ventricles, and proarrhythmic action of drugs. Malignant arrhythmias are induced and sustained by a series of triggering and modulating events acting on the vulnerable myocardium.19
Role of Noninvasive Electrocardiology in Risk Stratification
Even though SCD is defined as being unexpected and frequently occurs as a first clinical event in previously asymptomatic persons, attempts have been made to identify risk markers indicating increased predisposition for arrhythmic events.20
Depressed EF that persists for years has been recognized as a major determinant of increased mortality rate, so the assessment of LVEF remains the gold standard in identifying patients who benefit from ICD therapy.17,21–24 The highest risk of death and SCD is attributed to a subgroup of patients with LVEF less than 30%. In comparison with earlier studies, recent series have suggested that the curve relating death to EF has “shifted to the left,” implying that for a given degree of left ventricular dysfunction, the increase in mortality rate is somewhat less than previously reported. Furthermore, the main drawback of EF in risk stratification lies in its low sensitivity and specificity.25,26
Noninvasive ECG parameters are believed to reflect the myocardial substrate as well as triggers and modulators potentially contributing to life-threatening arrhythmia risk. Therefore, the combination of ECG markers with low EF may potentially enhance risk stratification. Several ECG markers have been introduced into SCD risk stratification over the past few decades. Most of them have been associated with all-cause mortality and cardiac death. Nevertheless, the association with SCD is unclear, and the results of studies are conflicting.20,27–29 Detailed descriptions of specific risk stratification methods are available in other chapters in this text that detail these methods.
Electrocardiographic techniques include surface ECG, signal-averaged ECG (SAECG), ambulatory Holter monitoring, exercise tests, and other techniques such as baroreceptor sensitivity assessment. Surface ECG provides data on the underlying rhythm, resting heart rate, QRS duration, conduction abnormalities, QRS fragmentation, Q-T interval duration, and T-wave morphology or specific changes suggestive of primary electrical diseases.29–31
SAECG reveals the presence of late potentials reflecting heterogeneity of conduction in the myocardium. The presence of late potentials, prolonged filtered QRS duration, or both in the SAECG of patients with normal QRS duration on standard ECG indicates an increased risk of cardiac events. A broad QRS complex is associated with an increased risk of death, and patients with such conduction disturbances do not benefit from SAECG analyses.30,31
Long-term Holter monitoring allows evaluation of heart rate, ventricular ectopy, heart rate variability (HRV), heart rate turbulence (HRT), and dynamicity of repolarization.20,27–29 Ambulatory Holter monitoring is the most comprehensive tool for identifying and quantifying factors that may contribute to the mechanism of SCD (Figure 72-2). The effects of the autonomic nervous system on the heart could be evaluated by quantifying HRV, illustrating the relationship between the parasympathetic and sympathetic components of this system. HRT complements HRV analysis by providing insight into a baroreflex sensitivity component of central regulation of the cardiovascular system.28 Abnormalities of the central regulation of the heart are unlikely to cause SCD without an altered myocardial substrate and additional factors increasing the vulnerability of the myocardium to VT. The vulnerability of the myocardium may be expressed as impaired repolarization dynamicity, increased frequency and complexity of ventricular arrhythmias, and transient ischemic ST-T changes.
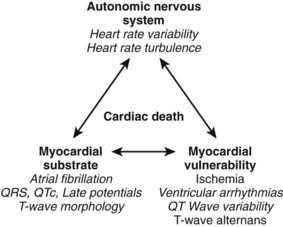
FIGURE 72-2 Factors contributing to cardiac death and respective Holter-derived electrocardiogram parameters.
(From Zareba W, Moss AJ: Noninvasive risk stratification in postinfarction patients with severe left ventricular dysfunction and methodology of the MUSIC II noninvasive electrocardiology substudy, J Electrocardiol 36[Suppl]:101–108, 2003.)
Exercise tests go beyond evaluating ST-T changes and provide additional information on the risk of SCD based on heart rate behavior and ventricular ectopy during the recovery phase.32 Microvolt T-wave alternans (TWA), considered to be a reflection of repolarization abnormalities, was originally determined during an exercise test, but numerous recent data support the equal value of TWA assessed by long-term monitoring.33,34
Invasive Electrophysiology Study
Testing the inducibility of VT in patients with prior MI has been a standard procedure for a number of years for identifying high-risk patients prone to SCD. Two primary prevention clinical trials—the Multicenter Automatic Defibrillator Implantation Trial (MADIT) and the Multicenter Unsustained Tachycardia Trial (MUSTT)—which enrolled patients with prior MI and depressed LVEF who presented with nonsustained VT (NSVT) and inducibility of ventricular tachyarrhythmias during invasive electrophysiology study (EPS), demonstrated that such a risk stratification algorithm was able to select a subset of patients with prior MI and a very high mortality risk.21,35 Nevertheless, secondary analysis from MUSTT revealed that despite significant differences in outcome between inducible patients enrolled in the trial and noninducible patients enrolled in a EPS registry, inducibility was found to be of limited use because the 5-year mortality rate in inducible patients was 48% compared with 44% in noninducible patients.36 Subsequently, MADIT II showed that additional risk stratifiers (including EPS) are not necessary when EF is severely depressed.22 In fact, in more than 80% of patients randomized to the ICD arm of MADIT II, invasive EPS, in an attempt to induce tachyarrhythmias, was performed at the time of ICD placement. Inducibility of ventricular arrhythmias, observed in 40% of studied patients, was not effective in identifying patients with cardiac events defined as VT, VF, or death.37 Therefore, MUSTT and MADIT II subanalyses suggested that in patients with substantially depressed left ventricular function, inducibility at EPS should not be considered a useful predictor of outcome. However, inducibility may have much better predictive value in patients with prior MI and an LVEF greater than 30% or less than 35%. Such a hypothesis was confirmed in a study by Cappato et al, who investigated the usefulness of inducibility in 285 survivors of cardiac arrest enrolled in the Cardiac Arrest Study Hamburg (CASH) trial and found that inducibility at EPS was predictive for SCD in patients with LVEF greater than 35% (hazard ratio [HR], 3.0; P = .006), whereas it was not useful in patients with lower LVEF (HR, 1.1; P = .81).38
Inducibility in patients with nonischemic cardiomyopathy has not been considered useful for predicting increased risk of death. However, data from the Defibrillators in Nonischemic Cardiomyopathy Treatment Evaluation (DEFINITE) substudy, which evaluated ICD-based inducibility of VT or VF, found that inducibility of either VT or VF was associated with an increased likelihood of subsequent ICD therapy for VT or VF.39
Bedside Risk Stratification Models
In risk stratification for SCD or cardiac death, attempts are frequently made to use sophisticated noninvasive or invasive methods reflecting ECG-based electrical myocardial involvement or autonomous nervous system regulation of the cardiovascular system. However, evaluating the risk of death could also be accomplished by using clinical parameters readily available to physicians when assessing patients in hospitals and in outpatient clinics. Retrospective data analyses from the ICD trials MADIT II, MUSTT, and the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) yielded risk stratification models based on such clinical variables.40–42
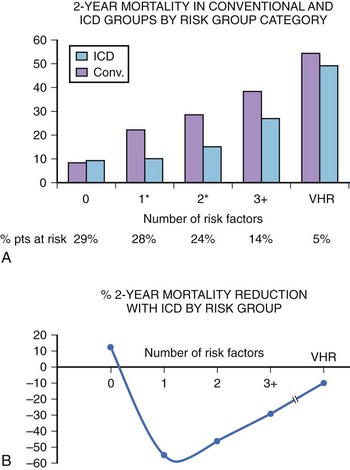
The simplest bedside risk stratification model was proposed by the MADIT II investigators, who evaluated five clinical factors: (1) NYHA class higher than class II, (2) age greater than 70 years, (3) blood urea nitrogen level greater than 26 mg/dL, (4) QRS duration greater than 0.12 seconds, and (5) atrial fibrillation (AF). Crude mortality rates in the conventional group were 8% and 28% in patients with zero or one or more risk factors, respectively, and 43% in very high-risk patients, who were defined by a blood urea nitrogen level of 50 mg/dL or more, serum creatinine level of 2.5 mg/dL or more, or both (Figure 72-3). Defibrillator therapy was associated with a 49% reduction in the risk of death (P < .001) among patients with one or more risk factors (n = 786), whereas no ICD benefit was identified in patients with no risk factors (n = 345; HR, 0.96; P = .91) and in very high-risk patients (n = 60; HR, 1.00; P > .99). This model could easily be adopted and could significantly improve low utilization of ICDs for primary prevention of death and SCD in patients with low EF and prior MI.
| Inducible VT | 17 |
| History of CHF | 19 |
| Patient enrolled as inpatient | 17 |
| EF ≤20% (for EF values between 20% and 40%, add one point for each EF percentage point >40) | 20 |
| EF = 40% | 0 |
| NSVT not discovered within 10 days after bypass grafting | 17 |
| IVCD or LBBB | 10 |
The SCD-HeFT investigators adopted the Seattle Heart Failure Model for predicting mortality and ICD benefit in their study population. The model included age, gender, systolic blood pressure, ischemic origin, NYHA class, LVEF, angiotensin-converting enzyme inhibitor use, angiotensin receptor blocker use, β-blocker use, statin use, furosemide equivalent daily dose in milligrams per kilogram, serum sodium, digoxin use, carvedilol use, and creatinine. This relatively complex model yielded scores categorizing patients in quintile subgroups. ICD treatment decreased the relative risk of SCD by 88% in the lowest risk group versus 24% in the highest risk group (P = .009 for interaction) and decreased the relative risk of total mortality by 54% in the lowest risk group versus no benefit (2%) in the highest risk group (P = .014 for interaction).41
The Muerte Subita en Insufficiencia Cardiaca (MUSIC) study was designed to evaluate risk predictors for SCD in patients with mild to moderate CHF (NYHA class II to III). In a cohort of 992 ambulatory patients, a risk score based on 10 variables (prior atherosclerotic vascular event, left atrial size >26 mm/m2, LVEF ≤35%, AF, LBBB or IVCD, NSVT, frequent ventricular premature beats [VPBs], estimated glomerular filtration rate <60 mL/min/1.73 m2, hyponatremia ≤138 mEq/L, N-terminal pro–B-type natriuretic peptide >1000 ng/L, and positive troponin) identified ambulatory patients with CHF at high risk of total mortality and SCD during follow-up.42
Risk Stratification in Patients with Prior Myocardial Infarction and Ischemic Cardiomyopathy
CAD remains the condition most commonly associated with SCD. Patients with prior AMI are at significant risk of SCD during the first few months after the index event. However, data from patients with AMI and heart failure or depressed EF indicate that during first 3 months, SCD is most frequently caused by recurrent MI or rupture of the ventricle.43 The risk of SCD from tachyarrhythmia tends to be relatively low during the first few years but increases in later years after MI when remote remodeling of the myocardium takes place. Yap et al, on the basis of a combined analysis of five multi-center trials that enrolled patients with prior MI and LVEF less than 40% or frequent VPBs, documented that in this high-risk subgroup the risk of arrhythmic death is higher than that of nonarrhythmic death for up to 2 years of post-infarction follow-up, with the highest risk during the first 6 months after MI.44 With time, the risk of arrhythmias decreases, but the risk of death from heart failure persists. Nevertheless, the absolute risk of death from any cause was the highest in the first 6 months after MI and decreased with time. Interestingly, nonarrhythmic death occurred more among females after 6 months. The risk of arrhythmic death was also higher in younger patients.44
Historically, detecting and quantifying Holter-recorded ventricular arrhythmias was the first ECG-based approach to determine the risk of patients with prior MI and to implement antiarrhythmic therapy.45 Ventricular arrhythmias are associated with acute ischemia caused by partial or total occlusion of coronary arteries. In patients with ischemic cardiomyopathy, monomorphic VT may result from re-entry mechanisms in the scarred areas of the myocardium. An association exists between the increased frequency and the complexity of ventricular arrhythmias with cardiac death and SCD. In a classic study by Bigger et al, the occurrence of 10 or more VPBs per hour was associated with an increased mortality rate.46 Subsequent results of the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI-2) trial confirmed that frequent VPBs (>10 per hour) were independently associated with SCD risk in the first 6 months after AMI in the thrombolytic era.47 Nevertheless, 10 years later, the presence of more than 10 VPBs per hour was associated only with non-SCD but not with SCD in the contemporary post-infarction population treated with modern primary coronary intervention procedures and widely used β-blockers. Conversely, the presence of NSVT was reported as an independent risk marker for SCD in patients with an LVEF less than 35%.48 It should be stressed that reducing ventricular arrhythmias with pharmacologic agents did not lead to improved survival and, in the case of several drugs, such therapy was associated with worse outcomes.49 Large day-to-day variabilities in NSVT detected by Holter monitoring further limit the use of this parameter as a risk stratifier. Primary prevention of SCD with ICD therapy was introduced by MADIT and MUSTT in patients with documented NSVT and inducibility of ventricular tachyarrhythmias.21,35 Nevertheless, after the MADIT II and SCD-HeFT trials, an EF of 30% or less is considered a sufficient risk stratifier without the need for documenting Holter-detected ventricular arrhythmias or inducible VT.22,24
As previously discussed, LVEF is the most acceptable measure of changes in the myocardial substrate. However, complementary information about the substrate may be obtained from electrocardiology. The parameters of interest include QRS duration and morphology (conduction disturbances), late potentials, and changes in repolarization duration and morphology. A wide QRS interval, particularly in relation to bundle branch block, has been consistently associated with worse prognosis, indicating increased risk of SCD as well as further deterioration of left ventricular function resulting in pump failure and death.31 The majority of recent data based on large clinical trials shows consistent association of prolonged QRS duration with all-cause, short-term, and long term mortality. Nevertheless, the association with SCD is not clear. Recent data based on contemporary population of patients with prior MI, the majority of whom were treated with percutaneous coronary intervention (PCI), showed that prolonged QRS (>120 ms) was associated with higher total and cardiac mortality but not with SCD.50 Discrepancy also exists in terms of QRS duration as a predictor of VT or VF therapy in patients with ischemic cardiomyopathy and ICDs. The Pacing Fast VT Reduces Shock Therapies (PainFREE II) study failed to document any relationship between QRS and VT or VF requiring ICD therapy.51 In patients from MADIT II with ischemic cardiomyopathy, a greater prolongation of baseline QRS was associated only with a trend toward increased benefit from ICD implantation.52 Subsequently, post hoc analysis of the MADIT II cohort showed that a prolonged QRS was associated with SCD risk only in the non-ICD arm, not in ICD recipients.53 It is therefore unclear whether QRS prolongation in the post-infarction cohorts may be considered an independent risk factor for SCD. It is probable that QRS should more likely be considered a surrogate of advanced myocardial disease related to the risk of subsequent events, which are, in turn, related to the development and progression of heart failure, but not as specific for arrhythmic events.
Late potentials refer to low-amplitude signals found at the end of the QRS complex that arise from areas of slow and heterogeneous conduction in a diseased myocardium and may represent and increased risk for subsequent cardiac arrhythmias. In patients with normal QRS duration, the presence of late potentials is a likely risk factor for cardiac events. Various studies in prethrombolytic era documented that abnormal SAECG may predict SCD in patients with prior MI.53,54 Data from MUSTT demonstrated that filtered QRS duration greater than 114 ms was independently associated with the primary study endpoint (arrhythmic death or cardiac arrest) during a 5-year follow-up.55 Patients with an abnormal SAECG had a 28% incidence of primary endpoints compared with 17% in those with normal SAECG (P < .001). The highest risk was found in a patients presenting with a combination of prolonged filtered QRS duration greater than 114 ms and EF less than 30%. Despite several studies that linked abnormal SAECG to arrhythmic events in patients with prior MI, SAECG is now alternatively used to identify low-risk patients, taking into account its high negative predictive value. Furthermore, it seems that in the reperfusion era with high rate of PCI procedures, late potentials lost their predictive value.56 An abnormal SAECG recorded in the early post-infarction period has insufficient predictive power, which seems to be overwhelmed by better predictive value of other ECG parameters (including HRT and TWA). However, data indicate that the combination of abnormalities in the SAECG with positive results of the TWA test might be useful in identifying high-risk individuals in the early post-infarction period.57,58
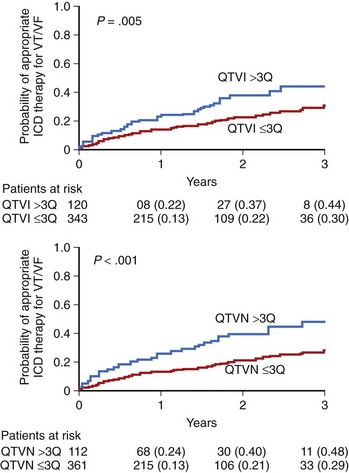
Static measures of QT duration and QT dispersion have been, for years, considered to be risk factors in patients with prior MI; however, their predictive value was usually overwhelmed by clinical covariates. Therefore more and more attention is now paid to dynamic measures of repolarization. The most commonly used method to evaluate QT dynamicity is to assess the relationship between the Q-T interval and the preceding R-R intervals expressed by the QT or R-R slope.29 A steeper slope indicates inappropriate shortening of the Q-T interval at higher heart rate and excessive lengthening of QT during low heart rate—both mechanisms significantly contributing to the risk of arrhythmic events. The dynamicity of the Q-T interval was found to be a potent risk marker of SCD. The Groupe d’Etude du Prognostic de l”Infarctus du Myocarde (GREPI) study demonstrated that a Q-T or R-R interval greater than 0.18 was independently associated with total mortality, with a stronger relationship with sudden cardiac death.59 An increased number of peaks of prolonged QTc interval—for example, the proportion of QTc intervals above the prespecified threshold (QTc >500 ms)—was described as a marker of life-threatening arrhythmias in patients with prior MI.60 A Q-T interval influenced by variety of factors may change in terms of duration as well a morphology. The ECG phenomenon consisting of beat-to-beat changes in repolarization duration and morphology appearing without the 2 : 1 pattern typical for TWA has been termed QT variability. These subtle beat-to-beat changes in T-wave amplitude and shape, as well as in QT duration, may be analyzed by several novel computerized ECG methods. These methods enable detection and quantification of microvolt-level changes, which otherwise remain undetected by the naked eye. Increased QT variability predicted arrhythmic events in the MADIT II population.61 The 2-year risk of VT or VF from Kaplan-Meier curves was twofold higher in patients in the highest quartile compared with those in lower quartiles for QT variability (QTVN) and QT variability index (QTVI) (P < .05 for each) (Figure 72-4). In multivariate Cox analysis, adjusted for significant clinical covariates, top-quartile QTVI and QTVN were independently associated with VT or VF (QTVN: HR, 2.18; 95% confidence interval [CI], 1.34 to 3.55; P = .002; QTVI: HR, 1.80; 95% CI, 1.09 to 2.95; P = .021).
Microvolt TWA (MTWA), which is the presence of 2 : 1 beat-to-beat changes in the amplitude of the T wave, has been shown to be associated with an increased risk of SCD and serious ventricular tachyarrhythmic events.62,63 In patients with ischemic cardiomyopathy, assessment of MTWA has been shown to be useful for predicting arrhythmic events. Bloomfield et al reported findings in 177 MADIT II–like patients who were assessed for MTWA and followed up for 2 years.63 They found that a positive MTWA was associated with a higher mortality rate than that associated with a QRS duration of greater than 120 ms. The actuarial mortality rate was 17.8% in patients with a positive MTWA compared with only 3.8% in MTWA-negative patients. It is noteworthy that most of the studies showed that MTWA carried a high negative predictive value of between 96% and 100%. This indicates that analysis of MTWA may be particularly helpful in avoiding unnecessary ICD implantation in patients with depressed left ventricular function who test negative for MTWA. Currently, MTWA is the only noninvasive ECG technique given class IIa indications for risk stratification, according to guidelines on ventricular arrhythmias and those on noninvasive risk stratification for SCD.17 Nevertheless, data from the Microvolt T-Wave Alternans Testing for Risk Stratification of Post-Myocardial Infarction Patients (MASTER) and Alternans Before Cardioverter Defibrillator (ABCD) trials indicated that MTWA is not as specific for arrhythmic events as previously believed.64,65
Traditional spectral analysis of MTWA requires an elevated and stabilized heart rate achieved by exercise or pacing. Within the past decade, several methods have been proposed to evaluate TWA from ECG recordings. However, the one known as modified moving average analysis has been the most extensively studied so far.66,67 In a small study by Verrier et al, Holter-based detection of TWA was associated with increased risk of arrhythmic events.68 This first report was further confirmed by findings from the Finnish Cardiovascular Study (FINCAVAS) and Epleronone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study (EPHESUS) trials.69,70 The Risk Estimation Following Infarction Non-invasive Evaluation (REFINE) study assessed TWA by the traditional spectral method from the exercise stress test as well as from the 20- to 30-minute ECG resting recordings following this stress test. Neither TWA techniques were predictive for the primary endpoint (cardiac death or resuscitated cardiac arrest) when assessed within the first 2 to 4 weeks after MI; however, they were independent risk markers when assessed 3 months after MI. TWA detected by modified moving average techniques was associated with a nearly threefold higher risk of cardiac death or resuscitated cardiac arrest during follow-up. Nevertheless, the best predictive model was provided by complex analysis of autonomic nervous system impairment assessed by HRT and the presence of electrical substrate expressed by TWA. The combination of abnormal Holter TWA and impaired HRT provided the highest HR at 4.18 (95% CI, 2.06 to 8.32; P = .001) to predict cardiac death or resuscitated cardiac arrest.71
Patients with prior MI are characterized by a scarred diseased myocardial substrate and impaired autonomic nervous tone. A variety of studies have explored the prognostic value of HRV parameters for predicting outcome in these patients.27,72–74 They have consistently shown that depressed HRV is associated with increased all-cause mortality or death from heart failure. Nevertheless, data on its prognostic significance for predicting SCD or arrhythmic death is limited and conflicting. Evidence for the association between depressed HRV parameters and SCD may be limited because of the difficulty in categorizing the sudden or arrhythmic nature of death but also could be because of a lack of strong evidence for this association. HRV also operates differently in different patient populations according to the disease and its advancement. Similarly, no studies exist that link HRV with EPS inducibility, further indicating that HRV may not be the right approach to identify susceptibility to arrhythmias. The past decade has shown an increased clinical interest in nonlinear dynamics of HRV methods for risk stratification purposes. A few studies have suggested that low levels of α1, a short-term scaling component of heart rate dynamics, is associated with increased mortality in patients with prior MI.48,75
HRT combines the assessment of three risk factors: HRV, PVBs, and baroreflex sensitivity.28 To date, the prognostic value of HRT has been documented in clinical studies enrolling more than 8000 patients with prior MI.28,76 Abnormal HRT has been proven to be an independent risk predictor of all-cause mortality and SCD in patients with prior MI. It is noteworthy that HRT works as a significant risk predictor in patients with an LVEF greater than 35%.77 The combination of abnormal autonomic nervous tone, reflected by abnormal deceleration capacity (a new parameter describing HRV related to slowing of heart rate), with blunted reactiveness of the autonomic nervous system reflected by impaired HRT, has been called severe autonomic failure and has proven to be of certain value in patients with prior MI and EF greater than 35%.78
The recently published CARISMA study findings have demonstrated that fatal or near-fatal arrhythmias in patients with prior MI and an LVEF less than 40% can be predicted by numerous risk markers, especially decreased HRV.15 HRV, HRT, arrhythmias, SAECG, TWA, and programmed electrical stimulation were assessed 1 and 6 weeks after AMI in patients with an EF of 40% or less measured between 3 and 21 days after MI. Of note, outof the 5869 acute MI patients screened in 10 European centers, only 23% presented with an LVEF of 40% or less assessed in the early post-infarction period. These data support the fact that modern treatment has significantly changed the clinical picture of patients with prior MI, and early invasive reperfusion strategies have led to a decreased number of patients with significantly impaired left ventricular function. Of the 312 patients enrolled in the CARISMA study, only 25 (8%) reached a primary endpoint, including 12 cases of symptomatic VT, 8 sudden deaths, 3 resuscitated cardiac arrests, and 2 instances of syncope. The primary endpoint was predicted by abnormal HRV, with the highest HR for left ventricular volume 5.7 or less (HR, 7; 95% CI, 2.4 to 20.3; P < .001), QT dispersion greater than 90 ms, SAECG QRS width 120 ms or more, and abnormal turbulence slope assessed at 6 weeks after MI as well as sustained monomorphic VT and sustained VT or VF evoked during programmed electrical stimulation. Neither an EF of 35% or less nor TWA were useful for risk stratification in the study population. Interestingly, HRV and HRT measured early after MI (1 week) were not predictive for arrhythmic event. This observation is consistent with previous results from the REFINE study.71 Despite strong evidence linking HRV and HRT with an increased risk of arrhythmic death, both are currently classified as class IIb indications for risk stratification in patients with ventricular arrhythmias.
Risk Stratification in Nonischemic Cardiomyopathy
A growing number of patients with nonischemic cardiomyopathy are being seen by cardiologists and are considered for prophylactic ICD therapy. On the basis of the results of the DEFINITE and SCD-HEFT trials, which showed benefit from ICD therapy in patients with nonischemic cardiomyopathy, indications for ICD include nonischemic cardiomyopathy with an EF of 35% or less for ICD therapy.17
Identifying patients with nonischemic cardiomyopathy who might benefit from ICD therapy more than other individuals remains a challenge. In contrast to patients with post-infarction cardiomyopathy, in patients with nonischemic cardiomyopathy, most risk stratification modalities were found to be of limited use. Invasive EPS with inducibility of ventricular arrhythmias is not useful as a risk stratification method. Several ECG-based noninvasive techniques have been studied, but the results are conflicting, and their application is therefore controversial.79
HRV, which is consistently associated with poor outcome in patients with prior MI, seems to have limited prognostic power in nonischemic patients. Grimm et al observed that neither HRV nor baroreflex sensitivity measures predicted major arrhythmic events in the 242 patients enrolled into the Marburg Cardiomyopathy database.80 However, an interesting application of HRV analysis was documented by Rashba et al in a subanalysis of the DEFINITE trial.81 Significant differences in mortality rates were observed between patients categorized according to standard deviation of normal-to-normal interval (SDNN) values. Patients with preserved HRV, defined as an SDNN greater than 113 ms, presented with a 0% mortality rate during a follow-up. It is therefore plausible that HRV may help identify low-risk patients with nonischemic cardiomyopathy.
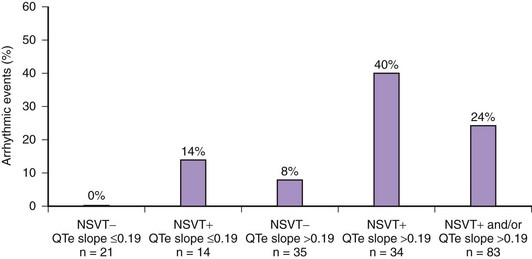
With regard to repolarization measures, independent prognostic value of QT dynamicity in patients with idiopathic dilated cardiomyopathy was reported by Iacoviello et al, who found that abnormal QT dynamicity was significantly associated with arrhythmic events (VT/VF or SCD) during a mean 39-month follow-up.82 The combination of steeper QTe slope (>0.19), decreased EF, and NSVT identified the group at the highest risk. It is worth emphasizing that QT or RR identified the higher risk group among patients with a low EF (<35%). The probability of arrhythmic events in patients with an EF less than 35%, NSVT, and increased QT or RR slope was as high as 40% (Figure 72-5). MTWA assessment seems to be of increasing interest in patients with dilated cardiomyopathy. Hohnloser et al studied 137 patients with dilated cardiomyopathy followed up for a mean 14 months. They found that decreased baroreflex sensitivity and the presence of MTWA were the only two significant predictors of arrhythmic events, outperforming other tested parameters such as NSVT, SAECG, EF, and HRV.83 The T-Wave Alternans in Patients With Heart Failure (ALPHA) study evaluated the prognostic value of MTWA in 446 patients with nonischemic dilated cardiomyopathy with NYHA II to III class heart failure and an EF less than 40%. Study findings showed that an abnormal TWA result was associated with a fourfold higher risk of cardiac death and life-threatening arrhythmias.84 In contrast, the SCD-HeFT TWA substudy did not demonstrate the usefulness of TWA in predicting life-threatening arrhythmias or ICD shocks.85 A 2009 meta-analysis on the role of TWA in risk stratification in nonischemic cardiomyopathy based on eight studies with nearly 1500 patients showed that a normal TWA test had a 96% negative predictive value and is useful in identifying low-risk patients who are unlikely to benefit from ICD therapy.86
Risk Stratification in Congestive Heart Failure
The occurrence of CHF is increasing among patients with cardiac diseases. The mode of death in patients with CHF depends mainly on the functional NYHA class, with SCD being predominant among patients with less advanced CHF and death from pump failure being predominant among those in NYHA class IV.14,87
VPBs can be found in up to 85% of patients with severe heart failure. Even though the relationship between ventricular arrhythmia and SCD is not clear, the majority of trials showed a significant association between the presence of NSVT and cardiac death.88–90 In the Captopril-Digoxin Multicenter Study, VPB, couplets, and NSVT were univariate predictors of total mortality.88 The presence of at least two episodes of NSVT was related with a threefold increase in total mortality and was an independent predictor of SCD. The Gruppo de Estudio de la Sobrevida en la Insuficiencia Cardiaca en Argentina (GESICA) trial documented that NSVT was associated with increased risk for both all-cause mortality and SCD.89 Spontaneous sustained VT is infrequent in Holter recordings, but if present, it predicts SCD.90
Decreased HRV and resting tachycardia are the common features seen in patients with CHF. The extent of HRV reduction correlates with the advancement of CHF expressed by EF, NYHA class, or brain natriuretic peptide levels.91 SDNN is the most extensively studied and best-validated HRV parameter. Similar to what was observed in patients with prior MI, reduction in HRV consistently predicts all-cause mortality and heart failure progression. However, it usually fails to predict SCD. In the UK-Heart Study, an SDNN less than 100 ms was associated with death from progressive heart failure but was not related to SCD.92 With regard to spectral methods, decreased low-frequency (LF) and very-low-frequency (VLF) components are the most frequently reported HRV measures related to death in CHF patients.93,94 However, different components of spectral analysis are related to different types of death. Decreased nighttime VLF values were related to progressive heart failure, whereas decreased nighttime LF values were associated with SCD.95
Data on the predictive value of HRT in patients with cardiomyopathies remain limited. In the Marburg Study, turbulence onset was found to be a significant predictor of transplant-free survival in 242 patients with idiopathic cardiomyopathy.96 In the UK-Heart Study, abnormal turbulence slope was found to be an independent risk predictor of death from decompensated heart failure.97 MUSIC findings showed that abnormal HRT was related to an increased risk of death and SCD in patients with mild-to-moderate heart failure, regardless of etiology (ischemic vs. nonischemic). However, consistent with the postulated mechanisms of HRT relating this phenomenon to abnormal baroreflex sensitivity and autonomic imbalance, abnormal HRT showed a trend toward a stronger association with death from heart failure than with SCD.98
Risk Stratification in Patients with Preserved Left Ventricular Function
A significant change in the clinical profile of survivors of MI has been seen in recent decades. Post-infarction populations from the 1970s to the 1980s ended up with an EF less than 30% in approximately one third of patients, whereas current data indicate that such values can be found in less than 10% of survivors of MI.15,26,78 More importantly, aggressive pharmacologic treatments may lead to further positive ventricular remodeling. Progress in the treatment of the acute phase of MI increases the chances of patients surviving and developing heart failure in the future. Therefore the current century has experienced a steady increase in the number of patients with heart failure and preserved EF, who may currently account for up to 40% to 50% of all patients with heart failure.99 The relative risk of death is lower in patients with preserved left ventricular function than in patients with significant left ventricular impairment, but the absolute number of patients at risk is high.18,99
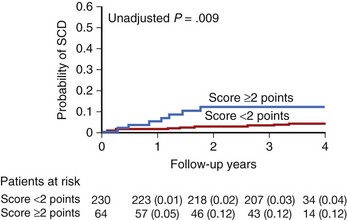
Among patients with stable CAD and preserved EF (>40%) from the Prevention of Events with Angiotensin Converting Enzyme Inhibition (PEACE) study, a simple clinical score that included age, gender, race, current angina, EF, prior revascularization, and diuretic and/or digitalis use, identified patients at risk of SCD. For risk stratification, 2 points were given for age older than 75 years, digitalis use, diuretic use, EF between 40% and 50%, and of non-white race; 1 point was given for male gender, age 65 to 75 years, current angina, and prior revascularization. The incidence of SCD at 4 years of follow-up was 0.8% for patients with a score 0 to 3 points, 2.2% for those with 4 to 6 points, and 10.4% for those with more than 6 points.100
With regard to noninvasive ECG risk stratification, data on the prognostic value of these parameters in patients with preserved LVEF is limited and the results are conflicting. Klinhengeben et al documented that in patients with prior MI and an EF greater than 35% treated with PCI for acute coronary syndromes, only patency of the infarct artery, but not autonomic markers such as baroreflex sensitivity or HRV, was significantly predictive for cardiac death or arrhythmic events.101 Barthel et al showed that in patients with prior MI and EF greater than 30%, a combination of abnormal HRT with age greater than 65 years and diabetes identified a group of patients at the highest risk of 2-year mortality.77 Makikalio et al confirmed that in the era of widely used PCI procedures and β-blockers, most of the Holter-based risk markers preserve their prognostic value and were particularly useful in patients with an EF greater than 35%. In a population of 2130 patients treated with coronary revascularization (70%) and/or β-blockers (94%), the incidence of SCD during a 2-year follow-up period was 1.8% in patients with an EF greater than 35% compared with 7.5% in patients with an EF of 35% or less. However, the total number of events was twofold higher in patients with preserved EF (35% vs.17%). Multivariate analysis showed that in patients with relatively preserved EF, SCD was independently predicted by the presence of an abnormal turbulence slope (HR, 4.7), NSVT (HR, 3.5), QRS of 120 ms or greater (HR, 3.2), and detrended fluctuation analysis less than 0.75 (HR, 2.7). Cumulative SCD rate was similar for patients with an EF of 35% or less and for those with an LVEF greater than 35% but with an abnormal turbulence slope.48
As documented by Bauer et al among patients with LVEF greater than 30%, the presence of severe autonomic failure identified a group with a 39% mortality rate compared with a 6% mortality rate in patients without such abnormality during a 5-year follow-up. After adjustment for age, diabetes mellitus, history of previous MI, gender, and arrhythmia on Holter monitoring, severe autonomic failure yielded a nearly fivefold higher risk of SCD (HR, 4.6; 95% CI, 3.1 to 7.0; P < .001).78
Autonomic nervous system measures and the parameters reflecting increased heterogeneity of repolarization have been proven to be useful in the risk stratification. In a Japanese prospective, multi-center study enrolling 1041 patients with prior MI, an EF of 40% or more, a positive MTWA test, and the presence of NSVT on Holter monitoring were significantly associated with serious arrhythmic events on multivariate analysis.102 The other method of TWA measurement with the modified moving average technique supported the usefulness of TWA test application in a population with preserved EF.103
The MUSIC study, which enrolled ambulatory patients with CHF in NYHA class II to III, documented that the risk of death in CHF patients with a relatively preserved EF (>35%) could be stratified by dynamic ECG measures. Patients with heart failure and an LVEF greater than 35% and abnormal ECG parameters had a 3-year mortality rate similar to those with significantly depressed left ventricular function. The scoring system, based on a combination of Holter-based parameters (turbulence slope, QT or RR slope, SDNN), identified patients at high risk of mortality and SCD during a more than 3-year follow-up. Patients with two or more abnormal risk markers were at risk of death (30% 3-year mortality rate) and SCD (12%), similar to death rates observed in patients with an LVEF of 35% or less (Figure 72-6). Interestingly, our study documented that, among patients with CHF with relatively preserved EF, traditional ECG risk markers such as increased heart rate, wide QRS, or frequent VPBs did not play a significant role in risk stratification. It seems that in this population, dynamic—not static—measures play a more important role. This could be explained by the presence of an early autonomic impairment in patients with still relatively preserved LVEF in the early stages of heart failure.104
Use of such a scoring system may be supported by another study by Watanabe et al, who, in a population of 680 patients with CHF from the Chronic Heart Failure Analyses and Registry in Tokushi District (CHART) study, identified an EF of less than 30%, left ventricular diastolic diameter greater than 60 mm, BNP level greater than 200 pg/mL, diabetes, and NSVT as significant risk predictors for SCD.105 The CHART patients with an LVEF of 30% or more and 0 to one risk markers were characterized by a very low mortality rate from SCD at 2 years of follow-up (2.8%) compared with 20% if the number of risk factors was three or more.
Ongoing trials will determine whether noninvasive risk markers can serve as indicators for ICD implantation in patients with an LVEF greater than 35% who are currently not covered by ICD implantation guidelines. REFINE will assess the prognostic value of Holter-based TWA and HRT assessment in patients with a history of recent MI and LVEF between 36% and 49%, and the Stratification of Autonomic Regulation for Risk Prediction in Postinfarction Patients with Preserved Left Ventricular Function (ISAR–ICD) study will assess the benefit from ICD therapy in patients stratified based on severe autonomic failure.106
Key References
Bauer A, Malik M, Schmidt G, et al. Heart rate turbulence: Standards of measurement, physiological interpretation, and clinical use: International Society for Holter and Noninvasive Electrophysiology Consensus. J Am Coll Cardiol. 2008;52:1353-1365.
Bayés de Luna A, Coumel P, Leclercq JF. Ambulatory sudden cardiac death: Mechanisms of production of fatal arrhythmia on the basis of data from 157 cases. Am Heart J. 1989;117:151-159.
Brenyo A, Zareba W. Prognostic significance of QRS duration and morphology. Cardiol J. 2011;1:8-17.
Buxton AE, Ellison KE, Lorvidhaya P, Ziv O. Left ventricular ejection fraction for sudden death risk stratification and guiding implantable cardioverter-defibrillators implantation. J Cardiovasc Pharmacol. 2010;55:450-455.
Cygankiewicz I, Zareba W, Vazquez R, et al. for the MUSIC Investigators: Risk stratification of mortality in patients with heart failure and left ventricular ejection fraction >35. Am J Cardiol. 2009;103:1003-1010.
Exner DV, Kavanagh KM, Slawnych MP, et al. Noninvasive risk assessment early after a myocardial infarction the REFINE study. J Am Coll Cardiol. 2007;50:2275-2284.
Goldberger JJ, Cain ME, Hohnloser SH, et al. American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society Scientific. Statement on noninvasive risk stratification techniques for identifying patients at risk for sudden cardiac death. J Am Coll Cardiol. 2008;52:1179-1199.
Haigney MC, Zareba W, Gentlesk PJ, et al. QT interval variability and spontaneous ventricular tachycardia or Huikuri HV, Raatikainen MJ, Moerch-Joergensen R, et al, for the CARISMA (Cardiac Arrhythmias and Risk Stratification after Acute Myocardial Infarction) study group: Prediction of fatal or nearly fatal cardiac arrhythmia events in patients with depressed left ventricular function after an acute myocardial infarction, for the Multicenter Automatic Defibrillator Implantation Trial II investigators. Eur Heart J. 2009;30:689-698.
Kong MH, Fonarow GC, Peterson ED, et al. Systematic review of the incidence of sudden cardiac death in the United States. J Am Coll Cardiol. 2011;57:794-801.
Makikallio TH, Barthel P, Schneider R, et al. Prediction of sudden cardiac death after acute myocardial infarction: role of Holter monitoring in the modern treatment era. Eur Heart J. 2005;26:762-769.
Myerburg RJ, Castellanos A. Cardiac arrest and sudden cardiac death. In Libby P, Bonow RO, Mann DL, Zipes DP, editors: Braunwald’s heart disease. A textbook of cardiovscular medicine, ed 8, Philadelphia: Saunders Elsevier, 2011.
Nieminen T, Verrier RL. Usefulness of T-wave alternans in sudden death risk stratification and guiding medical therapy. Ann Noninvasive Electrocardiol. 2010;15:276-288.
Zipes DP, Camm AJ, Borggrefe M, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: A report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines. Circulation. 2006;114:e385-e484.
1 Myerburg RJ, Castellanos A. Cardiac arrest and sudden cardiac death. In Libby P, Bonow RO, Mann DL, Zipes DP, editors: Braunwald’s heart disease: A textbook of cardiovscular medicine, ed 8, Philadelphia: Saunders Elsevier, 2011.
2 Chugh SS, Kelly KL, Tits JL. Sudden cardiac death with apparently healthy heart. Circulation. 2000;102:649-654.
3 Fox CS, Evans JC, Larson MG, et al. Temporal trends in coronary artery mortality and sudden cardiac death from 1950 to 1999: The Framingham Heart Study. Circulation. 2004;110:522-527.
4 Kong MH, Fonarow GC, Peterson ED, et al. Systematic review of the incidence of sudden cardiac death in the United States. J Am Coll Cardiol. 2011;57:794-801.
5 Chugh SS, Reinier K, Teodorescu C, et al. Epidemiology of sudden cardiac death: Clinical and research implications. Prog Cardiovasc Dis. 2008;51:213-218.
6 Cobb LA, Fahrenbruch CE, Olsufka M, et al. Changing incidence of out-of-hospital ventricular fibrillation, 1980–2000. JAMA. 2002;288:3008.
7 Herlitz J, Andersson E, Bang A, et al. Experiences from treatment of out-of-hospital cardiac arrest during 17 years in Goteborg. Eur Heart J. 2000;21:1251-1258.
8 Parish DC, Dinesh Chandra KM, Dane FC. Success changes the problem: Why ventricular fibrillation is declining, why pulseless activity is emerging and what to do about it. Resuscitation. 2003;58:31-35.
9 Pratt CM, Francis MJ, Luck JC, et al. Analysis of ambulatory electrocardiograms in 15 patients during spontaneous ventricular fibrillation with special reference to preceding arrhythmic events. J Am Coll Cardiol. 1983;2:789-797.
10 Kempf FC, Josephson ME. Cardiac arrest on ambulatory electrocardiograms. Am J Cardiol. 1984;53:1577-1582.
11 Olshausen KV, Witt T, Pop T, et al. Sudden death while wearing a Holter monitor. Am J Cardiol. 1991;67:381-386.
12 Bayés de Luna A, Coumel P, Leclercq JF. Ambulatory sudden cardiac death: Mechanisms of production of fatal arrhythmia on the basis of data from 157 cases. Am Heart J. 1989;117:151-159.
13 Liu M, Stevenson WG, Stevenson LW, et al. Diverse mechanisms of unexpected cardiac arrest in advanced heart failure. Circulation. 1989;80:1675-1680.
14 MERIT-HF Investigators. Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL randomized intervention trial in congestive heart failure (MERIT-HF). Lancet. 1999;353:2001-2007.
15 Huikuri HV, Raatikainen MJ, Moerch-Joergensen R, et al. for the CARISMA (Cardiac Arrhythmias and Risk Stratification after Acute Myocardial Infarction) study group: Prediction of fatal or nearly fatal cardiac arrhythmia events in patients with depressed left ventricular function after an acute myocardial infarction. Eur Heart J. 2009;30:689-698.
16 Gang UJO, Jons C, Jorgensen RM, et al. Heart rhythm at the time of death documented by an implantable loop recorder. Europace. 2010;12:254-260.
17 Zipes DP, Camm AJ, Borggrefe M, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: A report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines. Circulation. 2006;114:e385-e484.
18 Myerburg RJ, Kessler KM, Castellanos A. Sudden cardiac death: Epidemiology, transient risk, and intervention assessment. Ann Intern Med. 1993;119:1187-1197.
19 Bayés-Genís A, Viñolas X, Guindo J, et al. Electrocardiographic and clinical precursors of ventricular fibrillation: Chain of events. Cardiovasc Electrophysiol. 1995;6:410-417.
20 Goldberger JJ, Cain ME, Hohnloser SH, et al. American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society. Scientific statement on noninvasive risk stratification techniques for identifying patients at risk for sudden cardiac death. J Am Coll Cardiol. 2008;52:1179-1199.
21 Moss AJ, Hall WJ, Cannom DS, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmias. N Engl J Med. 1996;335:1933-1940.
22 Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction, for the Multicenter Automatic Defibrillator Implantation Trial II Investigators. N Engl J Med. 2002;346:877-883.
23 Kadish A, Dyer A, Daubert JP, et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy, for the Defibrillators in Non-Ischemic Cardiomyopathy Treatment Evaluation (DEFINITE) Investigators. N Engl J Med. 2004;350:2151-2158.
24 Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure, for the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. N Engl J Med. 2005;352:225-237.
25 Buxton AE, Ellison KE, Lorvidhaya P, Ziv O. Left ventricular ejection fraction for sudden death risk stratification and guiding implantable cardioverter-defibrillators implantation. J Cardiovasc Pharmacol. 2010;55:450-455.
26 Buxton AE, Lee KL, Hafley GE, et al. Limitations of ejection fraction for prediction of sudden death risk in patients with coronary artery disease: Lessons from the MUSTT study, for the MUSTT Investigators. J Am Coll Cardiol. 2007;50:1150-1157.
27 Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability. Standards of measurement, physiological interpretation and clinical use. Circulation. 1996;93:1043-1065.
28 Bauer A, Malik M, Schmidt G, et al. Heart rate turbulence: Standards of measurement, physiological interpretation, and clinical use: International Society for Holter and Noninvasive Electrophysiology Consensus. J Am Coll Cardiol. 2008;52:1353-1365.
29 Zareba W, Bayes de Luna A. QT dynamics and variability. Ann Noninvasive Electrocardiol. 2005;10:256-262.
30 Zareba W, Moss AJ. Noninvasive risk stratification In postinfarction patients with severe left ventricular dysfunction and methodology of the MUSIC II noninvasive electrocardiology substudy. J Electrocardiol. 2003;36(Suppl):101-108.
31 Brenyo A, Zareba W. Prognostic significance of QRS duration and morphology. Cardiol J. 2011;1:8-17.
32 Kligfield P, Lauer MS. Exercise electrocardiogram testing: beyond the ST segment. Circulation. 2006;114:2070-2082.
33 Cutler MJ, Rosenbaum DS. Risk stratification for sudden cardiac death: Is there a clinical role for T wave alternans? Heart Rhythm. 2009;6(8 Suppl):S56-S61.
34 Nieminen T, Verrier RL. Usefulness of T-wave alternans in sudden death risk stratification and guiding medical therapy. Ann Noninvasive Electrocardiol. 2010;15:276-288.
35 Buxton AE, Lee KL, Fisher JD, et al. A randomized study of the prevention of sudden death in patients with coronary artery disease, for the Multicenter Unsustained Tachycardia Trial Investigators. N Engl J Med. 1999;341:1882-1890.
36 Buxton AE, Lee KL, DiCarlo L, et al. Electrophysiologic testing to identify patients with coronary artery disease who are at risk for sudden death. N Engl J Med. 2000;342:1937-1945.
37 Daubert JP, Zareba W, Hall WJ, et al. Predictive value of ventricular arrhythmia inducibility for subsequent ventricular tachycardia or ventricular fibrillation in Multicenter Automatic Defibrillator Implantation Trial (MADIT) II patients, for the MADIT II Study Investigators. J Am Coll Cardiol. 2006;47:98-107.
38 Cappato R, Boczor S, Kuck KH. Response to programmed ventricular stimulation and clinical outcome in cardiac arrest survivors receiving randomized assignment to implantable cardioverter defibrillator or antiarrhythmic drug therapy. Eur Heart J. 2004;25:642-649.
39 Daubert JP, Winters SL, Subacius H, et al. Ventricular arrhythmia inducibility predicts subsequent ICD activation in nonischemic cardiomyopathy patients: A DEFINITE substudy, for the Defibrillators In Nonischemic Cardiomyopathy Treatment Evaluation (DEFINITE) Investigators. Pacing Clin Electrophysiol. 2009;32:755-761.
40 Goldenberg I, Vyas AK, Hall WJ, et al. Risk stratification for primary implantation of a cardioverter-defibrillator in patients with ischemic left ventricular dysfunction, for the MADIT-II Investigators. J Am Coll Cardiol. 2008;51:288-296.
41 Levy WC, Lee KL, Hellkamp AS, et al. Maximizing survival benefit with primary prevention implantable cardioverter-defibrillator therapy in a heart failure population. Circulation. 2009;120:835-842.
42 Vazquez R, Bayes-Genis A, Cygankiewicz I, et al. The MUSIC Risk score: A simple method for predicting mortality in ambulatory patients with chronic heart failure, for the MUSIC Investigators. Eur Heart J. 2009;30:1088-1096.
43 Pouleur AC, Barkoudah E, Uno H, et al. Pathogenesis of sudden unexpected death in a clinical trial of patients with myocardial infarction and left ventricular dysfunction, heart failure, or both, for the VALIANT Investigators. Circulation. 2010;122:597-602.
44 Yap YG, Duong T, Bland M, et al. Potential demographic and baselines variables for risk stratification of high-risk post-myocardial infarction patients in the era of implantable cardioverter-defibrillator—a prognostic indicator. Int J Cardiol. 2008;126:101-107.
45 Moss AJ, DeCamilla J, Mietlowski W, et al. Prognostic grading and significance of ventricular premature beats after recovery from myocardial infarction. Circulation. 1975;52(6 Suppl):III204-II210.
46 Bigger JTJr, Fleiss JL, Kleiger R, et al. The relationships among ventricular arrhythmias, left ventricular dysfunction, and mortality in the 2 years after myocardial infarction. Circulation. 1984;69:250-258.
47 Maggioni AP, Zuanetti G, Franzosi MG, et al. Prevalence and prognostic significance of ventricular arrhythmias after acute myocardial infarction in the fibrinolytic era. GISSI-2 results. Circulation. 1993;87:312-322.
48 Makikallio TH, Barthel P, Schneider R, et al. Prediction of sudden cardiac death after acute myocardial infarction: Role of Holter monitoring in the modern treatment era. Eur Heart J. 2005;26:762-769.
49 Epstein AE, Hallstrom AP, Rogers WJ, et al. Mortality following ventricular arrhythmia suppression by encainide, flecainide, and moricizine after myocardial infarction. The original design concept of the Cardiac Arrhythmia Suppression Trial (CAST). JAMA. 1993;270:2451-2455.
50 Bauer A, Watanabe MA, Barthel P, et al. QRS duration and late mortality in unselected post-infarction patients of the revascularization era. Eur Heart J. 2006;27:427-433.
51 Buxton AE, Sweeney MO, Wathen MS, et al. QRS duration does not predict occurrence of ventricular tachyarrhythmias in patients with implanted cardioverter-defibrillators. J Am Coll Cardiol. 2005;46:310-316.
52 Dhar R, Alsheikh-Ali AA, Estes NA3d, et al. Association of prolonged QRS duration with ventricular tachyarrhythmias and sudden cardiac death in the Multicenter Automatic Defibrillator Implantation Trial II (MADIT-II). Heart Rhythm. 2008;5:807-813.
53 Kuchar DL, Thorburn CW, Sammel NL. Late potentials detected after myocardial infarction: natural history and prognostic significance. Circulation. 1986;74:1280.
54 Steinberg JS, Regan A, Sciacca RR, et al. Predicting arrhythmic events after acute myocardial infarction using the signal-averaged electrocardiogram. Am J Cardiol. 1992;69:13-21.
55 Gomes JA, Caine MME, Buxton AE. Prediction of long-term outcomes by signal-averaged electrocardiography in patients with unsustained ventricular tachycardia, coronary artery disease, and left ventricular dysfunction. Circulation. 2001;104:436-441.
56 Bauer A, Guzik P, Barthel P, et al. Reduced prognostic power of ventricular late potentials in post-infarction patients of the reperfusion era. Eur Heart J. 2005;26:755-761.
57 Ikeda T, Sakata T, Takami M, et al. Combined assessment of T-wave alternans and late potentials used to predict arrhythmic events after myocardial infarction. A prospective study. J Am Coll Cardiol. 2000;35:722-730.
58 Gold MR, Bloomfield DM, Anderson KP, et al. A comparison of T-wave alternans, signal averaged electrocardiography and programmed ventricular stimulation for arrhythmia risk stratification. J Am Coll Cardiol. 2000;36:2247-2253.
59 Chevalier P, Burri H, Adeleine P, et al. QT dynamicity and sudden death after myocardial infarction: Results of long term follow up study. J Cardiovasc Electrophysiol. 2002;14:227-233.
60 Homs E, Martí V, Offndo J, et al. Automatic measurement of corrected QT interval in Holter recordings: Comparison of its dynamic behavior in patients after myocardial infarction with and without life-threatening arrhythmias. Am Heart J. 1997;134(2 Pt 1):181-187.
61 Haigney MC, Zareba W, Gentlesk PJ, et al. QT interval variability and spontaneous ventricular tachycardia or fibrillation in the Multicenter Automatic Defibrillator Implantation Trial (MADIT) II patients, for the Multicenter Automatic Defibrillator Implantation Trial II investigators. J Am Coll Cardiol. 2004;44:1481-1487.
62 Pham Q, Quan KJ, Rosenbaum DS. T-wave alternans: Marker, mechanism, and methodology for predicting sudden cardiac death. J Electrocardiol. 2003;36(Suppl):75-81.
63 Bloomfield DM, Steinman RC, Namerow PB, et al. Microvolt T-wave alternans distinguishes between patients likely and patients not likely to benefit from implanted cardiac defibrillator therapy. Circulation. 2004;110:1885-1889.
64 Chow T, Kereiakes DJ, Onufer J, et al. Does microvolt T-wave alternans testing predict ventricular tachyarrhythmias in patients with ischemic cardiomyopathy and prophylactic defibrillators? The MASTER (Microvolt T Wave Alternans Testing for Risk Stratification of Post-Myocardial Infarction Patients) trial, for the MASTER Trial Investigators. J Am Coll Cardiol. 2008;52:1607-1615.
65 Costantini O, Hohnloser SH, Kirk MM, et al. The ABCD (Alternans Before Cardioverter Defibrillator) Trial: Strategies using T-wave alternans to improve efficiency of sudden cardiac death prevention, for the ABCD Trial Investigators. J Am Coll Cardiol. 2009;53:471-479.
66 Verrier RL, Nearing BD. Ambulatory ECG monitoring of T-wave alternans for arrhythmia risk assessment. J Electrocardiol. 2003;36(Suppl):193-197.
67 Verrier RL, Kumar K, Nearing BD. Basis for sudden cardiac death prediction by T-wave alternans from an integrative physiology perspective. Heart Rhythm. 2009;6:416-422.
68 Verrier RL, Nearing BD, La Rovere MT, et al. Ambulatory electrocardiogram-based tracking of T wave alternans in postmyocardial infarction patients to assess risk of cardiac arrest or arrhythmic death, for the ATRAMI Investigators. J Cardiovasc Electrophysiol. 2003;14:705-711.
69 Minkkinen M, Kähönen M, Viik J, et al. Enhanced predictive power of quantitative TWA during routine exercise testing in the Finnish Cardiovascular Study. J Cardiovasc Electrophysiol. 2009;20:408-415.
70 Stein PK, Sanghavi D, Domitrovich PP, et al. Ambulatory ECG-based T-wave alternans predicts sudden cardiac death in high-risk post-MI patients with left ventricular dysfunction in the EPHESUS study. J Cardiovasc Electrophysiol. 2008;19:1037-1042.
71 Exner DV, Kavanagh KM, Slawnych MP, et al. Noninvasive risk assessment early after a myocardial infarction the REFINE study. J Am Coll Cardiol. 2007;50:2275-2284.
72 Kleiger RE, Miller JP, Bigger JT, Moss AJ, for the Multicenter Post-Infarction Research Group. Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. Am J Cardiol. 1987;59:256-262.
73 La Rovere MT, Bigger JTJr, Marcus FI, et al. Baroreflex sensitivity and heart rate variability in prediction of total cardiac mortality after myocardial infarction, for the ATRAMI investigators. Lancet. 1998;351:478-484.
74 Bigger JTJr, Fleiss JL, Steinman RC, et al. Frequency domain measures of heart period variability and mortality after myocardial infarction. Circulation. 1992;85:164-171.
75 Huikuri HV, Makikallio TH, Peng CK, et al. Fractal correlation properties of RR interval dynamics and mortality in patients with depressed left ventricular function after an acute myocardial infarction, for the DIAMOND study group. Circulation. 2000;101:47.
76 Bauer A, Barthel P, Muller A, et al. Risk prediction by heart rate turbulence and deceleration capacity in postinfarction patients with preserved left ventricular function retrospective analysis of 4 independent trials. J Electrocardiol. 2009;42:597-601.
77 Barthel P, Schneider R, Bauer A, et al. Risk stratification after acute myocardial infarction by heart rate turbulence. Circulation. 2003;108:1221-1226.
78 Bauer A, Barthel P, Schneider R, et al. Improved stratification of autonomic regulation for risk prediction in post-infarction patients with preserved left ventricular function (ISAR-Risk). Eur Heart J. 2009;30:576-583.
79 Okutucu S, Oto A. Risk stratification in nonischemic dilated cardiomyopathy: Current perspectives. Cardiol J. 2010;17:219-229.
80 Grimm W, Christ M, Sharkova J, Maisch B. Arrhythmia risk prediction in idiopathic dilated cardiomyopathy based on heart rate variability and baroreflex sensitivity. Pacing Clin Electrophysiol. 2005;28(Suppl 1):S202-S206.
81 Rashba EJ, Estes NA, Wang P, et al. Preserved heart rate variability identifies low-risk patients with nonischemic dilated cardiomyopathy: Results from the DEFINITE trial. Heart Rhythm. 2006;3:281-286.
82 Iacoviello M, Forleo C, Guida P, et al. Ventricular repolarization dynamicity provides independent prognostic information toward major arrhythmic events in patients with idiopathic dilated cardiomyopathy. J Am Coll Cardiol. 2007;50:225-231.
83 Hohnloser SH, Klingenheben T, Bloomfield D, et al. Usefulness of microvolt T-wave alternans for prediction of ventricular tachyarrhythmic events in patients with dilated cardiomyopathy: Results from a prospective observational study. J Am Coll Cardiol. 2003;41:2220-2224.
84 Salerno-Uriarte JA, De Ferrari GM, Klersy C, et al. Prognostic value of T-wave alternans in patients with heart failure due to nonischemic cardiomyopathy: Results of the ALPHA Study, for the ALPHA Study Group Investigators. J Am Coll Cardiol. 2007;50:1896-1904.
85 Gold MR, Ip JH, Costantini O, et al. Role of microvolt T-wave alternans in assessment of arrhythmia vulnerability among patients with heart failure and systolic dysfunction: Primary results from the T-wave alternans. Sudden Cardiac Death in Heart Failure trial substudy. Circulation. 2008;118:2022-2028.
86 De Ferrari GM, Sanzo A. T-wave alternans in risk stratification of patients with nonischemic dilated cardiomyopathy: Can it help to better select candidates for ICD implantation? Heart Rhythm. 2009;6(3 Suppl):S29-S35.
87 Task Force for Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of European Society of CardiologyDickstein K, Cohen-Solal A, Filippatos G, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J. 2008;29:2388-2442.
88 Gradman A, Deedwania P, Cody R, et al. Predictors of total mortality and sudden death in mild-to moderate heart failure, for the Captopril-Digoxin Study Group. J Am Coll Cardiol. 1989;14:564-570.
89 Doval HC, Nul DR, Grancelli HO, et al. Nonsustained ventricular tachycardia in severe heart failure: Independent marker of increased mortality due to sudden death. GESICA-GEMA Investigators. Circulation. 1996;96:3198-3208.
90 Chen X, Shenasa M, Borggrefe M, et al. Role of programmed ventricular stimulation in patients with idiopathic dilated cardiomyopathy and documented sustained ventricular tachyarrhythmias: Inducibility and prognostic value in 102 patients. Eur Heart J. 1994;15:76-82.
91 Nolan J, Flapan AD, Capewell S, et al. Decreased cardiac parasympathetic activity in chronic heart failure and its relation to left ventricular function. Br Heart J. 1992;69:761-767.
92 Nolan J, Batin PD, Andrews R, et al. Prospective study of heart rate variability and mortality in chronic heart failure: Results of the United Kingdom heart failure evaluation and assessment of risk trial (UK-Heart). Circulation. 1998;98:1510-1516.
93 La Rovere MT, Pinna GD, Maestri R, et al. Short-term heart rate variability strongly predicts sudden death in chronic heart failure. Circulation. 2003;107:565-570.
94 Hadase M, Azuma A, Zen K, et al. Very low frequency power of heart rate variability is a powerful predictor of clinical prognosis in patients with congestive heart failure. Circ J. 2004;68:343-347.
95 Guzetti S, La Rovere MT, Pinna GD, et al. Different spectral components of 24h heart rate variability are related to different modes of death in congestive heart failure. Eur Heart J. 2005;26:357i-362i.
96 Grimm W, Schmidt G, Maisch B, et al. Prognostic significance of heart rate turbulence following ventricular premature beats in patients with idiopathic dilated cardiomyopathy. J Cardiovasc Electrophysiol. 2003;14:819-824.
97 Moore RK, Groves DG, Barlow PE, et al. Heart rate turbulence and death due to cardiac decompensation in patients with chronic heart failure. Eur J Heart Fail. 2006;8:585-590.
98 Cygankiewicz I, Zareba W, Vazquez R, et al. Heart rate turbulence predicts all-cause mortality and sudden death in congestive heart failure patients, for the Muerte Subita en Insuficiencia Cardiaca Investigators. Heart Rhythm. 2008;5:1095-1102.
99 Fitzgibbons TP, Meyer TE, Aurigemma GP. Mortality in diastolic heart failure: An update. Cardiol Rev. 2009;17:51-55.
100 Hsia J, Jablonski K, Rice MM, et al. Sudden cardiac death in patients with stable coronary artery disease and preserved left ventricular systolic function. Am J Cardiol. 2008;101:457-461.
101 Klingenheben T, Hohnloser SH. Usefulness of risk stratification for future cardiac events in infarct survivors with severely depressed versus near-normal left ventricular function: Results from a prospective long-term follow-up study. Ann Noninvasive Electrocardiol. 2003;8:68-74.
102 Ikeda T, Yoshino H, Sugi K, et al. Predictive value of microvolt T wave alternans for sudden cardiac death in patients with preserved cardiac function alter acute myocardial infarction: Results of a collaborative cohort study. J Am Coll Cardiol. 2006;48:2268-2274.
103 Nieminen T, Lehtimaki T, Viik J, et al. T-wave alternans predicts mortality in a population undergoing a clinically indicated exercise test. Eur Heart J. 2007;28:2332-2337.
104 Cygankiewicz I, Zareba W, Vazquez R, et al. Risk stratification of mortality in patients with heart failure and left ventricular ejection fraction >35, for the MUSIC Investigators. Am J Cardiol. 2009;103:1003-1010.
105 Watanabe J, Shinozaki T, Shiba N, et al. Accumulation of risk markers predicts the incidence of sudden death inpatients with chronic heart failure. Eur J Heart Fail. 2006;8:237-242.
106 Bauer A, Zurn CS, Schmidt G. Heart rate turbulence to guide treatment for prevention of sudden death. J Cardiovasc Pharmacol. 2010;55:531-538.