Chapter 15 Risk Factors for Anterior Cruciate Ligament Injuries in the Female Athlete
INTRODUCTION
The higher incidence of noncontact anterior cruciate ligament (ACL) injuries in female athletes than in male athletes participating in the same sport has received a significant amount of attention in the orthopaedic literature since the early 1990s. A study from the authors’ institution published in 199463 was one of the first to report this problem, because female soccer players were found to have nearly six times the rate of serious knee ligament injuries than that of male players (0.87 and 0.29/100 player-hr, respectively; P < .01). The following year, Arendt and Dick6 presented data from the National Collegiate Athletic Association (NCAA) of injuries sustained by soccer and basketball players over a 5-year period. The ACL injury rate in females was more than double that of males in soccer (0.31 and 0.13/1000 exposures, respectively; P < .05) and four times that of males in basketball (0.29 and 0.07/1000 exposures; respectively, P < .05). Messina and coworkers70 reported that female high school basketball players had nearly four times the incidence of ACL injuries than male players (0.091 and 0.024/1000 player-hr, respectively; P < .05). Gwinn and associates43 evaluated the incidence of ACL injuries in midshipmen at the U.S. Naval Academy over a 6-year period. These authors reported that women had a fourfold increase in this injury compared with men in intercollegiate soccer, basketball, and rugby collectively (0.511 and 0.129/1000 athlete-exposures, respectively; P = .006). During military training, women had nearly 11 times the incidence of ACL ruptures as men during obstacle course running (6.154 and 0.567/1000 athlete-exposures, respectively; P = .004). Agel and colleagues1 reviewed 13 years of NCAA injury data and reported a continued gender disparity in ACL injury rates between collegiate female and male basketball and soccer players.
Despite the multitude of investigations that have been conducted on potential risk factors for noncontact ACL ruptures, definitive conclusions cannot currently be reached for either males or females regarding what factor(s) may predispose an athlete to this injury. In addition, the reasons for the increased incidence of this injury in female athletes over that in male athletes cannot be scientifically defined at present. The problems are that the majority of studies published to date have either examined a very small sample size of each gender (therefore containing insufficient power to avoid a type II statistical error40), focused on only one possible risk category, or examined neuromuscular characteristics in a controlled laboratory environment instead of actual playing conditions. The potential risk factors that have been proposed for this injury are shown in Table 15-1. This chapter reviews investigations related to these risk factors and emphasizes findings that may have a role in the gender disparity in noncontact ACL injury rates. Opinions expressed by scientists and researchers from the 2005 Hunt Valley II Meeting (sponsored by the American Orthopaedic Society for Sports Medicine [AOSSM])41 regarding this problem are also provided in each major risk factor section as well as consensus statements generated from this meeting.
TABLE 15-1 Hypothesized Major Risk Factors for Anterior Cruciate Ligament Injury
| Gender | Category | Risk Factor |
|---|---|---|
| Males and females | Familial | Genetics, possibly related to anatomic structures (size intercondylar notch) |
| Males and females | Environmental |
ACL, anterior cruciate ligament.
GENETIC PREDISPOSITION
Although the question has been raised for many years of a potential genetic predisposition for ACL rupture, only two studies have been published regarding this risk factor. Harner and coworkers44 investigated familial and anatomic risk factors in a small series of 31 patients who had sustained noncontact bilateral ACL ruptures. Compared with a control group matched for age, sex, height, weight, and activity level, the patients demonstrated a significant difference in the incident rate of immediate family members who had sustained an ACL injury (35% and 4%, respectively; P < .01) and a significantly wider lateral femoral condyle (3.30 and 3.10 cm, respectively; P < .05). The authors concluded that there could have been a congenital predisposition to ACL injury that theoretically resulted from anatomic differences in the size of the femoral condyles.
Flynn and associates34 conducted a questionnaire-based study of 171 patients who sustained either contact or noncontact ACL ruptures to determine whether a familial predisposition existed for this injury. The patients were matched with 171 uninjured control subjects according to age, gender, and primary sport. The data were not sorted according to mechanism of ACL rupture (contact vs. noncontact). The survey results revealed that patients who had sustained ACL ruptures were twice as likely to have a first-, second-, or third-degree relative who also had an ACL tear than the control subjects. Limitations of the study include those associated with recall of injury by the patients of their relatives’ medical history and no medical documentation of the relatives’ ACL ruptures.
ENVIRONMENTAL
Climate Conditions
Few studies have been conducted to determine the effect of climate conditions, such as rainfall, heat, and humidity, on noncontact ACL injuries. In addition, no investigation to date has taken into account other risk factors (such as hormonal or neuromuscular) along with climate conditions that could confound possible conclusions. Orchard and colleagues82 examined intrinsic (height, weight, age, body mass index (BMI), history of prior ACL injury) and environmental-related variables as risk factors for noncontact ACL injuries in male Australian football players. The incidence of noncontact ACL injuries in the 1643 players was 0.62 per 1000 athlete-exposures. The most significant risk factors were a history of a prior ACL injury and weather conditions (high evaporation and low rainfall) that resulted in a dry playing surface. The theories that high shoe-surface traction was a risk factor for noncontact ACL injury and that dry playing conditions increased friction and torsional resistance between shoes and natural grass were advanced by the authors. Of note was the higher incidence of all ACL injuries in this group (0.82/1000 athlete-exposures) compared with previously published data of American football players (0.25/100 athlete-exposures93) and American collegiate soccer male players (0.12/1000 athlete- exposures7). The authors attributed this difference to the prevailing climatic conditions in Australia, which commonly produced dry, hard ground conditions.
Playing Surface
Meyers and Barnhill71 tracked male high school football injuries sustained in eight schools over 5 seasons. The rate of ACL injuries was nearly 50% higher on natural grass than on artificial turf (FieldTurf); however, a total of only 15 ACL ruptures were sustained in the 240 games surveyed. Olsen and coworkers81 examined ACL injury rates in both men and women team handball players to determine whether an association existed between injury rates and two types of floor surfaces. Over a period of seven seasons (94,136 player-hr), the ACL injury rates were 0.24 per 1000 player-hours for men and 0.77 per 1000 player-hours for women (P = .001). The ACL injury rate for women was higher on artificial floors than that of women playing on wooden floors (0.96 and 0.41/1000 player-hr, respectively; P = .03). There was no difference in the ACL injury rate between floor surface types in the male players and there was no difference between genders in ACL injury rates on wooden floors. Unfortunately, the investigators had to eliminate two thirds of all ACL injuries that were incurred in the study group owing to unreliable floor-type exposure data.
Critical Points ENVIRONMENTAL RISK FACTORS
ACL injury rate for women was higher on artificial floors than on wooden floors in one study.
Effect of footwear on ACL injury rates has not yet been studied in women.
AOSSM Consensus: Shoe-surface interaction may affect ACL injury risk both directly and indirectly.
Footwear
Lambson and associates58 evaluated the effect of football cleat design on ACL injury rates (contact and noncontact) in 3119 high school football players who were followed for 3 seasons. A total of 42 ACL ruptures were recorded in this study. Shoes with long, irregular cleat designs produced significantly higher torsional resistance (P < .05) on both artificial and natural playing surfaces than the other cleat designs studied and were also associated with a significantly higher rate of ACL injuries (P = .0062). Whereas the authors recognized that many potential risk factors were not analyzed, they recommended that the long, irregular cleat design be discontinued in high school football players. The effect of footwear on ACL injuries in female athletes has not been investigated to date.
Prophylactic Knee Braces
No study to date has demonstrated that knee braces significantly reduce the incidence of ACL injuries in normal healthy athletes.76 Only two epidemiologic investigations were published in the 1990s on this topic, both of which followed only male football players. Sitler and colleagues102 conducted an investigation involving 1396 U.S. Military Academy cadets who played intramural tackle football and in whom the type of shoe, athlete exposure, brace compliance, playing surface, and knee injury history were controlled. The brace was a double-hinged, single, upright, off-the-shelf design (DonJoy, Inc., Carlsbad, CA) that was randomly assigned to players at the beginning of each of the 2 seasons surveyed. A statistically greater number of medial collateral ligament (MCL) injuries occurred in the control group than in the braced group (P < .05). Although a higher number of ACL injuries was found in the control group than in the braced group (12 vs. 4), the small number precluded statistical analysis. The second epidemiologic investigation published in this time period assessed only MCL injury patterns.2
AOSSM Consensus and Opinion
The Hunt Valley II Meeting participants concluded that data reported to date regarding environmental risk factors for ACL noncontact injuries has been “confusing and mixed.”41 The researchers did conclude that shoe-surface interaction may affect ACL injury risk both directly and indirectly.41 The direct effect is through higher traction, which may transmit excessive load forces to the knee during cutting and pivoting. The indirect effect is through alterations in neuromuscular movement patterns in an attempt to adapt to variations in shoe and surface factors. Future studies examining the potential impact of these factors should include both intrinsic and extrinsic variables and use sound epidemiologic study design.
ANATOMIC
Intercondylar Notch and ACL Size
An association between a small-sized intercondylar notch and an increased incidence of ACL ruptures has been reported or suggested by some authors,5,36,50,59,67,97,105 but refuted by others.47,65,92,108 The association, which remains debatable, has been reported by some investigators to be present in both genders.41,54,97 A general speculation has been raised by some authors41 that a small-sized notch will contain a small-sized ACL that is vulnerable to rupture owing to decreased strength properties. Variations in techniques used to determine notch size (plain non–weight-bearing and weight-bearing radiographs, magnetic resonance imaging [MRI], computed tomography [CT], photographic techniques), problems and lack of standardization with these techniques (such as uncontrolled knee flexion angles and rotation on radiographs), discrepancies in notch indices studied (lateral condylar width, total condylar width, notch width, notch width at two thirds notch height, notch width index, notch angle), and differences in statistical methods used to ascertain measurements account for the disagreement among studies. The major problem is that no study to date has entered anatomic indices along with hormonal and neuromuscular factors into an appropriate statistical model to determine the effects of all of these potentially important risk factors.
Critical Points ANATOMIC RISK FACTORS
Size of the ACL cannot be reliably predicted from the size of the intercondylar notch.
Uhorchak and coworkers,109 in the most comprehensive ACL risk factor study published to date, measured height, weight, BMI, condylar width, notch width, eminence width, tibial width, notch width index, generalized joint laxity, anteroposterior (AP) displacement on KT-2000 testing, isokinetic quadriceps and hamstrings concentric and eccentric strength, and hamstrings flexibility in a group of 895 West Point cadets (120 women, 739 men) upon their entrance into the academy. The cadets were followed for 4 years for ACL injuries, during which time 24 noncontact ACL ruptures occurred (16 in men, 8 in women). Using a hypothesis-driven logistic regression model, the factors of a narrow femoral notch, BMI 1 standard deviation (SD) or more above the mean, and generalized joint laxity explained 62.5% of the variability of the noncontact ACL tears in the female athletes. In addition, this model correctly predicted 75% (6 of 8) of the noncontact ACL injuries. The most predictive model in the men explained only 15% of the variability in the noncontact ACL injuries and was unable to predict any of the 16 injuries that occurred throughout the study period in the male athletes.
The shape of the intercondylar notch varies,53 but this does not appear to be useful in predicting patients who may have an increased risk for ACL injury.5,54,106 In addition, the size of the ACL cannot be reliably predicted from the size of the intercondylar notch.4,75,106 A few investigators have attempted to determine whether a gender difference exists in the cross-sectional area, mass, and volume of the ACL in uninjured subjects using MRI4,18,23,106 and in cadaveric specimens.14,75 Charlton and associates18 reported that, although a difference existed between uninjured men and women in the volume of the femoral notch and ACL, this difference was related to height and weight and not gender. Patients with smaller notches also had smaller ACLs. Anderson and colleagues4 found no difference between male and female high school basketball players in the notch width index or in the size of the ACL when normalized for lean body weight (body weight x [100 – % body fat]). When adjusted for body weight, the mean ACL area was significantly greater in the male players (P < .003). There was a correlation of ACL area to height in the male players (P = .03) but not in the female players. Taller male players had large ACLs, but taller female players had ACLs of a size similar to that of shorter female players. The authors concluded from their data that the cause of ACL rupture in patients with narrow notches was not due to a smaller (more vulnerable) ligament, but to a normal-sized ACL in a stenotic notch. This finding supported that previously described by Muneta and coworkers75 who, in a cadaveric study, found no correlation between the size of the intercondylar notch and that of the ACL.
Staeubli and associates106 measured the widths of the cruciate ligaments and intercondylar notches in 51 uninjured subjects with MRI. The notch measurements were performed in three areas in the coronal plane: at the notch entrance, at the intersection of the cruciate ligaments, and at the notch outlet. The authors reported a significant difference between genders in the absolute width of the ACL at the cruciate intersection (men, 6.1 ± 1.1 mm, and women, 5.2 ± 1.0 mm; P < .01). The intercondylar notch widths were also significantly greater in males, as were height, weight, and bicondylar femoral width. The ACL and notch size measurements were not normalized for these variables. The ACL occupied only 31.9% of the notch in men and 31.1% of the notch in women, refuting the belief that the size and shape of the notch lead to an increased risk of ACL injury.
Chandrashekar and colleagues14 studied the length, area, mass, and volume of the ACL in 20 cadaveric knees (10 males, 10 females, aged 17–50 yr) using a photographic three-dimensional scanning system. The male specimens had significantly larger values than the females for ACL length (29.82 mm ± 2.51 and 26.85 ± 2.82 mm, respectively; P = .01), mid-substance area (83.54 ± 24.89 mm2 and 58.29 ± 15.32 mm2, respectively; P = .007), mass (2.04 ± 0.26 g and 1.58 ± 0.42 g, respectively; P = .009), and volume (2967 ± 886 mm3 and 1954 ± 516 mm3, respectively; P = .003). There were no significant differences between genders in ACL mass density, notch width, or notch width index. ACL cross-sectional area and volume were not associated with body height or lean body mass in either gender. ACL mass strongly correlated with height in men (R = 0.7; P < .02), but not in women (R = 0.43; P ≥ .02). The authors concluded that because the density of the ACL is similar between genders, the smaller ligament size in women may contribute to their increased rate of noncontact ACL rupture.
Foot Pronation
Excessive foot pronation has been suggested as a potential risk factor for ACL injuries.3,9,66,115 Some authors have speculated that excessive subtalar joint pronation leads to increased internal tibial rotation and resultant high forces on the ACL. Two investigations involving small sample sizes reported significantly higher navicular drop values bilaterally in patients who sustained ACL ruptures compared with matched control subjects.3,9 Allen and Glasoe3 measured navicular drop in 18 subjects who had sustained ACL ruptures using a Metrecom three-dimensional digitizer. When compared with an age- and gender-matched control group, the mean values of the navicular drop of both the ACL-ruptured and the contralateral limbs of the patients were significantly larger than those in the control group (P < .05) by approximately 2 mm. No other risk factors were included in this investigation. Woodford-Rogers and coworkers115 measured navicular drop, calcaneal alignment, and anterior tibial translation in the uninjured limb of 22 high school and collegiate athletes (14 males, 8 females) who had sustained noncontact ACL injuries. The data were compared with those of athletes matched by sport, team, position, and level of competition. The authors reported that the ACL-injured athletes had greater amounts of navicular drop of approximately 2.5 mm in the male subjects and 2 mm in the female subjects. Discriminant analysis of the data showed that navicular drop, calcaneal alignment, and anterior tibial translation (when combined) were predictors of classification of athletes into the ACL-injured and the ACL-noninjured groups, because 87.5% of the athletes were correctly classified (chi-square, 9.00; P < .01). Both of these studies suggested that excessive pronation may lead to an increased risk of ACL rupture.
A combination of postural “faults” was found to have a greater predictive value for ACL injury than a single problem (such as excessive pronation) by Loudon and associates.66 In 20 female athletes with unilateral ACL ruptures, the combination of excessive knee hyperextension, navicular drop, and subtalar joint pronation was a strong discriminator between the patients and 20 control subjects. The authors concluded that an association existed between noncontact ACL injuries in females who had a standing posture of genu recurvatum and subtalar joint overpronation.
Smith and colleagues104 failed to find an association between excessive pronation and noncontact ACL injuries. The authors used a combination of navicular drop and calcaneal stance measures in 14 patients with ACL ruptures and compared the data with those of 14 control subjects matched for age, height, and weight. There was no significant difference in the navicular drop test between the patients and the controls. The authors cautioned that static measurements of pronation may not be representative of dynamic conditions and that future research should include not only dynamic analyses but other anatomic risk factors as well.
BMI
There is no evidence to support that an excessive BMI alone is a risk factor for noncontact ACL injuries. Ostenberg and Roos83 found that BMI was not a risk factor for knee injuries in female soccer players, as did Knapik and coworkers56 in military training–related injuries in female recruits. When combined with a narrow femoral notch and generalized joint laxity, a BMI greater than 1 SD above the mean did contribute to a high prediction of noncontact ACL injuries in Uhorchak and coworkers’ series.109
Generalized Ligament Laxity
Some authors have reported that females appear to have greater inherent joint laxity than males.12,60,88–90 Huston and Wojtys52 reported that females had significantly greater anterior tibial translation than males (6.5 and 5.8 mm, respectively; P < .05), as did Rozzi and associates90 (6.05 ± 1.46 mm and 4.80 ± 1.53 mm, respectively; P = .02). Seckin and colleagues94 reported a significantly greater prevalence of generalized joint hypermobility in female high school students than in male students (16.2% and 7.2%, respectively; P < .0001). Remvig and coworkers88 found considerable evidence in the literature of an increased prevalence of hypermobility among women. However, there is no evidence that an increase in generalized ligament laxity in females is associated with the increased rate of noncontact ACL injuries.
AOSSM Consensus and Opinion
The Hunt Valley II Meeting participants concluded that “there is no definite evidence that any anatomical factor is reliably associated across age groups and sexes with an increased rate of injury” based on the amount of conflicting published data and variety of study designs.41
HORMONAL
Sex Hormones in Human ACLs
Since the early 2000s, the hypothesis that fluctuations in sex hormones during certain periods of the menstrual cycle could be deleterious to the material and mechanical properties of the female ACL has been raised by several investigators. Some postulated that these harmful effects could explain the heightened risk of ACL ruptures in female athletes,53 although a recent investigation on a synomolgus monkey model showed no direct effects of estrogen on ACL mechanical or material properties.110 Estrogen and progesterone have been shown to significantly alter the structure and metabolism of collagen in human and animal models.98 Other authors have raised the question of whether hormonal surges could have a deleterious effect on muscle and neuromuscular indices, thereby increasing the vulnerability of the ACL to rupture during certain phases of the menstrual cycle.13
Critical Points HORMONAL RISK FACTORS
Questions Raised
Estrogen and progesterone target cells are present within the human ACL.
In 1996, Liu and associates64 conducted the first investigation to determine whether estrogen and progesterone target cells were located within the human ACL. Seventeen ACL specimens were obtained from patients undergoing a variety of surgical procedures, 13 from women and 4 from men. Both hormone receptors were found in the ACL fibroblasts, which led the authors to suggest that female sex hormones may have an effect on the ligament’s structure and composition.
A few years later, Yu and colleagues117 conducted an analysis of the effects of estrogen on human ACL fibroblast proliferation and procollagen synthesis. An ACL sample was obtained from a 32-year-old female patient undergoing a total knee replacement. A dose-dependent effect of estrogen was demonstrated, because the proliferation of ACL fibroblasts decreased as estrogen concentration was increased. This effect was most striking in the early periods of hormone exposure (days 1 and 3 after administration) and became less pronounced with time. In addition, a dose-dependent effect was found with type I procollagen synthesis, which decreased with increased estrogen concentration. Type I collagen is associated with mechanical strength of connective tissues.
In a second investigation, Yu and coworkers118 studied the effects of varying levels of estrogen and progesterone on human ACL fibroblast proliferation and procollagen synthesis. Cell lines were obtained from ligaments in two young female patients. The authors reported that estrogen had a dominant inhibitory effect on human ACL fibroblast proliferation and type I procollagen synthesis and that progesterone reduced this effect. A dose-dependent increase in ACL fibroblast proliferation and type I procollagen synthesis occurred when progesterone concentration was increased and estrogen concentration held constant. The dose-dependent effects of progesterone were more pronounced at lower levels of estrogen concentration than at higher levels. The authors concluded from these investigations that the acute hormonal fluctuations that occur during the menstrual cycle may induce changes in the metabolism of the ACL, weakening the ligament’s strength and increasing its vulnerability to injury.
Faryniarz and associates31 measured estrogen and relaxin receptors from resected ACL specimens in eight women and seven men an average of approximately 5 weeks after their injury. Whereas there was no significant difference between genders in the concentration of estrogen receptors in ACL cells, women had higher levels of relaxin-binding sites. The authors concluded that estrogen alone may not play a role in the gender disparity in noncontact ACL injury rates. However, their data were considered preliminary and the authors remarked that subtle differences between genders in estrogen concentration in human ACLs may be detected in a study with a larger sample size.
Influence of Sex Hormones on AP Tibial Translation
Several investigators have measured fluctuations in AP tibial displacement measured with a KT-2000 throughout the menstrual cycle.12,27,45,98,99 Heitz and colleagues45 followed seven active women aged 21 to 32 years with serial radioimmunoassay procedures to determine levels of estrogen and progesterone throughout a 28- to 30-day menstrual cycle. The subjects’ hormone levels and AP tibial displacement were measured on days 1, 10, 11, 12, 13, 20, 21, 22, and 23 of the menstrual cycle. Day 1 corresponded to the ovulatory phase; days 10 to 13, to the follicular phase (peak estrogen surge); and days 20 to 23, to the luteal phase (peak progesterone surge). Statistically significant increases in AP displacement (at 134 N) were reported between day 1 and the follicular phase (5.6 ± 1.34 mm and 6.4 ± 1.64 mm, respectively; P < .05) and between day 1 and the luteal phase (5.6 ± 1.34 mm and 7.0 ± 1.66 mm, respectively; P = .006).
Deie and coworkers27 followed 16 women aged 21 to 23 years with serial measurements of AP displacement, basal body temperature, and serum levels of estrogen and progesterone obtained two to three times per week over 4 consecutive weeks. The authors reported statistically significant increases in AP displacement between the follicular and the ovulatory phases (4.7 ± 0.8 mm and 5.3 ± 0.7 mm, respectively; P < .05) and between the follicular and the luteal phases (4.7 ± 0.8 mm and 5.2 ± 0.7 mm, respectively; P < .05). However, the differences in AP displacement are relatively small and of questionable clinical significance.
Shultz and associates98 conducted a rigorous investigation on 22 women aged 18 to 30 years in which daily tests were conducted to determine levels of estrogen, progesterone, and testosterone, as well as anterior tibial displacement, over one complete menstrual cycle. The authors reported that interaction of all three hormones explained 63% of the variance in anterior tibial translation. However, considerable variability was reported between subjects regarding the contribution of each hormone separately and all three collectively and in the associated time delay in which the change in anterior tibial displacement was detected after a hormonal surge. In addition, not all subjects demonstrated an increase in anterior tibial displacement; whereas some women had 4- to 5-mm differences across the cycle, others had little to no change.
In a second study, Shultz and colleagues99 compared the anterior tibial translation values of 22 female subjects collected daily over the course of one complete menstrual cycle with those of 20 males who were tested once per week for 4 weeks. The women underwent daily tests to determine the levels of estrogen, progesterone, and testosterone. The female subjects had significantly greater anterior tibial translation than the male subjects (P < .05) over the study period. However, these measurements varied daily and appeared to occur on days in which estrogen and progesterone levels were significantly elevated (early luteal phase). The authors stressed that it remains unknown whether the differences in knee joint laxity between genders accounts for the increased risk of ACL injury in females.
Beynnon and coworkers12 compared AP tibial translation values between 17 healthy women aged 17 to 29 years collected at five time periods (early follicular, late follicular, midluteal, late luteal during one menstrual cycle, and early follicular of the next cycle) with measurements obtained from 17 male control subjects aged 18 to 31 years. The females had significantly greater AP values (P = .01) at each time period. There was no significant difference within the female subjects in AP translation over time.
Association between Phases of the Menstrual Cycle and ACL Ruptures
In three investigations, hormone levels were measured after ACL ruptures in a total of 144 female athletes to determine whether an association existed between the incidence of this injury and a phase of the cycle.13,103,112 Wojtys and associates112 measured estrogen, progesterone, and luteinizing hormone metabolites in the urine of 65 female athletes within 24 hours of their ACL injury and at the start of their next menstrual cycle. The luteinizing hormone, identifiable by serum or urine specimens, determines when ovulation occurs and allows accurate identification of the follicular and luteal phases. Fifty-one of the women did not use oral contraceptives; in these subjects, significantly more ACL ruptures occurred during the ovulatory phase than expected (>2.5 times), and fewer injuries occurred during the luteal phase than expected (Table 15-2). Fourteen women were taking oral contraceptives; in this subgroup, there was no significant association found between the phase of the cycle and the incidence of ACL rupture. However, the number of subjects taking oral contraceptives was too low to draw statistically relevant conclusions.
TABLE 15-2 Phase of the Menstrual Cycle in Which Anterior Cruciate Ligament Ruptures Occurred According to Oral Contraceptive Use
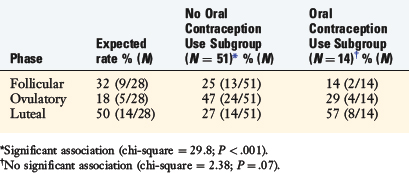
Slauterbeck and colleagues103 used questionnaires and saliva samples obtained within 72 hours of ACL ruptures in 38 female athletes to document cycle phase. Thirty-one of the women did not use oral contraceptives. There were a significantly greater number of ACL injuries during the follicular phase of the cycle than expected. Only 1 subject suffered an ACL rupture during the ovulatory phase.
Beynnon and coworkers13 measured serum concentrations of estrogen and progesterone in 42 female recreational alpine skiers within 2 hours of the ACL rupture. The subjects were matched with 46 controls. The investigators segregated the menstrual cycle into two phases, preovulatory and postovulatory, according to levels of progesterone measured. The data revealed that significantly more ACL ruptures occurred during the preovulatory phase than expected. After considering skier experience and ability, the female subjects were estimated to be three times more likely to tear their ACL during the preovulatory phase. The authors concluded that their data were similar to those reported by others,103,113 with an apparent association toward a greater proportion of female athletes suffering ACL ruptures in the preovulatory (follicular) phase than in later phases of the cycle. Whether this observation is due to deleterious effects of hormonal fluctuations on collagen metabolism or to changes in muscle contraction and neuromuscular control remains to be determined.
Influence of Hormone Fluctuations and Oral Contraceptives on Knee Kinematics
As of the time of writing, a study conducted at the authors’ laboratory19 was the only published to date that assessed whether hormonal cycling in women affected loading on the knee during high-risk tasks. Twenty-five women, 12 of whom were not taking oral contraceptives and 13 of whom were on oral contraceptives, and 12 males underwent neuromuscular testing. The female subjects completed the same tests six times over an 8-week period during which time serum concentrations of estrogen and progesterone were measured. Each subject was tested twice during the follicular, luteal, and ovulatory phases. The tests included a horizontal jump, a vertical jump, and a drop-jump from a 30-cm box onto a single leg. Hip and knee kinematics and peak externally applied moments were calculated. The male subjects underwent the same tests on one occasion. The results showed no significant difference between genders or between the two female subgroups in moments or knee flexion angles. The authors concluded that fluctuations in hormones throughout the menstrual cycle are not solely responsible for the gender disparity in noncontact ACL injury rates; rather, that the problem most likely is a result of a “complex interaction between ligament structural properties, fatigue, and neuromuscular control.”19
AOSSM Consensus and Opinion
Participants of the Hunt Valley II Meeting agreed that further well-controlled investigations are required to understand the implications of fluctuating or surging female hormones on ACL injury risk and knee function.41 Although there appears to be an uneven distribution of ACL injuries in the follicular phase of the menstrual cycle, more data are required before definitive conclusions may be reached. There was no consensus among panel members regarding the role of oral contraceptives on knee injury risk or function.
NEUROMUSCULAR/BIOMECHANICS
Several neuromuscular and biomechanical factors have been hypothesized by various investigators to be responsible for the disparity between genders in noncontact ACL injury rates (Table 15-3). Differences between female and male athletes in movement patterns; muscle strength, activation, and recruitment patterns; and knee joint stiffness have been demonstrated under controlled preplanned and reactive conditions in the laboratory. As well, videotape analyses of noncontact ACL injuries demonstrate certain lower extremity positions and characteristics that lend support to the theory that these differences may likely play a role in this problem.57,80
TABLE 15-3 Hypothesized Neuromuscular and Biomechanical Risk Factors for Noncontact Anterior Cruciate Ligament Injury in the Female Athlete
| Category | Risk Factor | Hypothesized Gender Difference |
|---|---|---|
| Movement patterns |
Biomechanical Function of the Hamstring Musculature
Many noncontact ACL ruptures occur when an athlete lands from a jump.33,35,39,55 Ground reaction forces measured during various jumping models have been reported to be 3 to 14 times body weight.29,72,73,79,100,101 When analyzed on videotape, noncontact ACL injuries frequently occur with a forceful valgus and tibial rotation motion with the knee close to full extension.80 The hamstring musculature is important in stabilizing the knee joint because it functions as a joint compressor and restrains anterior tibial translation.68,74 The biomechanical function of the pes anserinus (sartorius, gracilis, and semitendinosus muscles) was assessed many years ago in a study involving 15 fresh cadaver knees.77 The anatomic courses and insertions of the three muscles relative to the knee joint and tibia were recorded at standard positions of knee flexion. On 5 of these specimens, biplane radiographs were collected to determine the orientation and load lines of the muscles at 0°, 30°, 60°, and 90° of flexion. A gentle pull on the muscle belly was done to simulate muscle contractions. The spatial relations of the muscles and tendons that form the pes anserinus were recorded by placing fine wire markers under direct visualization into the superficial aspect of the midportion of each muscle belly and tendon. The wires extended from a proximal point on the thigh to the insertion in the tibia. The dissection was limited to a subcutaneous exposure in order not to disturb the structures under study.
Critical Points NEUROMUSCULAR/BIOMECHANICAL RISK FACTORS
High quadriceps activity can serve as a major intrinsic force in noncontact ACL injuries.
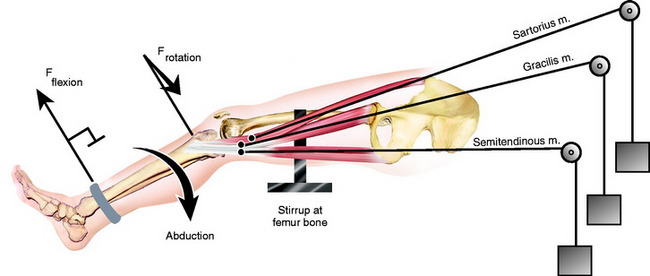
Mechanical tests of the forces produced on the knee joint under known loading conditions of the pes anserinus were performed on 8 unenbalmed extremities. The three muscles were loaded individually and then collectively with weights up to 7.72 kg, which provided easily measurable forces on the leg (Fig. 15-1). The flexion force produced was measured by a circular bearing attached to the distal aspect of the leg, which allowed the tibia to be rotated without significantly changing the knee joint’s axial center of rotation. Rotation was measured by two Steinmann pins that were inserted through the tibial tubercle in a transverse plane. A cord to measure rotation force (Frotation) was attached at right angles to one pin. This cord was loaded prior to testing, which allowed the limbs to be positioned in external tibial rotation up to 15°.
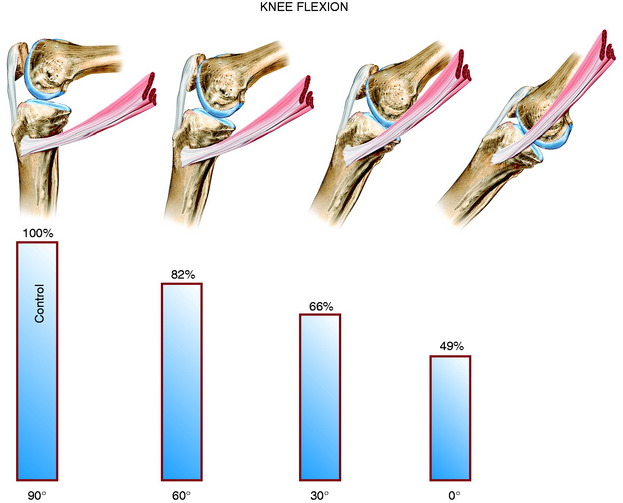
The flexion force of the pes anserinus was greatest at 90° of knee flexion (Fig. 15-2). As the knee was extended, the tendon insertion angle became more acute relative to the tibia, resulting in a decrease in the mechanical advantage of the muscle and a subsequent decrease in the flexion moment about the knee joint despite equal muscle loading conditions. The difference in the mean values of the flexion force at the four knee positions was statistically significant (P < .05).
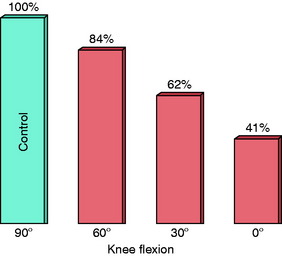
The rotation force of the pes anserinus was greatest at 90° of knee flexion (Fig. 15-3). The decrease in the angle of tendon insertion relative to the tibial with knee extension explains the decrease in rotation force in a manner similar to that noted for the flexion force. There was a statistically significant difference in the mean values of the rotation force at the four knee flexion positions (P < .05).
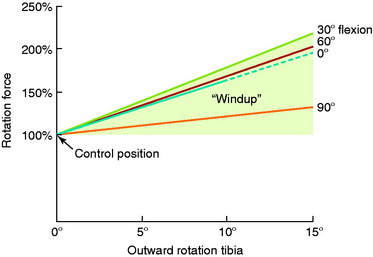
The rotation force of the pes anserinus under the same muscle load increased with increasing external tibial rotation at the four knee flexion positions (Fig. 15-4). The rotation force produced at 15° of external tibial rotation was approximately double that measured at 0° of external tibial rotation. The wind-up effect, although present at 90° of knee flexion, was smaller in magnitude than that measured at 30° of knee flexion. The difference in the mean rotation force values was significant at the four knee flexion positions (P < .05).
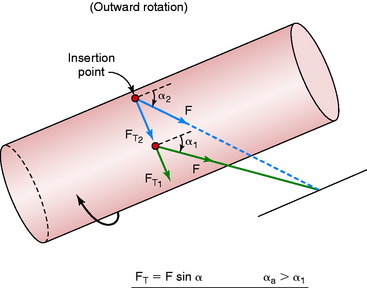
There was no significant change in the flexion force of the pes anserinus at the different positions of external tibial rotation. The wind-up effect is due in part to a change with external tibial rotation in the angle of muscle tendon insertion of the pes anserinus relative to the tibia (Fig. 15-5). The tibia may be viewed as a cylinder undergoing external rotation whereby the tendon insertion course angle increases from α1 to α2. The component of the force that produces the rotation effect (FT) is equal to (F sin α) and thus increases as the angle α increases.
These data indicate that the sartorius, gracilis, and semitendinosus muscles have a marked functional dependence on the angle of knee flexion and degrees of external tibial rotation. They actively oppose extension by stabilizing the knee posteriorly and preventing knee hyperextension and anterior subluxation of the tibia. In addition, these muscles actively oppose external tibial rotation. The mechanical advantage of the pes anserinus increases as the knee goes into further flexion. At 0° of extension, the flexion force is reduced to 49% of that measured at 90° of flexion. Other investigators have reported that a quadriceps-hamstrings co-contraction cannot reduce ACL strain from full extension to approximately 20° of flexion.78,85
Consequences of High Quadriceps Forces on the ACL
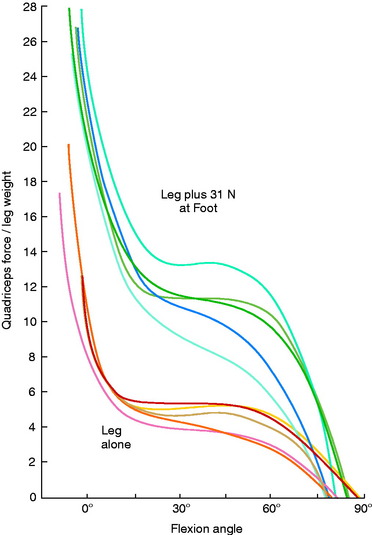
Grood and associates42 examined the knee extension exercise in cadavers to determine the conditions in which the ACL was loaded, the quadriceps force that developed during knee flexion-extension, and the forces that were incurred on the extensor mechanism as the knee was extended. An open kinetic chain knee extension exercise was simulated both without resistance and with 31 N (7 lb) of resistance provided by an ankle weight placed at the foot. The quadriceps force required to extend the knee remained at a constant value of 177 N between 50° and 15°, but then rose rapidly to reach 350 N at 0° (Fig. 15-6). The addition of resistance doubled the quadriceps force that was required to extend the knee, resulting in large muscle forces on the ACL and patellofemoral joint.
DeMorat and colleagues28 reported that a high quadriceps load (4500 N) simulated in cadaveric knees at 20° of flexion produced significant anterior tibial translation (mean, 19.5 mm). Whereas all 11 knees sustained damage to the ACL, not all suffered complete failure. The authors concluded that the quadriceps can serve as a major intrinsic force in noncontact ACL injuries.
Colby and coworkers21 measured hamstring and quadriceps muscle activation and knee flexion angles during eccentric motion of sidestep cutting, cross-cutting, stopping, and landing in 15 collegiate athletes. A high-level quadriceps muscle activation occurred just before foot-strike and peaked in mideccentric motion. The peak quadriceps muscle activation occurred between 39° (stopping) and 53° (cross-cutting) of knee flexion and averaged between 126% (landing) and 161% (stopping) of that measured in a maximum isometric contraction. Hamstring muscle activation was submaximal at and after foot-strike. The minimal hamstring muscle activation occurred between 21° (stopping) and 34° (cutting) of knee flexion and averaged between 14% (landing) and 40% (cross-cutting) that of a maximum isometric contraction. The knee flexion position at which foot-strike occurred during all four activities averaged 22° (range, 14° on stopping to 29° on cross-cutting). The authors concluded that the combination of the high level of quadriceps activity, low level of hamstrings activity, and low angle of knee flexion during eccentric contractions in these maneuvers could produce significant anterior translation of the tibia. The subjects included 9 men and 6 women; a gender comparison was not conducted.
Gender Differences in Movement Patterns on Landing and Take-Off
A study conducted at the authors’ laboratory48 using a two-camera, video-based optoelectronic digitizer and a multicomponent force plate was one of the first to demonstrate gender differences in movement patterns. Eleven high school female volleyball players were matched with 9 male athletes according to age, height, and weight and taken through jumping tasks and isokinetic lower extremity muscle strength testing. The males demonstrated greater knee extension moments on landing and take-off, which were interpreted to be likely due to their high use of the hamstrings musculature. Males also had a greater mean hamstring-to-quadriceps ratio on isokinetic testing at 360°/sec. Interestingly, males had significantly greater peak landing forces than females (6.1 and 4.2 times body weight, respectively; P < .01). The hypothesis was advanced that male athletes most likely use different mechanisms than those used by female athletes to compensate for these high landing forces. The investigation did not find significant gender differences with respect to knee abduction-adduction moments, knee flexion angles on landing and take-off, flexion moments, and ankle and hip flexion-extension and abduction-adduction moments.
Huston and associates51 found significant differences between genders on the knee flexion angle measured at impact from a drop-jump. Ten males and 10 females, matched for height, performed three drop-jumps from heights of 20, 40, and 60 cm. The men consistently demonstrated greater knee flexion angles than the women at 20 cm (8° and 5.4°, respectively; P < .05), 40 cm (10° and 5.4° respectively; P < .05), and 60 cm (16° and 7°, respectively; P < .05). The authors hypothesized that ground reaction forces are likely to be greater in women per unit body weight than in men because women land with a straighter knee.
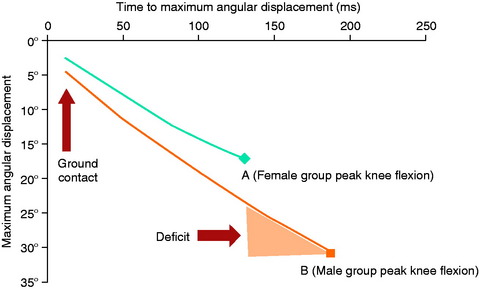
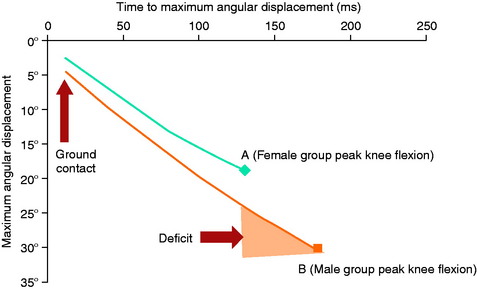
Lephart and colleagues62 evaluated kinematic and ground reaction forces in 30 collegiate athletes on single-leg landing and single-leg forward hopping. In both tasks, the females had significantly less knee flexion and lower leg internal rotation after impact than males and also took less time to reach their maximum knee flexion subsequent to impact (Figs. 15-7 and 15-8). The authors interpreted these findings to indicate that women experience a more abrupt absorption of impact forces on landing. The women also demonstrated greater hip internal rotation with lower leg external rotation from the point of impact to the maximum rotation position. There was no difference in vertical ground reaction forces between genders.
Decker and coworkers26 examined kinetic, kinematic, and energetic indices of 9 female and 12 male recreational athletes during a two-legged drop-jump task. The females demonstrated significantly greater knee extension and ankle plantar flexion angles at initial ground contact (P < .05). The female group also had greater energy absorption from the knee and ankle than from the hip (P < .05), whereas the male group had equal amounts of energy absorption from all lower extremity joints. The female group performed 34% less negative hip work, 30% more negative knee work, and 52% more negative ankle work than the male group (P < .05). There were no differences between the groups in vertical ground reaction forces. The findings indicated that females were in a more erect posture on initial impact than the males; however, the general external loading conditions were similar between genders. The women preferred to use the ankle musculature to absorb impact forces, which was accompanied with greater knee extension and ankle plantar flexion angles. Conversely, the males demonstrated greater knee flexion and less plantar flexion angles on impact, allowing a transfer of the forces to the larger muscles such as the hip extensors.
Salci and associates91 reported that female collegiate volleyball players landed with lower knee and hip flexion angles and higher ground reaction forces than male players during simulated spike and block maneuvers. Sell and colleagues96 conducted an investigation involving high school basketball players in which both planned and reactive (to a visual cue) stop-jump tasks were performed vertically, horizontally to the left, and horizontally to the right. During the reactive tasks, females had lower maximum knee flexion angles than males (68.4° and 74.9°, respectively; P = .001), greater maximum knee valgus angles (–7.5° and –4.2°, respectively; P < .05), greater anterior shear force at peak posterior ground reaction force (P < .05), and greater knee flexion moment at peak posterior ground reaction force (P < .05). During the horizontal jump to the left, females had significantly lower maximum knee flexion angles (P = .007), lower knee flexion at posterior ground reaction force (P = .006), and greater knee valgus at posterior ground reaction force (P < .05). The authors hypothesized that these differences could place greater strain on the female ACL. For all subjects, the horizontal jump to the left (to the medial aspect of the right knee) produced greater vertical and posterior ground reaction forces, proximal anterior tibial shear force, valgus and flexion moments, and lowest knee flexion angles than the other jumps. In addition, measured knee kinematics and kinetics were significantly altered during the reactive (unplanned) jumps. The authors recommended that future study designs take into account jump direction and simulate as closely as possible actual playing conditions to more accurately study ACL risk factors.
In contrast to many other studies, Fagenbaum and Darling30 reported that female athletes had significantly greater knee flexion angles (from 10°–14°) on landing than male athletes (P < .05), all of whom were collegiate basketball players attending the same university. The females demonstrated greater knee flexion both before and upon contact. Women also landed with greater knee flexion acceleration than men (P < .05). Cowling and Steele22 measured knee, hip, and trunk flexion angles in 11 females and 9 males matched for sport during a dynamic and abrupt deceleration single-leg task. No significant differences were found between genders in flexion angles on landing.
Gender Differences in Movement Patterns on Cutting
Malinzak and coworkers69 reported that female athletes had smaller knee flexion angles, greater valgus angles, increased quadriceps muscle activation, and decreased hamstring muscle activation during the stance cycle of straight running and two preplanned cutting maneuvers. The authors believed that these differences in lower extremity motion patterns could have been due to differences in anatomic structures, motor controls, or physiologic characteristics, although none of these factors was measured. Another investigation reported that during running, females had significantly greater hip internal rotation, peak hip adduction, and peak knee abduction and were in a greater abducted knee position throughout stance than males.32
Pollard and associates86 studied three-dimensional hip and knee joint kinematics and moments during a randomly cued cutting maneuver in 24 experienced collegiate soccer players. The authors reported no differences between genders in peak knee joint abduction or internal rotation angles during the first 0° to 40° of knee flexion across the stance phase. There were also no differences with respect to peak hip internal rotation angles. Females did demonstrate significantly less hip abduction than the males (P = .03). No gender differences were found for peak knee adduction, knee external rotation, hip abduction, or hip external rotation joint moments. The authors speculated that the failure to find differences in mechanics could have been a result of years of training and exposure to the same sport.
Besier and colleagues10,11 studied external knee moments and knee flexion angles during straight running, sidestepping, and crossover cutting in male subjects in two investigations. The data revealed that large increases occurred during cutting and sidestepping in varus-valgus and internal-external rotation moments compared with straight running (P < .05). The authors concluded that these movements placed the ACL at higher risk of injury, particularly at low knee flexion angles. During sidestepping, combined external loads of flexion, valgus, and internal rotation were observed, potentially increasing the load on both the ACL and the MCL. During cutting, combined flexion and varus loads could place large loads on the fibular collateral ligament. Female athletes were not included in these investigations.
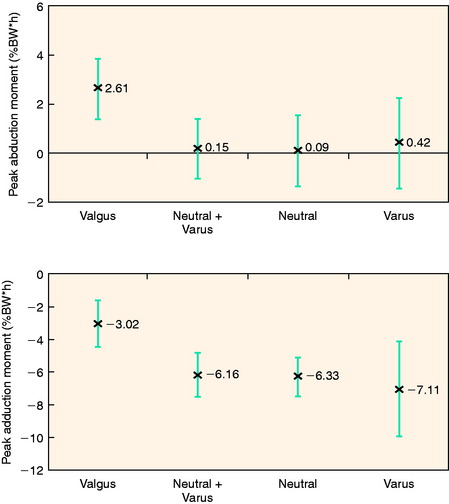
Chaudhari and coworkers20 observed a correlation between frontal plane lower limb alignment and knee moments, because subjects who assumed a valgus lower limb position during a 90° lateral run-to-cut maneuver had significantly higher knee abduction moments than those who had a neutral or varus lower limb position (Fig. 15-9; P < .01). Of the 21 subjects tested, 67% of females assumed a lower limb valgus alignment compared with 22% of males.
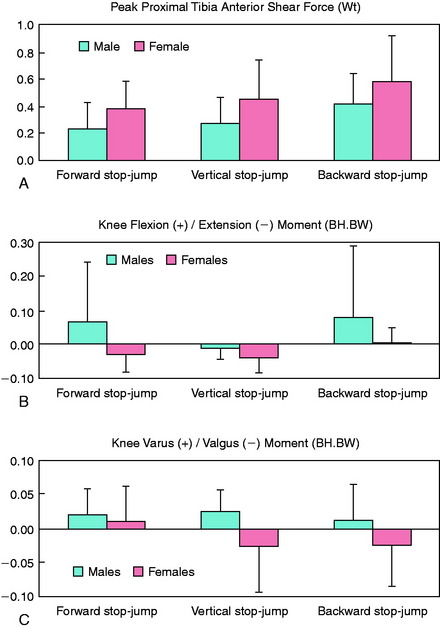
Gender Differences in Movement Patterns on Stop-Jump Tasks
A gender comparison of knee kinetics in three stop-jump tasks (Fig. 15-10) found that women had significantly greater proximal anterior shear forces, extension moments and valgus moments on landing than men (Fig. 15-11).17 The investigators believed that the increased proximal shear force was due to a high quadriceps muscle force, a low hamstrings muscle force, a straight knee on landing, or a combination of all of these factors. There was no difference between male and female athletes in knee valgus-varus moments, thereby refuting that this moment is responsible for the gender disparity in noncontact ACL injury rates. Chappell and associates16 also assessed the effect of fatigue on knee kinetics in these same stop-jump tasks. Female subjects had significantly greater peak proximal tibial anterior shear forces than males, greater knee extension moments at peak proximal tibial anterior shear force, and smaller knee flexion angles (P = .001, all comparisons) in both unfatigued and fatigued states. The mean valgus moment at the peak proximal tibial anterior shear force of female subjects increased 96% from the unfatigued to the fatigued condition (from 0.026–0.051 times body height x weight). Male subjects decreased mean valgus moment by 43% between test conditions. The authors concluded that fatigue increased the risk of ACL injury more in females than in males.
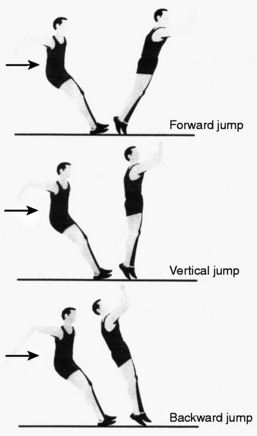
FIGURE 15-10 Three stop-jump tasks.
(From Chappell, J. D.; Yu, B.; Kirkendall, D. T.; Garrett, W. E.: A comparison of knee kinetics between male and female recreational athletes in stop-jump tasks. Am J Sports Med 30:261–267, 2002.)
A third investigation from Chappell and colleagues15 was conducted to determine whether gender differences existed during the preparation for landing in the vertical stop-jump task. Female recreational athletes displayed less knee and hip flexion, less hip external rotation, and increased hip abduction than male athletes upon preparation for landing. The authors hypothesized that the athletes “preprogrammed” these lower extremity motions during the flight phase of the last step of the approach run in this task.
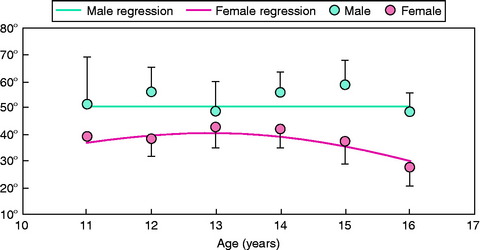
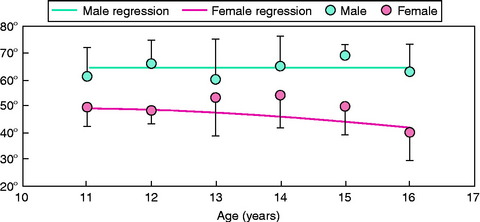
Yu and coworkers116 studied lower extremity kinematics during a stop-jump task in soccer players aged 11 to 16 years. The athletes were divided into six age groups, with each group composed of five female and five male subjects. Female players older than 12 years had decreased knee and hip flexion angles (Figs. 15-12 and 15-13) than the male athletes on landing. All players younger than 12 years had valgus knee angles at initial foot contact with the ground. Female players increased the amount of knee valgus motion as age increased. However, male players older than 12 years demonstrated a varus knee angle at initial contact. The authors acknowledged the small sample size as a limitation of the study.
Gender Differences in Movement Patterns on Squatting
During a dynamic single-leg squat in 18 healthy intercollegiate athletes (9 men, 9 women), Zeller and associates119 reported that female athletes had significantly greater ankle dorsiflexion, ankle pronation, hip adduction, and hip flexion than males. The women began the movement in greater valgus alignment and remained in this alignment throughout the squat. In addition, the women had less trunk lateral flexion than the men. The investigation revealed that women had poor hip control, which resulted in an adducted position that in turn allowed the femur to internally rotate, which placed the knee into a valgus position.
Gender Differences in Muscle Strength, Activation, and Recruitment Patterns
Marked differences between adolescent and adult male and female athletes in quadriceps and hamstrings peak torques, even when normalized for body weight, have been documented by numerous investigations.8,48,52,62,91 One of the largest studies conducted to date on 853 females and 177 males aged 9 to 17 demonstrated that significant gender differences in lower extremity strength become evident at age 14 (see Chapter 16, Lower Limb Neuromuscular Control and Strength in Prepubescent and Adolescent Male and Female Athletes).8 This investigation revealed that females appear to reach peak hamstrings strength at age 11, with no significant difference found in this factor between girls 11 years of age and those up to 17 years of age. No difference in isokinetic muscle strength values between boys and girls younger than 14 years has been reported by many laboratories.24,25,46,49,87,95,107
Huston and Wojtys52 studied lower extremity muscle strength, endurance, reaction time, and recruitment order in response to an anterior tibial translation force in 100 elite collegiate athletes and 40 matched nonathletic controls. The female athletes had significantly weaker knee flexor and extensor peak torques (normalized for body weight, 60°/sec and 240°/sec) and endurance values than the male athletes and were only marginally stronger than the female controls. The female athletes had slower time-to-peak torque values for knee flexors than the male athletes (430 and 328 msec, respectively; P < .001). Only 28% of the female athletes recruited their hamstrings first in response to an anterior tibial translation force compared with 45% of the other three subgroups. The preferred order of muscle recruitment in the female athletes was quadriceps, hamstrings, and gastrocnemius. In contrast, the preferred order of muscle recruitment in the male athletes, male controls, and female controls was hamstrings, quadriceps, and gastrocnemius.
Rozzi and associates90 failed to find a gender difference in time-to-peak torque in 34 healthy collegiate athletes tested at 180°/sec. On a single-leg drop jump test, no differences were detected between genders in mean onset times for the quadriceps or hamstrings musculatures. The female athletes demonstrated greater electromyographic (EMG) peak amplitude and area of the lateral hamstring on landing. In addition, the female athletes had greater anterior tibial displacements and reduced knee joint proprioception (time to detect the knee moving into extension) than the male athletes. These investigators postulated that the female athletes adopted compensatory mechanisms of increased hamstring activity to achieve knee stability in the presence of increased inherent joint instability.
Cowling and Steele22 measured muscle activation patterns in 11 females and 7 males during a dynamic and abrupt deceleration single-leg task. There were no significant differences between genders in quadriceps muscle activation patterns on landing. However, males had a significant delay in the onset of semimembranosus muscle burst peak time relative to initial contact compared with females (113 ± 46 msec and 173 ± 54 msec, respectively; P < .05). The authors postulated that this delay allowed peak hamstring muscle activity to coincide with the anterior tibiofemoral joint forces generated just after initial contact and enable the hamstrings to act as a synergist to the ACL.
Zeller and associates119 measured muscle activity during a single-leg dynamic squat in nine female and nine male collegiate athletes. The women had greater quadriceps femoris activation than the men in both the area under the linear envelope (78.8% ± 26.1% and 34.4% ± 16.4% of maximal voluntary isometric contraction, respectively; P < .05) and muscle activation (83.4% ± 14.5% and 36.2% ± 14.5% of maximal voluntary isometric contraction, respectively; P < .05). Chappell and colleagues15 measured muscle activation during the preparation for landing in the vertical stop-jump in recreational athletes. The females had greater quadriceps and hamstrings muscle activation than the males during landing preparation, but had lower hamstring activation after landing (foot-strike).
Leetun and associates61 measured hip abduction and external rotation isometric strength, abdominal muscle function, and back extensor and quadratus lumborum endurance in 79 female and 60 male intercollegiate athletes. The athletes were tested prior to the onset of their sport season and then followed for that season for injuries. The male athletes had greater hip isometric abduction (P < .05) and external rotation (P < .001) strength than the females. Only 1 athlete in the series sustained an ACL injury.
Gender Differences in Knee Stiffness
Wojtys and colleagues111 measured passive and active anterior shear stiffness of the knee joint in 10 men and 13 women. The subjects were placed in a knee testing apparatus that recorded anterior tibial translation and muscle activity with surface electromyography. Tests were conducted in a passive state and then in an active state in response to an anterior tibial translation force that was 20% of the subject’s body weight. Knee shear stiffness values were obtained by dividing the load of the anteriorly directed force by the anterior displacement of the knee joint. All subjects had uninjured, physiologically lax knees (≥6 mm anterior tibial translation on KT-1000 testing). There was no difference between the men and women in passive anterior tibial translation. Whereas there was no significant difference between genders in passive shear stiffness, men produced significantly higher active stiffness values during a maximum co-contraction (70.9 and 40.7 N/mm, respectively; P = .005). Men increased knee joint stiffness by 379% compared with the passive state, and women increased this value by 212%. There was no association between muscle strength, time-to-peak torque, or body height and the ability to increase shear stiffness. No difference was found between genders in EMG activity levels of the lower extremity.
In a separate investigation, Wojtys and coworkers114 reported that female athletes involved in pivoting sports had significantly smaller increases in torsional stiffness of the knee under internal rotation loading conditions than male athletes (159% ± 13% and 275% ± 39%; P = .001). The 24 athletes were matched for age, height, weight, BMI, shoe size, and activity level.
A reduction in active muscle stiffness in females compared with males was reported by Granata and associates37,38 during isometric knee flexion and extension and hopping tasks. These authors noted that effective stiffness increased linearly with the applied torque load. The gender difference was amplified at higher loads, leading the investigators to conclude that this finding had implications for potential injury during functional loading tasks.
Padua and colleagues84 found no differences between genders in leg stiffness during two-legged hopping tasks when the data were normalized for body mass. Significant differences were detected in stiffness prior to normalization, leading the authors to conclude that this finding was due to the lighter mass of the female subjects. No gender associations were found for joint angles at initial ground contact or joint excursions of the knees and ankles. Females recruited 46% greater quadriceps activity than the males and 37% greater soleus activity; however, no difference was found between genders in hamstrings activity during the hopping tasks.
1 Agel J., Arendt E.A., Bershadsky B. Anterior cruciate ligament injury in National Collegiate Athletic Association basketball and soccer: a 13-year review. Am J Sports Med. 2005;33:524-530.
2 Albright J.P., et al. Medial collateral ligament knee sprains in college football. Effectiveness of preventive braces. Am J Sports Med. 1994;22:12-18.
3 Allen M.K., Glasoe W.M. Metrecom measurement of navicular drop in subjects with anterior cruciate ligament injury. J Athl Train. 2000;35:403-406.
4 Anderson A.F., Dome D.C., Gautam S., et al. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med. 2001;29:58-66.
5 Anderson A.F., Lipscomb A.B., Liudahl K.J., Addlestone R.B. Analysis of the intercondylar notch by computed tomography. Am J Sports Med. 1987;15:547-552.
6 Arendt E., Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995;23:694-701.
7 Arendt E.A., Agel J., Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999;34:86-92.
8 Barber-Westin S.D., Noyes F.R., Galloway M. Jump-land characteristics and muscle strength development in young athletes: a gender comparison of 1140 athletes 9 to 17 years of age. Am J Sports Med. 2006;34:375-384.
9 Beckett M.E., Massie D.L., Bowers K.D., Stoll D.A. Incidence of hyperpronation in the ACL injured knee: a clinical perspective. J Athl Train. 1992;27:58-62.
10 Besier T.F., Lloyd D.G., Ackland T.R., Cochrane J.L. Anticipatory effects on knee joint loading during running and cutting maneuvers. Med Sci Sports Exerc. 2001;33:1176-1181.
11 Besier T.F., Lloyd D.G., Cochrane J.L., Ackland T.R. External loading of the knee joint during running and cutting maneuvers. Med Sci Sports Exerc. 2001;33:1168-1175.
12 Beynnon B.D., Bernstein I.M., Belisle A., et al. The effect of estradiol and progesterone on knee and ankle joint laxity. Am J Sports Med. 2005;33:1298-1304.
13 Beynnon B.D., Johnson R.J., Braun S., et al. The relationship between menstrual cycle phase and anterior cruciate ligament injury: a case-control study of recreational alpine skiers. Am J Sports Med. 2006;34:757-764.
14 Chandrashekar N., Slauterbeck J., Hashemi J. Sex-based differences in the anthropometric characteristics of the anterior cruciate ligament and its relation to intercondylar notch geometry: a cadaveric study. Am J Sports Med. 2005;33:1492-1498.
15 Chappell J.D., Creighton R.A., Giuliani C., et al. Kinematics and electromyography of landing preparation in vertical stop-jump: risks for noncontact anterior cruciate ligament injury. Am J Sports Med. 2007;35:235-241.
16 Chappell J.D., Herman D.C., Knight B.S., et al. Effect of fatigue on knee kinetics and kinematics in stop-jump tasks. Am J Sports Med. 2005;33:1022-1029.
17 Chappell J.D., Yu B., Kirkendall D.T., Garrett W.E. A comparison of knee kinetics between male and female recreational athletes in stop-jump tasks. Am J Sports Med. 2002;30:261-267.
18 Charlton W.P., St. John T.A., Ciccotti M.G., et al. Differences in femoral notch anatomy between men and women: a magnetic resonance imaging study. Am J Sports Med. 2002;30:329-333.
19 Chaudhari A.M., Lindenfeld T.N., Andriacchi T.P., et al. Knee and hip loading patterns at different phases in the menstrual cycle: implications for the gender difference in anterior cruciate ligament injury rates. Am J Sports Med. 2007;35:793-800.
20 Chaudhari A.M., Hearn B.K., Leveille L.A., et al. The effects of dynamic limb alignment on knee moments during single limb landing: implications for the analysis of the non-contact injury to the anterior cruciate ligament. Proceedings of the 2003 Summer Bioengineering Conference, June 25–29, Key Biscayne, FL. 2003.
21 Colby S., Francisco A., Yu B., Kirkendall D., et al. Electromyographic and kinematic analysis of cutting maneuvers. Implications for anterior cruciate ligament injury. Am J Sports Med. 2000;28:234-240.
22 Cowling E.J., Steele J.R. Is lower limb muscle synchrony during landing affected by gender? Implications for variations in ACL injury rates. J Electromyogr Kinesiol. 2001;11:263-268.
23 Davis T.J., Shelbourne K.D., Klootwyk T.E. Correlation of the intercondylar notch width of the femur to the width of the anterior and posterior cruciate ligaments. Knee Surg Sports Traumatol Arthrosc. 1999;7:209-214.
24 De Ste Croix M.B., Armstrong N., Welsman J.R., Sharpe P. Longitudinal changes in isokinetic leg strength in 10- to 14-year-olds. Ann Hum Biol. 2002;29:50-62.
25 De Ste Croix M.B.A., Armstrong N., Welsman J.R. Concentric isokinetic leg strength in pre-teen, teenage and adult males and females. Biol Sport. 1999;16:75-86.
26 Decker M.J., Torry M.R., Wyland D.J., et al. Gender differences in lower extremity kinematics, kinetics and energy absorption during landing. Clin Biomech (Bristol, Avon). 2003;18:662-669.
27 Deie M., Sakamaki Y., Sumen Y., et al. Anterior knee laxity in young women varies with their menstrual cycle. Int Orthop. 2002;26:154-156.
28 DeMorat G., Weinhold P., Blackburn T., et al. Aggressive quadriceps loading can induce noncontact anterior cruciate ligament injury. Am J Sports Med. 2004;32:477-483.
29 Dufek J.S., Bates B.T. The evaluation and prediction of impact forces during landings. Med Sci Sports Exerc. 1990;22:370-377.
30 Fagenbaum R., Darling W.G. Jump landing strategies in male and female college athletes and the implications of such strategies for anterior cruciate ligament injury. Am J Sports Med. 2003;31:233-240.
31 Faryniarz D.A., Bhargava M., Lajam C., et al. Quantitation of estrogen receptors and relaxin binding in human anterior cruciate ligament fibroblasts. In Vitro Cell Dev Biol Anim. 2006;42:176-181.
32 Ferber R., Davis I.M., Williams D.S.3rd. Gender differences in lower extremity mechanics during running. Clin Biomech (Bristol, Avon). 2003;18:350-357.
33 Ferretti A., Papandrea P., Conteduca F., Mariani P.P. Knee ligament injuries in volleyball players. Am J Sports Med. 1992;20:203-207.
34 Flynn R.K., Pedersen C.L., Birmingham T.B., et al. The familial predisposition toward tearing the anterior cruciate ligament: a case control study. Am J Sports Med. 2005;33:23-28.
35 Gerberich S.G., Luhmann S., Finke C., et al. Analysis of severe injuries associated with volleyball activities. Physician Sportsmed. 1987;15:75-79.
36 Good L., Odensten M., Gillquist J. Intercondylar notch measurements with special reference to anterior cruciate ligament surgery. Clin Orthop Relat Res. 1991;263:185-189.
37 Granata K.P., Padua D.A., Wilson S.E. Gender differences in active musculoskeletal stiffness. Part II. Quantification of leg stiffness during functional hopping tasks. J Electromyogr Kinesiol. 2002;12:127-135.
38 Granata K.P., Wilson S.E., Padua D.A. Gender differences in active musculoskeletal stiffness. Part I. Quantification in controlled measurements of knee joint dynamics. J Electromyogr Kinesiol. 2002;12:119-126.
39 Gray J., Taunton J.E., McKenzie D.C., et al. A survey of injuries to the anterior cruciate ligament of the knee in female basketball players. Int J Sports Med. 1985;6:314-316.
40 Greenfield M.L., Kuhn J.E., Wojtys E.M. A statistics primer. Power analysis and sample size determination. Am J Sports Med. 1997;25:138-140.
41 Griffin L.Y., et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34:1512-1532.
42 Grood E.S., Suntay W.J., Noyes F.R., Butler D.L. Biomechanics of the knee-extension exercise. Effect of cutting the anterior cruciate ligament. J Bone Joint Surg Am. 1984;66:725-734.
43 Gwinn D.E., Wilckens J.H., McDevitt E.R., et al. The relative incidence of anterior cruciate ligament injury in men and women at the United States Naval Academy. Am J Sports Med. 2000;28:98-102.
44 Harner C.D., Paulos L.E., Greenwald A.E., et al. Detailed analysis of patients with bilateral anterior cruciate ligament injuries. Am J Sports Med. 1994;22:37-43.
45 Heitz N.A., Eisenman P.A., Beck C.L., Walker J.A. Hormonal changes throughout the menstrual cycle and increased anterior cruciate ligament laxity in females. J Athl Train. 1999;34:144-149.
46 Henderson R.C., Howes C.L., Erickson K.L., et al. Knee flexor-extensor strength in children. J Orthop Sports Phys Ther. 1993;18:559-563.
47 Herzog R.J., Silliman J.F., Hutton K., et al. Measurements of the intercondylar notch by plain film radiography and magnetic resonance imaging. Am J Sports Med. 1994;22:204-210.
48 Hewett T.E., Stroupe A.L., Nance T.A., Noyes F.R. Plyometric training in female athletes. Decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24:765-773.
49 Holm I., Steen H., Olstad M. Isokinetic muscle performance in growing boys from pre-teen to maturity. An eleven-year longitudinal study. Isok Exer Sci. 2005;13:153-158.
50 Houseworth S.W., Mauro V.J., Mellon B.A., Kieffer D.A. The intercondylar notch in acute tears of the anterior cruciate ligament: a computer graphics study. Am J Sports Med. 1987;15:221-224.
51 Huston L.J., Vibert B., Ashton-Miller J.A., Wojtys E.M. Gender differences in knee angle when landing from a drop-jump. Am J Knee Surg. 2001;14:215-219.
52 Huston L.J., Wojtys E.M. Neuromuscular performance characteristics in elite female athletes. Am J Sports Med. 1996;24:427-436.
53 Hutchinson M.R., Ireland M.L. Knee injuries in female athletes. Sports Med. 1995;19:288-302.
54 Ireland M.L., Ballantyne B.T., Little K., McClay I.S. A radiographic analysis of the relationship between the size and shape of the intercondylar notch and anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2001;9:200-205.
55 Kirkendall D.T., Garrett W.E.Jr. The anterior cruciate ligament enigma. Injury mechanisms and prevention. Clin Orthop. 2000;372:64-68.
56 Knapik J.J., Wright J.E., Mawdsley R.H., Braun J. Isometric, isotonic, and isokinetic torque variations in four muscle groups through a range of joint motion. Phys Ther. 1983;63:938-947.
57 Krosshaug T., Nakamae A., Boden B.P., et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35:359-367.
58 Lambson R.B., Barnhill B.S., Higgins R.W. Football cleat design and its effect on anterior cruciate ligament injuries. A threeyear prospective study. Am J Sports Med. 1996;24:155-159.
59 LaPrade R.F., Burnett Q.M. Femoral intercondylar notch stenosis and correlation to anterior cruciate ligament injuries. A prospective study. Am J Sports Med. 1994;22:198-203.
60 Larsson L.G., Baum J., Mudholkar G.S. Hypermobility: features and differential incidence between the sexes. Arthritis Rheum. 1987;30:1426-1430.
61 Leetun D.T., Ireland M.L., Willson J.D., et al. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004;36:926-934.
62 Lephart S.M., Ferris C.M., Riemann B.L., et al. Gender differences in strength and lower extremity kinematics during landing. Clin Orthop. 2002;401:162-169.
63 Lindenfeld T.N., Schmitt D.J., Hendy M.P., et al. Incidence of injury in indoor soccer. Am J Sports Med. 1994;22:364-371.
64 Liu S.H., al-Shaikh R., Panossian V., et al. Primary immunolocalization of estrogen and progesterone target cells in the human anterior cruciate ligament. J Orthop Res. 1996;14:526-533.
65 Lombardo S., Sethi P.M., Starkey C. Intercondylar notch stenosis is not a risk factor for anterior cruciate ligament tears in professional male basketball players: an 11-year prospective study. Am J Sports Med. 2005;33:29-34.
66 Loudon J.K., Jenkins W., Loudon K.L. The relationship between static posture and ACL injury in female athletes. J Orthop Sports Phys Ther. 1996;24:91-97.
67 Lund-Hanssen H., Gannon J., Engebretsen L., et al. Intercondylar notch width and the risk for anterior cruciate ligament rupture. A case-control study in 46 female handball players. Acta Orthop Scand. 1994;65:529-532.
68 MacWilliams B.A., Wilson D.R., DesJardins J.D., et al. Hamstrings cocontraction reduces internal rotation, anterior translation, and anterior cruciate ligament load in weight-bearing flexion. J Orthop Res. 1999;17:817-822.
69 Malinzak R.A., Colby S.M., Kirkendall D.T., et al. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin Biomech (Bristol, Avon). 2001;16:438-445.
70 Messina D.F., Farney W.C., DeLee J.C. The incidence of injury in Texas high school basketball. A prospective study among male and female athletes. Am J Sports Med. 1999;27:294-299.
71 Meyers M.C., Barnhill B.S. Incidence, causes, and severity of high school football injuries on FieldTurf versus natural grass: a 5-year prospective study. Am J Sports Med. 2004;32:1626-1638.
72 Mizrahi J., Susak Z. Analysis of parameters affecting impact force attenuation during landing in human vertical free fall. Eng Med. 1982;11:141-147.
73 Mizrahi J., Susak Z. In-vivo elastic and damping response of the human leg to impact forces. J Biomech Eng. 1982;104:63-66.
74 More R.C., Karras B.T., Neiman F., et al. Hamstrings—an anterior cruciate ligament protagonist: an in vitro study. Am J Sports Med. 1993;21:231-237.
75 Muneta T., Takakuda K., Yamamoto H. Intercondylar notch width and its relation to the configuration and cross-sectional area of the anterior cruciate ligament. A cadaveric knee study. Am J Sports Med. 1997;25:69-72.
76 Najibi S., Albright J.P. The use of knee braces, part 1: prophylactic knee braces in contact sports. Am J Sports Med. 2005;33:602-611.
77 Noyes F.R., Sonstegard D.A. Biomechanical function of the pes anserinus at the knee and the effect of its transplantation. J Bone Joint Surg Am. 1973;55:1225-1241.
78 O’Connor J.J. Can muscle co-contraction protect knee ligaments after injury or repair? J Bone Joint Surg Br. 1993;75:41-48.
79 Oggero E., Pagnacco G., Morr D.R., et al. The mechanics of drop landing on a flat surface—a preliminary study. Biomed Sci Instrum. 1997;33:53-58.
80 Olsen O.E., Myklebust G., Engebretsen L., Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32:1002-1012.
81 Olsen O.E., Myklebust G., Engebretsen L., et al. Relationship between floor type and risk of ACL injury in team handball. Scand J Med Sci Sports. 2003;13:299-304.
82 Orchard J., Seward H., McGivern J., Hood S. Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. Am J Sports Med. 2001;29:196-200.
83 Ostenberg A., Roos H. Injury risk factors in female European football. A prospective study of 123 players during one season. Scand J Med Sci Sports. 2000;10:279-285.
84 Padua D.A., Carcia C.R., Arnold B.L., Granata K.P. Gender differences in leg stiffness and stiffness recruitment strategy during two-legged hopping. J Mot Behav. 2005;37:111-125.
85 Pandy M.G., Shelburne K.B. Dependence of cruciate-ligament loading on muscle forces and external load. J Biomech. 1997;30:1015-1024.
86 Pollard C.D., Davis I.M., Hamill J. Influence of gender on hip and knee mechanics during a randomly cued cutting maneuver. Clin Biomech (Bristol, Avon). 2004;19:1022-1031.
87 Ramos E., Frontera W.R., Llopart A., Feliciano D. Muscle strength and hormonal levels in adolescents: gender related differences. Int J Sports Med. 1998;19:526-531.
88 Remvig L., Jensen D.V., Ward R.C. Epidemiology of general joint hypermobility and basis for the proposed criteria for benign joint hypermobility syndrome: review of the literature. J Rheumatol. 2007;34:804-809.
89 Rosene J.M., Fogarty T.D. Anterior tibial translation in collegiate athletes with normal anterior cruciate ligament integrity. J Athl Train. 1999;34:93-98.
90 Rozzi S.L., Lephart S.M., Gear W.S., Fu F.H. Knee joint laxity and neuromuscular characteristics of male and female soccer and basketball players. Am J Sports Med. 1999;27:312-319.
91 Salci Y., Kentel B.B., Heycan C., et al. Comparison of landing maneuvers between male and female college volleyball players. Clin Biomech (Bristol, Avon). 2004;19:622-628.
92 Schickendantz M.S., Weiker G.G. The predictive value of radiographs in the evaluation of unilateral and bilateral anterior cruciate ligament injuries. Am J Sports Med. 1993;21:110-113.
93 Scranton P.E.Jr., Whitesel J.P., Powell J.W., et al. A review of selected noncontact anterior cruciate ligament injuries in the National Football League. Foot Ankle Int. 1997;18:772-776.
94 Seckin U., Tur B.S., Yilmaz O., et al. The prevalence of joint hypermobility among high school students. Rheumatol Int. 2005;25:260-263.
95 Seger J.Y., Thorstensson A. Muscle strength and electromyogram in boys and girls followed through puberty. Eur J Appl Physiol. 2000;81:54-61.
96 Sell T.C., Ferris C.M., Abt J.P., et al. The effect of direction and reaction on the neuromuscular and biomechanical characteristics of the knee during tasks that simulate the noncontact anterior cruciate ligament injury mechanism. Am J Sports Med. 2006;34:43-54.
97 Shelbourne K.D., Davis T.J., Klootwyk T.E. The relationship between intercondylar notch width of the femur and the incidence of anterior cruciate ligament tears. A prospective study. Am J Sports Med. 1998;26:402-408.
98 Shultz S.J., Kirk S.E., Johnson M.L., et al. Relationship between sex hormones and anterior knee laxity across the menstrual cycle. Med Sci Sports Exerc. 2004;36:1165-1174.
99 Shultz S.J., Sander T.C., Kirk S.E., Perrin D.H. Sex differences in knee joint laxity change across the female menstrual cycle. J Sports Med Phys Fitness. 2005;45:594-603.
100 Simpson K.J., Kanter L. Jump distance of dance landings influencing internal joint forces: I. Axial forces. Med Sci Sports Exerc. 1997;29:916-927.
101 Simpson K.J., Pettit M. Jump distance of dance landings influencing internal joint forces: II. Shear forces. Med Sci Sports Exerc. 1997;29:928-936.
102 Sitler M., Ryan J., Hopkinson W., et al. The efficacy of a prophylactic knee brace to reduce knee injuries in football. A prospective, randomized study at West Point. Am J Sports Med. 1990;18:310-315.
103 Slauterbeck J.R., Fuzie S.F., Smith M.P., et al. The menstrual cycle, sex hormones, and anterior cruciate ligament injury. J Athl Train. 2002;37:275-278.
104 Smith J., Szczerba J.E., Arnold B.L., et al. Role of hyperpronation as a possible risk factor for anterior cruciate ligament injuries. J Athl Train. 1997;32:25-28.
105 Souryal T.O., Freeman T.R. Intercondylar notch size and anterior cruciate ligament injuries in athletes. A prospective study. Am J Sports Med. 1993;21:535-539.
106 Staeubli H.U., Adam O., Becker W., Burgkart R. Anterior cruciate ligament and intercondylar notch in the coronal oblique plane: anatomy complemented by magnetic resonance imaging in cruciate ligament-intact knees. Arthroscopy. 1999;15:349-359.
107 Sunnegardh J., Bratteby L.E., Nordesjo L.O., Nordgren B. Isometric and isokinetic muscle strength, anthropometry and physical activity in 8 and 13 year old Swedish children. Eur J Appl Physiol Occup Physiol. 1988;58:291-297.
108 Teitz C.C., Lind B.K., Sacks B.M. Symmetry of the femoral notch width index. Am J Sports Med. 1997;25:687-690.
109 Uhorchak J.M., Scoville C.R., Williams G.N., et al. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003;31:831-842.
110 Wentorf F.A., Sudoh K., Moses C., et al. The effects of estrogen on material and mechanical properties of the intra- and extra-articular knee structures. Am J Sports Med. 2006;34:1948-1952.
111 Wojtys E.M., Ashton-Miller J.A., Huston L.J. A gender-related difference in the contribution of the knee musculature to sagittal-plane shear stiffness in subjects with similar knee laxity. J Bone Joint Surg Am. 2002;84:10-16.
112 Wojtys E.M., Huston L., Boynton M.D., et al. The effect of the menstrual cycle on anterior cruciate ligament injuries in women as determined by hormone levels. Am J Sports Med. 2002;30:182-188.
113 Wojtys E.M., Huston L.J., Lindenfeld T.N., et al. Association between the menstrual cycle and anterior cruciate ligament injuries in female athletes. Am J Sports Med. 1998;26:614-619.
114 Wojtys E.M., Huston L.J., Schock H.J., et al. Gender differences in muscular protection of the knee in torsion in size-matched athletes. J Bone Joint Surg Am. 2003;85:782-789.
115 Woodford-Rogers B., Cyphert L., Denegar C.R. Risk factors for anterior cruciate ligament injury in high school and college athletes. J Athl Train. 1994;29:343-346.
116 Yu B., McClure S.B., Onate J.A., et al. Age and gender effects on lower extremity kinematics of youth soccer players in a stop-jump task. Am J Sports Med. 2005;33:1356-1364.
117 Yu W.D., Liu S.H., Hatch J.D., et al. Effect of estrogen on cellular metabolism of the human anterior cruciate ligament. Clin Orthop Relat Res. 1999;366:229-238.
118 Yu W.D., Panossian V., Hatch J.D., et al. Combined effects of estrogen and progesterone on the anterior cruciate ligament. Clin Orthop Relat Res. 2001;383:268-281.
119 Zeller B.L., McCrory J.L., Kibler W.B., Uhl T.L. Differences in kinematics and electromyographic activity between men and women during the single-legged squat. Am J Sports Med. 2003;31:449-456.