Chapter 3 Risk and Gender Factors for Noncontact Anterior Cruciate Ligament Injury
Environmental Risk Factors
Certain studies have examined surface conditions relating to ACL injuries. Olsen et al1 and Torg et al2 both studied team handball and found an increased risk of ACL injury while playing on synthetic floors versus traditional parquet floors. Both believed that the increased friction of synthetic flooring was the cause. Orchard et al,3 Heidt et al,4 and Scranton et al5 all reported higher rainfall and cooler temperatures were related to decreased ACL injuries and theorized that dry, hot weather conditions promote increased frictional forces on the playing field, thus in turn resulting in increased injury rates.
Lambson et al6 in a 3-year prospective study looked at footwear to evaluate torsional resistance of modern football cleats. They compared four styles of football shoes and found that the edge design, a design having longer irregular cleats at the periphery and many smaller cleats interiorly, was associated with higher ACL injury rates.
Bracing Pros and Cons
Prophylactic and functional (postreconstructive) knee bracing has long been a controversial subject. Over the past 20 years, attitudes have fluctuated regarding the effectiveness of braces in preventing knee injury in the uninjured athlete, the ACL deficient athlete, and the ACL reconstructed athlete. A study by Decoster and Vailas7 on brace prescriptions patterns noted that there has been a decreasing tendency for orthopaedic surgeons to prescribe ACL braces. The authors also noted that a primary factor influencing brace prescription by orthopaedists was the activity level of the patient.7
Early studies on prophylactic brace wear by Teitz et al8 and Rovere et al9 indicated no benefit to brace wear. These authors cited increased rates of knee injury in some athletes using prophylactic knee braces. In contrast, two other studies—the West Point study by Sitler et al10 involving 1396 cadets at the U.S. Military Academy who played intramural tackle football and the Big Ten Conference study by Albright et al11 involving 987 NCAA football players—concluded that prophylactic knee braces were effective in reducing injury. Since these studies, there has been a paucity of data to support prophylactic bracing for ACL injury protection, but it is believed that braces may provide some advantage to reducing medial collateral ligament (MCL) injury.12,13
Braces are commonly prescribed following ACL injury or reconstruction; however, little evidence supports their physiological or biomechanical efficacy. In a prospective randomized clinical trial of functional bracing for ACL deficient athletes, Swirtun et al14 found that subjectively, patients had initial sense of increased stability, but these investigators were unable to find objective benefits. In contrast, Kocher et al studied the use of braces to prevent reinjury in 180 ACL deficient alpine skiers and found reinjury occurred in 2% of the braced skiers compared with 13% of the unbraced “control” skiers.15
Risberg et al investigated the effect of knee bracing after ACL reconstruction in a prospective clinical trial of 60 patients randomized postoperatively (30 braced and 30 without brace) with 2 years of follow-up.16 They found no evidence that bracing affected knee joint laxity, range of motion, muscle strength, functional knee tests, patient satisfaction, or pain in braced athletes compared with athletes who did not use a brace following ACL reconstruction. Furthermore, they found prolonged bracing, which they defined as brace wear 1 to 2 years postoperatively, produced decreases in quadriceps muscle strength. McDevitt et al in a prospective, randomized multicenter study of 100 subjects likewise found no significant differences between braced and nonbraced subjects following ACL reconstruction.17
It has been theorized that damage to the ACL can disrupt mechanoreceptors in the knee leading to decreased proprioception.18 Birmingham et al19 has suggested that brace wear may help to correct this deficit somewhat, but benefits do not carry over to more demanding tasks. To examine knee proprioception, researchers have studied the threshold for detection of passive knee motion and found that brace application to the ACL deficient limb does not improve the threshold to detect passive range of motion.20,21
Anatomical Risk Factors
Association Between Q Angle and Injury Risk
The Q angle, which typically ranges from 12 to 15 degrees, is formed by the intersection of two lines, one from the anterior superior iliac spine to the midpoint of the patella and another from the tibial tubercle to the same reference point on the patella. It has been proposed that an increased Q angle may be associated with an increased risk for knee injury because excessive lateral forces could negatively influence the knee’s mechanical alignment.22,23
Females have been reported to have larger Q angles than their male counterparts24,25; however, in a trigonometric evaluation, Grelsamer et al reported a mean difference of only 2.3 degrees between the Q angles of men and women and furthermore found that men and women of equal height demonstrated similar Q angles.26 Shambaugh et al25 studied the relationship between lower extremity alignment and injury rates in recreational basketball players and found larger Q angles in athletes who sustained knee injures. In contrast, other authors have not been able to relate injury to Q angle.22,27,28 Guerra et al29 reported that quadriceps contraction alters Q angle measurements, thus making it difficult to establish a direct link between static Q angle measurements and injury.
Notch Width as a Risk Factor
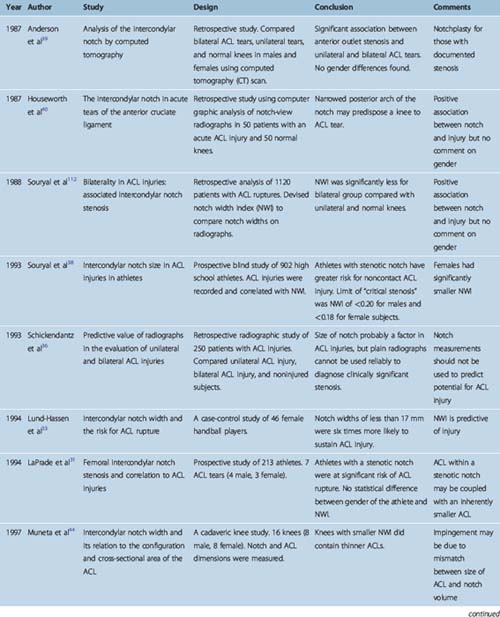
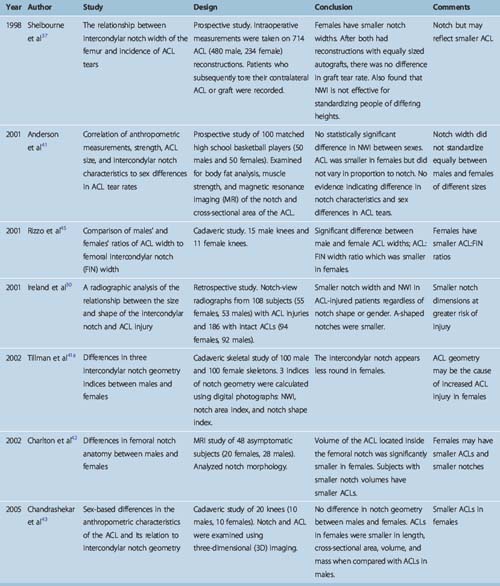
Structural characteristics of the distal femur and femoral intercondylar notch as well as ACL geometry and the ACL relationship to the intercondylar notch have been implicated as anthropometric factors associated with ACL injury rate disparity between males and females. It has been postulated that a smaller notch, termed notch stenosis, may cause impingement to the ACL and put it at increased risk of injury, or possibly a smaller notch may imply a smaller ACL leading to decreased load to failure. Although these factors have been heavily studied using plain radiography,30–38 computed tomography (CT),39,40 magnetic resonance imaging (MRI),41,42 and cadaveric43–45 and in vitro37 analysis, a lack of consistent measurement techniques and findings has made it difficult to interpret results. Therefore there is still no consensus relating morphology of the intercondylar notch to ACL injury rates. A chronological summary of the data is listed in Table 3-1.
Hormonal Risk Factors
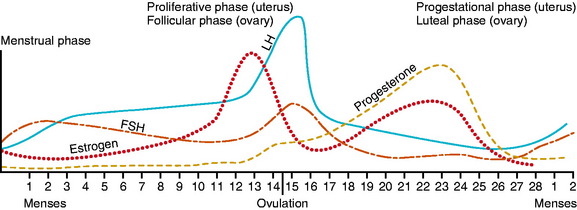
The increased incidence of ACL injury in women compared with men has raised interest regarding the influence of sex hormones on injury occurrence. Fig. 3-1 describes the menstrual cycle. A normal cycle is typically 28 to 30 days. The follicular phase (i.e., the stage of the follicle development) begins with menstruation and ends with ovulation. The latter lasts approximately 3 to 5 days and, if pregnancy does not occur, is followed by the luteal phase, which begins with the involution of the follicle and formation of the corpus luteum. Estradiol secretion is biphasic, peaking in both the follicular and luteal stages. Progesterone is produced by the corpus luteum and therefore occurs in the luteal phase only.
Monthly Distribution of Anterior Cruciate Ligament Injuries
Initial surveys of injury occurrence throughout the monthly menstrual cycle revealed that injuries were not equally distributed throughout the cycle but instead were clustered either around menstruation or the ovulation period of the cycle.46–48
However, the reliability of these early data was questioned because subjects were not frequently controlled for the use of birth control pills and hormonal assays were not done to verify cycle times; instead, athletes recalled or reported their menstrual history. Repeated studies using radioimmunoassays on serum, urine, or saliva verified the non–chance distribution of ACL injuries throughout the menstrual cycle.48–51
Sex Hormones and Laxity
If sex hormone levels do influence injury rates, how this occurs is not clear. Multiple studies in the past decade have focused on the influence of sex hormones on knee laxity, and some investigators have even correlated female sex hormone levels and laxity measures with menstrual cycle phase. In 1999, Wojtys and Huston52 reported on a series-controlled study of 12 females and 12 males, in which they found a decrease in knee laxity on day 12 of the monthly menstrual cycle in women versus no monthly variation in knee laxity in men.
In the following year, however, Belanger et al53reported no significant difference in anterior knee laxity throughout the monthly cycle in 18 Brown University athletes studied over 10 weeks. Similarly, Karageanes et al54 reported no significant changes in ACL laxity from the follicular to luteal phases. This research group measured laxity before workouts in 26 athletes, comparing these data to self-charted menstrual cycles. Van Lunen et al,55 using a within-subjects linear model, reported on 12 females tested for knee laxity at the onset of menses, near ovulation, and on day 23 with hormonal assays performed on blood drawn on those same days. They found no association between follicular, ovulatory, or luteal phase hormone concentrations and ACL laxity measures.
This is in contrast to an earlier study by Heitz et al,56 who not only compared laxity measures taken on days 1, 10, 11, 12, 13, 20, 21, 22, and 23 of a self-reported menstrual cycle but also compared these data with serum estradiol and progesterone levels as measured by immunoassays in seven active females who reported normal 28- to 30-day menstrual cycles. These investigators found a significant difference in anterior knee laxity when comparing laxity measures at baseline estrogen levels with peak levels of estrogen and when comparing laxity at baseline progesterone levels with that of peak progesterone levels. These results are similar to a series-controlled Japanese study57 involving 16 women and 8 men, which found no statistical difference in anterior displacement over time in men but did find variation in anterior knee laxity in women between the follicular and ovulatory phases and between the follicular and luteal phases at 89N displacement. Furthermore, Shultz et al58 obtained daily knee laxity measures as well as assayed daily serum samples for estradiol, progesterone, and testosterone in 25 females throughout one complete menstrual cycle and concluded that changes in sex hormones mediated changes in knee laxity across the menstrual cycle. Moreover, these investigators found a variable knee laxity response among females, with some females experiencing significant variation in knee laxity across the monthly cycle and others experiencing very little.
Even if an association can be demonstrated among sex hormones, menstrual phase, and increased laxity, an increase in knee laxity has not been reliably associated with an increased risk of ACL injury.59–62
Sex Hormones and Ligament Biology
Female sex hormones have been found in animal and human studies to have a direct effect on growth and development of bone, muscle, and connective tissue. In 1996, Liu et al63 reported receptor sites for estrogen and progesterone in the human ACL, and in 2005, Lovering and Romani reported androgen receptors in the female ACL as well, suggesting that these sex hormones could have a direct effect on the structure and composition of the ACL.64
In fact, in 1997, Liu et al reported a significant reduction in procollagen synthesis by ACL fibroblasts and in fibroblast proliferation with increasing estradiol concentrations.65 Similarly, Slauterbeck et al66 found that high-dose 17β-estradiol significantly decreased the tensile strength of the ACL in ovariectomized rabbits compared with the tensile strength of the ACL in ovariectomized rabbits not supplemented with estrogen. Seneviratne et al67 reported that despite the presence of estrogen receptors on ovine ACL fibroblasts, there was no significant difference in ACL fibroblast proliferation or collagen synthesis when cells in culture were exposed to 17β-estradiol at physiological concentrations. In 2003, Strickland et al,68 in a controlled laboratory study of 38 matured ewes, found that estrogen or a selective estrogen receptor agonist at physiological levels did not result in a change in the mechanical properties of the sheep’s knee ligament. Arendt et al69 mechanically tested ACLs of 26 young rhesus monkeys (14 ovariectomized and 12 sham-operated) and concluded that estrogen had no effect on the mechanical or material properties of the ACL in these primates.
Sex Hormones and Other Concerns
Perhaps sex hormones influence ACL injuries not by a direct effect on the mechanical properties of the ligament but on other injury-associated parameters such as balance, muscle response time, mood, and focus.70,71 Estrogen and progesterone have been found to influence the cardiovascular system, blood pressure, heart rate, minute ventilation, substrate metabolism, thermal regulation, resting O2 consumption, and other factors.72,73 Variable results regarding anaerobic performance and the menstrual cycle have been reported, with some researchers claiming no change in anaerobic ability across the cycle and others claiming greater anaerobic capacity and peak power during the luteal phase.74
Wojyts and Huston52 investigated the variations in strength, endurance, and time to peak torque in 12 women on days 1, 12, and 24 of a complete cycle and found no significant variation in any of these factors across the menstrual cycle.
Schultz et al have made the thoughtful statement that although we do not know how the impact of the menstrual cycle affects noncontact ACL injuries, the preponderance of evidence favors the idea that the incidence of noncontact ACL injuries does vary throughout the monthly cycle and does not occur by chance alone. Therefore, one has to question the validity of data accumulated in women regarding other risk factors for ACL injury that do not take into account the time of the monthly menstrual cycle during which the data were obtained.75 In summary, research in the area of sex hormones’ effects on ACL injury rates has been intense in the last several years, but many questions remain unanswered.
Neuromuscular Risk Factors
The majority of ACL injuries occur without direct contact made to the player’s knee. Players may describe a bump or a hit to another body area that throws them off balance (a perturbation), but in more than 70% of ACL injuries, a noncontact mechanism has been identified.27,47,76–78 Moreover, interviews with players and analysis of injury videotapes from basketball, soccer, football, and volleyball have revealed that most injuries occur with decelerating, as when stopping, cutting, changing directions, or landing a jump.79–81
However, the exact mechanism—that single action or cascade of events that ultimately results in an ACL injury—is still largely unknown. Markolf et al,82 using fresh frozen cadavers, applied combined loads to the tibia and measured the effects on the ACL through a wide range of motion angles. These researchers found that a combination of internal rotation and anterior tibial force resulted in the highest load to the ACL. Earlier, Markolf et al had reported that the ACL experienced large loads when the knee was near straight (i.e., at angles between 0 and 20 degrees of flexion).83
The most detailed analysis of the mechanism of ACL injury has been in alpine skiing, where videotape analysis of ACL injuries has revealed two potential mechanisms of injury.84,85 The most common is the so-called “phantom foot mechanism” that occurs when the skier falls or sits backwards, catching the inside edge of the tail of the ski, which results in internal rotation of the tibia with the knee flexed well beyond 90 degrees. The second injury mechanism in skiing occurs with a hard, off-balance landing. In this scenario, the skier’s boot “pushes” the tibia forward on landing, increasing the load on the ACL.
Garrett has suggested that a large eccentric quadriceps contraction with the knee in slight flexion can result in sufficient force to tear the ACL; in other words, the quadriceps could be the intrinsic force in a noncontact ACL injury.85a This theory was investigated in a laboratory study by DeMorat et al86 using 13 fresh frozen potted knees held in 20 degrees of flexion. A 4500N quadriceps force anteriorly displaced the tibia, resulting in damage to the ACL in 11 knees and gross disruption of this ligament in 6 of these 11 knees. Two knees sustained tibial plateau fractures.
It is known that joint stability is provided not only by the static ligament restraints but also by dynamic muscle contraction. In fact, Markolf reported that patients who were not athletes could increase varus and valgus knee stiffness by twofold to fourfold with isometric contraction of the hamstrings and quadriceps.87 Women have been found to be less able to stiffen their knees through muscle contraction than men, a factor that may place women at greater risk for ACL injury when compared with men.88–90
A study by Wojtys et al90 employing 23 volunteers (10 men and 13 women who were selected to participate because they had healthy but “loose knees” [i.e., a manual maximal anterior arthrometric laxity measurement of at least 6 mm]) found that maximal co-contraction of the knee significantly decreased mean anterior tibial translation in all volunteers, but the percent increase in sheer stiffness of the knee was greater in men (P = 0.003). This same research group earlier studied 10 elite female athletes and 10 elite male athletes with sex-matched, nonathlete controls and reported that female athletes compared with male athletes took longer to generate maximal hamstring muscle torque during isokinetic testing and contracted their quadriceps, rather than their hamstrings, as an initial response to anterior tibial translation. Overall, females had less strength and endurance than males and had greater anterior tibial laxity.91
Not only do women demonstrate variations in strength, laxity, and muscle recruitment, but a number of researches have reported that women perform cutting maneuvers and land jumps in a more upright posture—a posture shown by Markolf et al to put greater strain on the ACL.82,83,92–98 In contrast, in 1996 Hewett et al99 reported no difference in knee flexion angles on landing between males and females, and Fagenbaum and Darling evaluated eight females and six male varsity collegiate basketball players and reported that women landed with increased knee flexion angles.100
Recently, several research groups have used three-dimensional (3D) kinematics to evaluate landing and cutting movements.101–105 McLean et al evaluated side-stepping in 10 male and 10 female collegiate athletes and found women had significant larger normalized knee valgus moments than males.103 These findings are consistent with other researchers who reported larger knee valgus motions in women compared with men performing side-step cutting maneuvers96 and are also consistent with greater valgus motion reported in women doing jump-landing tasks.106,107
Researchers have also emphasized the relationship of knee position to neuromuscular control of the hip. They believe that knee valgus moments are related to hip flexion and internal rotation on contact during side-stepping,102 a relationship previously emphasized by Kibler.108
Ford et al,109 using 3D kinematic analysis of 81 high school basketball athletes (47 females and 34 males) performing a drop–vertical jump maneuver, reported that females landed with greater total valgus knee motion and a greater maximal valgus knee angle than male athletes. Moreover, this same group of researchers prospectively examined 205 female soccer, basketball, and volleyball players performing a jump-landing task and reported that of these 205 subjects, 9 sustained an ACL injury during the time of the study.107 These 9 subjects had a knee abduction angle on landing of 8 degrees greater (P > 0.05) than uninjured athletes and a 2.5 times greater knee abduction moment (P < 0.001) and 20% higher ground reaction force (P < 0.05) than those who did not sustain an ACL injury. Three-dimensional kinematic and kinetic analysis was used for the study.
Increased valgus knee movements in female recreational athletes during the landing phase of vertical and backward jumping were also reported by Chappell et al,92 but this research group found no difference in the magnitude of the knee varus-valgus moments between genders. These researchers also reported that female recreational athletes had an increased proximal tibial anterior sheer force during the landing phase in a stop-jump task compared with male recreational athletes.
In their investigation of gender differences in 3D hip and knee joint mechanics in college athletes performing five randomly cued cutting trials, Pollard et al found no gender differences in selected peak hip and knee joint kinematics and movements, except in peak hip abduction, where females demonstrated significantly less peak hip abduction than did males.105
Familial Tendency to Noncontact Anterior Cruciate Ligament Injury
In a retrospective study published in 1994, Harner et al110 compared 31 patients who sustained bilateral ACL injuries with 23 matched control subjects (i.e., no history of ACL injury) and reported a significant increase (P < 0.01) in the ACL incidence rate among immediate family members of the 31 ACL-injured patients compared with the controls. Similarly, Flynn et al111 compared 171 ACL-injured subjects with 171 matched controls and found that ACL-injured patients were twice as likely to have relatives who had sustained an ACL injury compared with the controls (adjusted odds ratio = 2.00; 95% confidence interval, 1.19–3.33).
1 Olsen OE, Myklebust G, Engebretsen L, et al. Relationship between floor type and risk of ACL injury in team handball. Scand J Med Sci Sports. 2003;13:299-304.
2 Torg JS, Stilwell G, Rogers K. The effect of ambient temperature on the shoe-surface interface release coefficient. Am J Sports Med. 1996;24:79-82.
3 Orchard J, Seward H, McGivern J, et al. Rainfall, evaporation and the risk of non-contact anterior cruciate ligament injury in the Australian Football League. Med J Aust. 1999;170:304-306.
4 Heidt RS, Dormer SG, Cawley PW, et al. Differences in friction and torsional resistance in athletic shoe-turf surface interfaces. Am J Sports Med. 1996;24:834-842.
5 Scranton PE, Whitesel JP, Powell JW, et al. A review of selected non-contact anterior cruciate ligament injuries in the National Football League. Foot Ankle Int. 1997;18:772-776.
6 Lambson R, Barnhill B, Higgins R. Football cleat design and its effect on anterior cruciate ligament injuries. Am J Sports Med. 1996;24:155-159.
7 Decoster LC, Vailas JC. Functional anterior cruciate ligament bracing: a survey of current brace prescription patterns. Orthopedics. 2003;26:701-706. discussion, 706
8 Teitz C, Hermanson B, Kronmal R, et al. Evaluation of the use of braces to prevent injury to the knee in collegiate football players. J Bone Joint Surg Am. 1987;69:2-8.
9 Rovere G, Haupt H, Yates C. Prophylactic knee bracing in college football. Am J Sports Med. 1987;15:111-116.
10 Sitler M, Ryan J, Hopkinson W, et al. The efficacy of a prophylactic knee brace to reduce knee injuries in football. A prospective randomized study at West Point. Am J Sports Med. 1994;18:310-315.
11 Albright J, Powell J, Smith W, et al. Medial collateral ligament knee sprains in college football. Am J Sports Med. 1994;22:12-18.
12 Albright JP, Saterbak A, Stokes J. Use of knee braces in sport. Current recommendations. Sports Med. 1995;20:281-301.
13 Najibi S, Albright JP. The use of knee braces, part 1: prophylactic knee braces in contact sports. Am J Sports Med. 2005;33:602-611.
14 Swirtun LR, Jansson A, Renstrom P. The effects of a functional knee brace during early treatment of patients with a nonoperated acute anterior cruciate ligament tear: a prospective randomized study. Clin J Sport Med. 2005;15:299-304.
15 Kocher MS, Sterett WI, Briggs KK, et al. Effective functional bracing on subsequent knee injury in ACL deficient professional skiers. J Knee Surg. 2003;16:87-92.
16 Risberg MA, Holm I, Steen H, et al. The effect of knee bracing after anterior cruciate ligament reconstruction. A prospective, randomized study with two years’ follow-up. Am J Sports Med. 1999;29:76-83.
17 McDevitt ER, Taylor DC, Miller MD, et al. Functional bracing after anterior cruciate ligament reconstruction: a prospective, randomized, multicenter study. Am J Sports Med. 2004;32:1887-1892.
18 Lephart SM, Kocher MS, Fu FH, et al. Proprioception following anterior cruciate ligament reconstruction. J Sport Rehabil. 1992;1:188-196.
19 Birmingham TB, Kramer JF, Kirkley A, et al. Knee bracing after ACL reconstruction: effects on postural control and propriception. Med Sci Sports Exerc. 2001;33:1253-1258.
20 Beynnon BD, Good L, Risbert MA. The effect of bracing on proprioception of knees with anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2002;32:11-15.
21 Risberg MA, Beynnon BD, Peura GD, et al. Proprioception after anterior cruciate ligament reconstruction with and without bracing. Knee Surg Sports Traumatol Arthrosc. 1999;7:303-309.
22 Duffey ML, Martin DF, Cannon DW, et al. Etiologic factors associated with anterior knee pain in distance runners. Med Sci Sports Exerc. 2000;32:1825-1832.
23 Heiderscheit BC, Hamill J, Van Emmerik RE. Q-angle influences on the variability of lower extremity coordination during running. Med Sci Sport Exerc. 1999;31:1313-1319.
24 Heiderscheit BC, Hamill J, Caldwell GE. Influence of Q-angle on lower-extremity running kinematics. J Orthop Sports Phys Ther. 2000;30:271-278.
25 Shambaugh JP, Klein A, Herbert JH. Structural measures as predictors of injury in basketball players. Med Sci Sports Exerc. 1991;23:522-527.
26 Grelsamer RP, Dubey A, Weinstein CH. Men and women have similar Q angles: a clinical and trigonometric evaluation. J Bone Joint Surg Br. 2005;87:1498-1501.
27 Gray J, Taunton J, McKinzie D, et al. A survey of injuries to the anterior cruciate ligament of the knee in female basketball players. Int J Sports Med. 1985;6:314-316.
28 Myer GD, Ford KR, Hewett TE. The effects of gender on quadriceps muscle activation strategies during a maneuver that mimics a high ACL injury risk position. J Electromyogr Kinesiol. 2005;15:181-189.
29 Guerra JP, Arnold MJ, Gajdosik RL. Q angle: effects of isometric quadriceps contraction and body position. J Orthop Sports Phys Ther. 1994;19:200-204.
30 Ireland ML, Ballantyne BT, Little K, et al. A radiographic analysis of the relationship between the size and shape of the intercondylar notch and anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2001;9:200-205.
31 LaPrade R, Burnett Q. Femoral intercondylar notch stenosis and correlation to anterior cruciate ligament injuries. Am J Sports Med. 1994;22:198-203.
32 Lombardo S, Sethi PM, Starkey C. Intercondylar notch stenosis is not a risk factor for anterior cruciate ligament tears in professional male basketball players: an 11-year prospective study. Am J Sports Med. 2005;33:29-34.
33 Lund-Hassen H, Gannon J, Engebretsen L, et al. Intercondylar notch width and risk of ACL rupture in female varisty team handball players. A case control study. Acta Orthop Scand. 1994;65:529-532.
34 Norwood LA, Cross MJ. The intercondylar shelf and the anterior cruciate ligament. Am J Sports Med. 1977;5:171-176.
35 Palmer I. On the injuries to the ligaments to the knee joint. A clinical study. Acta Chir Scand. 53(suppl), 1938.
36 Schickendantz M, Weiker G. The predictive value of radiographs in the evaluation of unilateral and bilateral anterior cruciate ligament injuries. Am J Sports Med. 1993;21:110-113.
37 Shelbourne KD, Davis TJ, Klootwyk TE. The relationship between intercondylar notch width of the femur and the incidence of anterior cruciate ligament tears: a prospective study. Am J Sports Med. 1998;26:402-408.
38 Souryal TO, Freeman TR. Intercondylar notch size and anterior cruciate ligament injuries in athletes: a prospective study. Am J Sports Med. 1993;21:535-539.
39 Anderson AF, Lipscomb AB, Liudahl KJ, et al. Analysis of the intercondylar notch by computed tomography. Am J Sports Med. 1987;15:547-552.
40 Houseworth S, Mauro V, Mellon B, et al. The intercondylar notch in acute tears of the anterior cruciate ligament: a computer graphics study. Am J Sports Med. 1987;15:221-224.
41 Anderson AF, Dome DC, Gautam S, et al. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med. 2001;29:58-66.
41a Tillman MD, Smith KR, Bauer JA, et al. Differences in three intercondylar notch geometry indices between males and females: a cadaver study. Knee. 2002;9:41-46.
42 Charlton WP, St John TA, Ciccotti MG, et al. Differences in femoral notch anatomy between men and women: a magnetic resonance imaging study. Am J Sports Med. 2002;30:329-333.
43 Chandrashekar N, Slauterbeck J, Hashemi J. Sex-based differences in the anthropometric characteristics of the anterior cruciate ligament and its relation to intercondylar notch geometry. Am J Sports Med. 2005;33:1492-1498.
44 Muneta T, Takakuda K, Yamamoto H. Intercondylar notch width and its relation to the configuration and cross-sectional area of the anterior cruciate ligament. Am J Sports Med. 1997;25:69-72.
45 Rizzo M, Holler SB, Bassett FH. Comparison of males’ and females’ ratios of anterior-cruciate-ligament width to femoral-intercondylar-notch width: a cadaveric study. Am J Orthop. 2001;30:660-664.
46 Arendt E, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athletic Tr. 1999;34:86-92.
47 Myklebust G, Maehlum S, Holm I, et al. A prospective cohort study of anterior cruciate ligament injuries in elite Norwegian team handball. Scand J Med Sci Sports. 1998;8:149-153.
48 Wojtys EM, Huston LJ, Lindenfeld TN, et al. Association between the menstrual cycle and anterior cruciate ligament injuries in female athletes. Am J Sports Med. 1998;26:614-619.
49 Beynnon BD, Johnson RJ, Braun S, et al. The relationship between menstrual cycle phase and anterior cruciate ligament injury: a case-control study of recreational alpine skiers. Am J Sports Med. 2006;34:757-764.
50 Slauterbeck JR, Fuzie SF, Smith MP, et al. The menstrual cycle, sex hormones, and anterior cruciate ligament injury. J Athl Train. 2002;37:275-278.
51 Wojtys EM, Huston LJ, Boynton MD, et al. The effect of the menstrual cycle on anterior cruciate ligament injuries in women as determined by hormone levels. Am J Sports Med. 2002;30:182-188.
52 Wojtys EM, Huston LJ. The effect of the female menstrual cycle on lower extremity neuromuscular performance and anterior knee laxity. Anaheim, CA: American Academy of Orthopaedic Surgeons, 1999.
53 Belanger MJ, Moore DC, Crisco JJIII, et al. Knee laxity does not vary with the menstrual cycle, before or after exercise. Am J Sports Med. 2004;32:1150-1157.
54 Karageanes SJ, Blackburn K, Vangelos ZA. The association of the menstrual cycle with the laxity of the anterior cruciate ligament in adolescent female athletes. Clin J Sport Med. 2000;10:162-168.
55 Van Lunen BL, Roberts J, Branch JD, et al. Association of menstrual-cycle hormone changes with ACL laxity measurements. J Athl Train. 2003;38:298-303.
56 Heitz NA. Hormonal changes throughout the menstrual cycle and increased anterior cruciate ligament laxity in females. J Athl Train. 1999;343:144-149.
57 Deie M, Sakamaki Y, Sumen Y, et al. Anterior knee laxity in young women varies with their menstrual cycle. Int Orthop. 2002;26:154-156.
58 Shultz SJ, Kirk SE, Johnson ML, et al. Relationship between sex hormones and anterior knee laxity across the menstrual cycle. Med Sci Sports Exer. 2004;36:1165-1174.
59 Grana W, Moretz J. Ligamentous laxity in secondary school athletes. J Am Med Assoc. 1978;240:1975-1976.
60 Kalenak A, Morehouse C. Knee stability and knee ligament injuries. J Am Med Assoc. 1975;234:1143-1145.
61 Moretz J, Walters R, Smith L. Flexibility as a prediction of knee injuries in college football players. PSM. 1982;10:93-97.
62 Steiner M, Grana W, Chillag K, et al. The effect of exercise on anterior-posterior knee laxity. Am J Sports Med. 1986;14:24-29.
63 Liu S, Al-Shakin R, Panossian V, et al. Primary immunolocalization of estrogen progesterone target cells in the human anterior cruciate ligament. J Ortho Res. 1996;14:526-533.
64 Lovering RM, Romani WA. Effect of testosterone on the female anterior cruciate ligament. Am J Physiol Regul Integr Comp Physiol. 2005;289:R15-R22.
65 Liu SH, Al-Shaikh RA, Panossian V, et al. Estrogen affects the cellular metabolism of the anterior cruciate ligament: a potential explanation for female athletic injury. Am J Sports Med. 1997;25:704-709.
66 Slauterbeck JR, Clevenger C, Lundberg W, et al. Estrogen level alters the failure load of the rabbit anterior cruciate ligament. J Orthop Res. 1999;17:405-408.
67 Seneviratne AE, Williams RJ, Rodeo SA, et al. The effect of estrogen on ovine anterior cruciate ligament fibroblasts: cell proliferation and collagen synthesis. Am J Sports Med. 2004;32:1613-1618.
68 Strickland SM, Belknap TW, Turner SA, et al. Lack of hormonal influences on mechanical properties of sheep knee ligaments. Am J Sports Med. 2003;31:210-215.
69 Arendt E, Agel J, Dick R. Profile of the ACL injured athlete. A pilot study. In: Griffin LY, editor. Prevention of noncontact ACL injuries. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2001:77-86.
70 Posthuma BW, Bass MJ, Bull SB, et al. Detecting changes in function ability in women with premenstrual syndrome. Am J Obstet Gynecol. 1987;15:275-278.
71 Zimmerman E, Parlee MB. Behavioral changes associated with the menstrual cycle: an experimental investigation. J Appl Sociol Psychol. 1973;3:335-344.
72 Janse de Jonge XA. Effects of the menstrual cycle on exercise performance. Sports Med. 2003;33:833-851.
73 Lebrun CM, Rumball JS. Relationship between athletic performance and menstrual cycle. Curr Womens Health Rep. 2001;1:232-240.
74 Materson G. The impact of menstrual phases on anaerobic power performance in collegiate women. J Strength Cond Res. 1999;13:325-329.
75 Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing non-contact ACL injuries: a review of the Hunt Valley II Meeting, January 2005. Am J Sports Med. 2006;34:1512-1532.
76 Boden BP, Dean GS, Feagin JA. Mechanism of anterior cruciate ligament injury. Orthopedics. 2000;23:573-578.
77 Malone TR. Relationship of gender in anterior cruciate ligament (ACL) injuries of NCAA division I basketball players. J South Orthop Assoc. 1992;2:36-39.
78 Myklebust G, Makhlum S, Emgebretsen L, et al. Registration of cruciate ligament injuries in Norwegian top level team handball. A prospective study covering two seasons. Scand J Med Sci Sports. 1997;7:289-292.
79 Dufek JS, Bates BT. The evaluation and prediction of impact forces during landings. Med Sci Sports Exerc. 1990;22:370-377.
80 Ferretti A, Papandrea P, Conteduca F, et al. Knee ligament injuries in volleyball players. Am J Sports Med. 1992;20:203-207.
81 Griffis D, Vequist S, Yearout K, et al. Injury prevention of the anterior cruciate ligament. Abstract at the American Orthopaedic Society for Sports Medicine 15th Annual Meeting, No. 13, Traverse City, MI, 1989. 1989.
82 Markolf KL, Burchfield DM, Shapiro MM, et al. Combined knee-loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13:930-935.
83 Markolf K, Gorek J, Kalzo M, et al. Direct measurement of resistant forces in the anterior cruciate ligament. J Bone Joint Surg Am. 1990;72:557-567.
84 Ettlinger C, Johnson R, Shealy J. A method to help reduce the risk of serious knee sprains incurred in alpine skiing. Am J Sports Med. 1995;23:531-537.
85 Johnson RJ. The ACL injury in female skiers. In: Griffin LY, editor. Prevention of noncontact ACL injuries. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2001:107-112.
85a Garrett WEJr. Non-contact ACL injuries in female athletes: risk factors and biomechanical considerations. Instructional Course Lecture Series, 78th Annual American Academy of Orthopaedic Surgeons Meeting. Feb 9, 2003. New Orleans, LA
86 DeMorat G, Weindhold P, Blackburn T, et al. Aggressive quadriceps loading can induce noncontact anterior cruciate ligament injury. Am J Sports Med. 2004;32:477-483.
87 Markolf KL, Graff-Radford A, Amstutz HC. In vivo knee stability. A quantitative assessment using an instrumented clinical testing apparatus. J Bone Joint Surg Am. 1978;60:664-674.
88 Bryant JT, Cooke TD. Standardized biomechanical measurement for varus-valgus stiffness and rotation in normal knees. J Orthop Res. 1988;6:863-870.
89 Such CH, Unsworth A, Wright V, et al. Quantitative study of stiffness in the knee joint. Ann Rheum Dis. 1975;34:286-291.
90 Wojtys EM, Ashton-Miller JA, Huston LJ, et al. A gender-related difference in the contribution of the knee musculature to sagittal-plane shear stiffness in subjects with similar knee laxity. J Bone Joint Surg Am. 2002;84A:10-16.
91 Huston LJ, Wojtys EM. Neuromuscular performance characteristics in elite female athletes. Am J Sports Med. 1996:427-436.
92 Chappell JD, Yu B, Kirkendall DT, et al. A comparison of knee kinetics between male and female recreational athletes in stop-jump task. Am J Sports Med. 2002;30:261-267.
93 Colby SM, Francisco A, Kirkendall DT. Electromyographic and kinematic analysis of cutting maneuvers. Implications for anterior cruciate ligament injury. Am J Sports Med. 2000;28:1234-1240.
94 Decker MJ, Torry MR, Wyland DJ, et al. Gender differences in lower extremity kinematics, kinetics, and energy absorption during landing. Clin Biomech (Bristol, Avon). 2003;18:662-669.
95 Huston LJ, Vibert B, Ashton-Miller JA, et al. Gender differences in knee angle when landing from a drop-jump. Am J Knee Surg. 2001;14:215-219.
96 Malinzak RA, Colby SM, Kirkendall DT, et al. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin Biomech. 2001;16:438-445.
97 Teitz CC. Video analysis of ACL injuries. In: Griffin LY, editor. Prevention of noncontact ACL injuries. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2001:93-96.
98 Yu B, McClure SB, Onate JA, et al. Age and gender effects on knee motion patterns of youth soccer players in a stop-jump task. Am J Sports Med. 2005;33:1356-1364.
99 Hewett TE, Stroupe AL, Nance TA, et al. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24:765-773.
100 Fagenbaum R, Darling WG. Jump landing strategies in male and female college athletes and the implications of such strategies for anterior cruciate ligament injury. Am J Sports Med. 2003;31:233-240.
101 Hewett TE, Myer GD, Ford KR. Decrease in neuromuscular control about the knee with maturation in female athletes. J Bone Joint Surg Am. 2004;86:1601-1608.
102 McLean SG, Walker K, Ford KR, et al. Evaluation of a two dimensional analysis method as a screening and evaluation tool for anterior cruciate ligament injury. Br J Sports Med. 2005;39:355-362.
103 McLean SG, Huang X, Su A, et al. Sagittal plane biomechanics cannot injure the ACL during sidestep cutting. Clin Biomech (Bristol, Avon). 2004;19:828-838.
104 McLean SG, Lipfert SW, van den Bogert AJ. Effect of gender and defensive opponent on the biomechanics of sidestep cutting. Med Sci Sports Exerc. 2004;36:1008-1016.
105 Pollard CD, Davis IM, Hamill J. Influence of gender on hip and knee mechanics during a randomly cued cutting maneuver. Clin Biomech (Bristol, Avon). 2004;19:1022-1031.
106 Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes. Part 1: mechanisms and risk factors. Am J Sports Med. 2006;34:299-311.
107 Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33:492-501.
108 Kibler WB, Livingston B. Closed-chain rehabilitation for upper and lower extremities. J Am Acad Orthop Surg. 2001;9:412-421.
109 Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35:1745-1750.
110 Harner C, Paulos L, Greenwald A, et al. Detailed analysis of patients with bilateral anterior cruciate ligament injuries. Am J Sports Med. 1994;22:37-43.
111 Flynn RK, Pedersen CL, Birmingham TB, et al. The familial predisposition toward tearing the anterior cruciate ligament: a case control study. Am J Sports Med. 2005;33:23-28.
112 Souryal TO, Moore HA, Evans JP. Bilaterality in anterior cruciate ligament injuries: associated intercondylar notch stenosis. Am J Sports Med. 1988;5:449-454.