CHAPTER 21 Right hemicolectomy
Step 1. Surgical anatomy
♦ The ileocolic vascular pedicle of the superior mesenteric artery must be isolated and divided. If the resection is performed for malignancy, it is important to divide this pedicle close to the root of the mesentery.
♦ The mesenteric vessels should be divided up to and including the right branch of the middle colic artery for a formal right hemicolectomy.
Step 2. Preoperative considerations
Patient preparation
♦ A preoperative colonoscopy will identify the lesion to be removed. The endoscopist should tattoo the lesion in order to allow the operating surgeon to then identify a mucosal lesion from the serosal side of the bowel, and thus remove the appropriate specimen.
♦ An abdominal computed tomography (CT) scan may also help localize the lesion to be removed as well as provide an anatomic overview of the patient’s abdomen.
♦ A full preoperative metastatic workup should be performed for malignant lesions.
♦ Patients should receive preoperative bowel preparation the day before surgery (e.g., GoLYTELY, HalfLytely, phospho soda, magnesium citrate).
♦ Within 1 hour of skin incision, intravenous (IV) antibiotics must be administered.
♦ Indications for laparoscopic right colectomy are the same as those for open colectomy and include colonic polyps, Crohn disease, colon cancer, and so on.
♦ Oncologic results have been shown to be equivalent between laparoscopic and open surgery for colon cancer.
♦ There are some contraindications to laparoscopic colectomy, which include the following:
Equipment and instrumentation
♦ Veress needle, 12-mm port, 5-mm ports.
♦ A 5-mm or 10-mm, 30-degree camera (a zero-degree camera can also be used).
♦ 5-mm LigaSure device (Covidien, Mansfield, Massachusetts) or Harmonic scalpel (Ethicon, Somerville, New Jersey).
♦ Endo GIA (Autosuture, Covidien) roticulating stapler with gastrointestinal (3.5-mm staple height) cartridge load for division of colon; a cartridge (2.5-mm staple height) for division of ileum and a vascular cartridge (2-mm staple height) can be used for division of ileocolic vascular pedicle instead of using one of the cutting or sealing devices LigaSure or Harmonic scalpel.
♦ An Endoloop (Ethicon, Somerville, New Jersey) should be available (although not necessarily opened) in case of the need for rapid vascular control.
♦ Laparoscopic suction/irrigator.
♦ Handheld linear cutting gastrointestinal stapler (3.5-mm staple height).
♦ Handheld linear non-cutting TA gastrointestinal stapler (3.5- to 4.8-mm staple height).
Step 3. Operative steps
Access and port placement
♦ A Veress needle is inserted in the left upper quadrant and pneumoperitoneum is established with carbon dioxide to a pressure of approximately 15 mmHg.
♦ A 12-mm port is inserted in the supraumbilical region, and a 30-degree camera is introduced.
♦ The abdomen is inspected for metastatic disease, especially focusing on the liver.
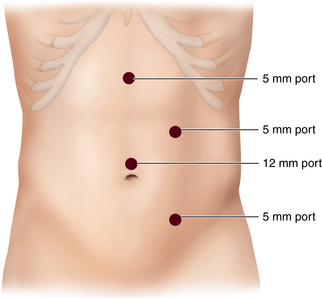
♦ Insert a 5-mm port in the left lower quadrant, left upper quadrant, and subxiphoid region under direct vision (Figure 21-1).
Dissection
♦ Adhesions, if present, are gently taken down using sharp dissection, and the abdomen is further explored for metastasis and resectability.
♦ The patient is positioned in Trendelenburg with the left side down.
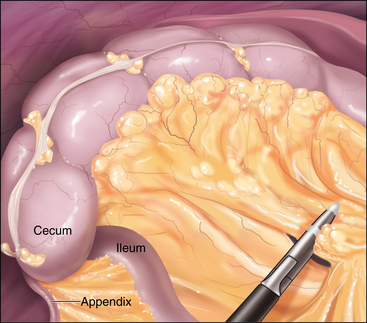
♦ Dissection begins by identifying the appendix, cecum, and terminal ileum. The assistant provides medial traction of the cecum.
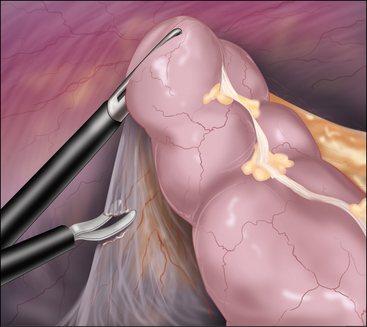
♦ The right colon lateral attachments are then taken down. Identify and sharply incise the right white line of Toldt, beginning at the cecum, taking care to identify and avoid the right ureter (Figure 21-2).
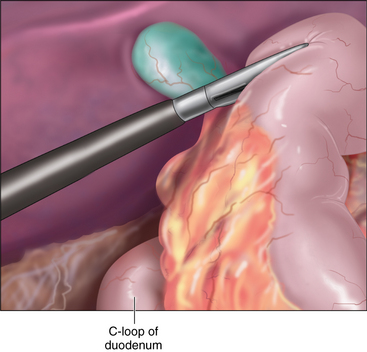
♦ The sharp dissection continues up to and around the hepatic flexure while the assistant is providing medial traction on the right colon. The patient is placed in reverse Trendelenburg to facilitate exposure. The duodenum is protected at all times. When the right colon is retracted medially, the duodenum is identified (Figure 21-3).
Division of bowel and vascular pedicle
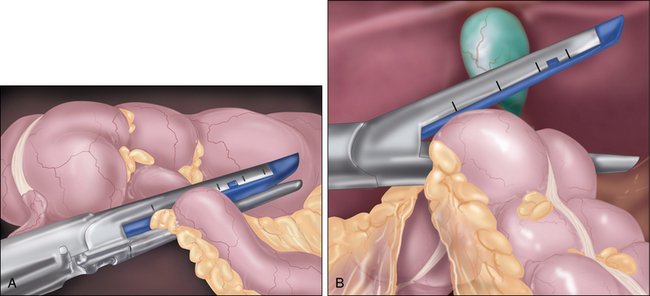
♦ Once the right colon is medialized, divide the terminal ileum using a laparoscopic stapler (Figure 21-4A).
♦ It is best to divide the mesentery using a LigaSure or ultrasonic coagulator to maintain hemostasis while minimizing thermal spread. The ileocolic and right colic vessels may be divided with these devices. Ensure proximal ligation of vessels for malignant disease to encompass the maximum number of lymph nodes in the specimen (Figure 21-5).
♦ Isolate and clear the distal resection line on the transverse colon. Divide the colon with a laparoscopic stapler (Figure 21-4B).
Specimen removal
♦ The specimen is placed in the right upper quadrant, and the patient is placed in the neutral position.
♦ Either the subxiphoid or the umbilical port site is used for specimen extraction and extracorporeal anastomosis.
♦ The port is removed and the site is extended for 4 cm vertically. A wound protector may be used at this point. When the specimen is removed, the proximal and distal segments of bowel are brought out through the wound.
Anastomosis
♦ A side-to-side, functional end-to-end anastomosis is performed with a handheld linear stapler GIA stapler, and the common enterotomy is closed with a TA stapler. The anastomosis is returned to the abdomen.
♦ The 4-cm incision is closed. Pneumoperitoneum is reestablished, and the abdomen is inspected for bleeding.
♦ All ports are removed under direct vision, irrigated, and closed.
Step 5. Pearls and pitfalls
♦ Move the camera and instruments around to achieve triangulation.
♦ Always know the location of the right ureter, duodenum, IVC, and stomach to avoid inadvertent injury.
♦ Upsize ports if necessary to accommodate cameras and staplers as needed.
♦ Closely visualize the abdomen for bleeding as pneumoperitoneum is being released.
. The Clinical Outcomes of Surgical Therapy Study Group: A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350;20:2050-2059.
Davies MM, Nelson H. Small bowel/colon resection. In: Zinner MJ, Ashley SW, editors. Maingot’s Abdominal Operations. 11th ed. New York: McGraw-Hill; 2007:1151-1167.
Larson DW, Nelson H. Laparoscopic colectomy for cancer. J Gastrointest Surg. 2004;8(5):636-642.