Chapter 58 Rheumatologic Disease in the Intensive Care Unit
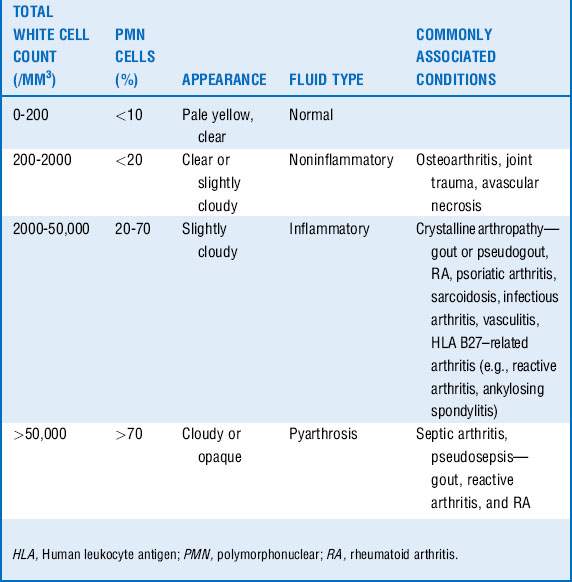
1 A critically ill patient is seen with an acute hot, swollen joint. What is the next step in management? What are the most common organisms found in a septic joint?
2 List the risk factors for the development of septic arthritis
5 What specific precautions should be taken when performing intubation in a patient with RA?
 Long-term use of corticosteroid
Long-term use of corticosteroid
 Severe peripheral joint deformities from RA
Severe peripheral joint deformities from RA
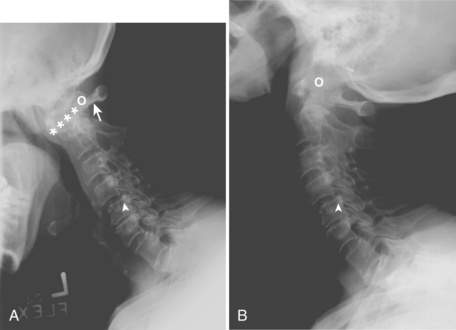
If clinical or radiographic evidence of subluxation exists and intubation is required, an anesthesiologist should be present during the procedure. In patients with AAS, subluxation is worsened with cervical flexion and reduced by cervical extension. Cricoarytenoid arthritis may also complicate endotracheal intubation. These patients may present with symptoms of tracheal pain, stridor, dysphonia, and shortness of breath (see Fig. 58-1).
6 What is scleroderma renal crisis (SRC)? When should this diagnosis be considered, and how is it confirmed?
 Clinical symptoms include headaches, visual disturbances from hypertensive retinopathy, seizures, encephalopathy, fever, general malaise, pulmonary edema. Less commonly, patients may have arrhythmias, myocarditis, and pericarditis.
Clinical symptoms include headaches, visual disturbances from hypertensive retinopathy, seizures, encephalopathy, fever, general malaise, pulmonary edema. Less commonly, patients may have arrhythmias, myocarditis, and pericarditis.
 Laboratory tests typically show an elevated creatinine level, microangiopathic hemolytic anemia, and thrombocytopenia. Urinalysis may show mild proteinuria, hematuria, and granular casts.
Laboratory tests typically show an elevated creatinine level, microangiopathic hemolytic anemia, and thrombocytopenia. Urinalysis may show mild proteinuria, hematuria, and granular casts.
7 Who is at risk for SRC, and what are risk factors indicating poor prognosis? What treatment should be initiated in SRC?
Poor prognosis for recovery from SRC is associated with the following:
9 How do you interpret a positive ANA test? What additional investigations should be ordered if there is a positive ANA test?
10 What clinical findings in a patient whose condition is deteriorating would prompt the consideration of SLE?
11 Describe antiphospholipid syndrome (APS)
APS is an acquired cause of hypercoagulability. Fifty percent of patients with APS have SLE. Recurrent venous and arterial thromboses and embolism are the hallmark of this syndrome. See Table 58-2.
Table 58-2 Clinical features and investigations of antiphospholipid syndrome
VDRL, Venereal Disease Research Laboratory.
12 What other laboratory evaluations may be useful in the diagnosis of other connective tissue disorders?
| Autoantibody | Disorder |
|---|---|
| Rheumatoid factor | RA (80%); SLE (10%); MCTD (50%-60%); Sjögren syndrome (80%-90%); infections; chronic liver and pulmonary disease and cryoglobulinemia (>40%) |
| Anti–cyclic citrulline peptide antibody | RA |
| ANA profile | |
MCTD, Mixed connective tissue disease; RA, rheumatoid arthritis; RNP, ribonuclear protein; SLE, systemic lupus erythematosus.
13 Patients with antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis frequently are seen in the intensive care unit (ICU). What diseases are associated with a positive ANCA test?
There are two forms of ANCA: cytoplasmic (c-ANCA) and perinuclear (p-ANCA). If the ANCA is positive, two target antigens should also be checked: myeloperoxidase (MPO) and serine proteinase-3 (PR3). See Box 58-1.
| C-ANCA | |
|---|---|
| PR3 positive: | |
ANCA, Antineutrophil cytoplasmic antibody; EBV, Epstein-Barr virus; MPO, myeloperoxidase; PR3, serine proteinase-3; RA, rheumatoid arthritis; SLE, systemic lupus erythematosus.
14 Diffuse alveolar hemorrhage (DAH) is a common presentation to the ICU. What are the clinical features? What are the common autoimmune conditions associated with DAH?
The common autoimmune diseases presenting with DAH include the following:
15 A patient with RA comes to the ICU with severe shortness of breath. Describe the different pulmonary causes
Pulmonary complications from RA account for 10% to 20% of all mortality.
 Parenchymal involvement: interstitial lung disease, bronchiolitis obliterans with organizing pneumonia, rheumatoid nodules
Parenchymal involvement: interstitial lung disease, bronchiolitis obliterans with organizing pneumonia, rheumatoid nodules
 Airway involvement: upper airway obstruction, obstructive sleep apnea, bronchiolitis (obliterative), bronchiectasis, Caplan syndrome, cricoarytenoid arthritis
Airway involvement: upper airway obstruction, obstructive sleep apnea, bronchiolitis (obliterative), bronchiectasis, Caplan syndrome, cricoarytenoid arthritis
 Vascular involvement: pulmonary hypertension, pulmonary vasculitis
Vascular involvement: pulmonary hypertension, pulmonary vasculitis
 Pleural involvement: pleural effusion, empyema, bronchopleural fistula or pyopneumothorax, chyliform effusions, lung entrapment
Pleural involvement: pleural effusion, empyema, bronchopleural fistula or pyopneumothorax, chyliform effusions, lung entrapment
 Drug-related lung toxicity: methotrexate, leflunomide, tumor necrosis factor (TNF) inhibitors, gold salts, and D-penicillamine
Drug-related lung toxicity: methotrexate, leflunomide, tumor necrosis factor (TNF) inhibitors, gold salts, and D-penicillamine
 Infections: pneumonia, bronchiectasis, empyema, infected nodules
Infections: pneumonia, bronchiectasis, empyema, infected nodules
16 An elderly woman comes to the ICU with fever of unknown origin, an elevated ESR, headaches, disorientation, and weakness. What rheumatologic condition should not be missed?
 Cranial symptoms: headaches, scalp tenderness, jaw claudication, diplopia, blindness, diminished temporal artery pulse, and stroke
Cranial symptoms: headaches, scalp tenderness, jaw claudication, diplopia, blindness, diminished temporal artery pulse, and stroke
 Polymyalgia rheumatica (PMR): gradual or acute onset of symmetric stiffness and pain in proximal muscle groups such as shoulders, hips, thighs, and neck
Polymyalgia rheumatica (PMR): gradual or acute onset of symmetric stiffness and pain in proximal muscle groups such as shoulders, hips, thighs, and neck
 Combination of PMR and cranial symptoms
Combination of PMR and cranial symptoms
 Abdominal symptoms: upper back pain, chest pain, dysphagia, dyspnea, superior vena cava syndrome due to thoracic aorta aneurysm or dissection; mesenteric ischemia
Abdominal symptoms: upper back pain, chest pain, dysphagia, dyspnea, superior vena cava syndrome due to thoracic aorta aneurysm or dissection; mesenteric ischemia
 Systemic symptoms: weight loss, fevers, fatigue, and malaise
Systemic symptoms: weight loss, fevers, fatigue, and malaise
17 Describe important side effects of biologic agents, such as TNF-α antagonists (e.g., etanercept, infliximab, adalimumab, certolizumab, and golimumab) that should be considered in an acutely ill ICU patient
 Reactivation of latent and miliary tuberculosis (TB)
Reactivation of latent and miliary tuberculosis (TB)
 Listeriosis with symptoms of meningoencephalitis or septicemia
Listeriosis with symptoms of meningoencephalitis or septicemia
 Disseminated fungal diseases such as histoplasmosis and coccidioidomycosis
Disseminated fungal diseases such as histoplasmosis and coccidioidomycosis
 Pneumocystis carinii (jirovecii) pneumonia (PCP)
Pneumocystis carinii (jirovecii) pneumonia (PCP)
 Reactivation of hepatitis B virus and herpes zoster infection
Reactivation of hepatitis B virus and herpes zoster infection
Remember: Live vaccinations should not be administered to patients taking biologic agents.
18 What adverse events associated with short- and long-term steroid use can be present in patients in the ICU?
Box 58-2 Common acute and chronic adverse effects of glucocorticoids
| Acute | Chronic |
|---|---|
 Atypical presentations of community-acquired and opportunistic infections
Atypical presentations of community-acquired and opportunistic infections
 Osteoporosis-associated fractures occurring with minor trauma
Osteoporosis-associated fractures occurring with minor trauma
 Osteonecrosis of large joints especially the hips, knees, ankles, and shoulders
Osteonecrosis of large joints especially the hips, knees, ankles, and shoulders
 Proximal muscle weakness due to steroid-induced myopathy
Proximal muscle weakness due to steroid-induced myopathy
 Higher risk of adverse cardiovascular and cerebrovascular disease
Higher risk of adverse cardiovascular and cerebrovascular disease
19 What precautions should be undertaken when admitting a patient taking long-term low-dose steroids to the ICU for an acute illness?
20 What are the sinister signs of back pain? What causes of back pain should not be missed in a critically ill patient?
 Unexplained weight loss, night sweats, fevers, chills
Unexplained weight loss, night sweats, fevers, chills
 Back pain that wakes patient from sleep
Back pain that wakes patient from sleep
 Increasing or persistent back pain despite analgesia and rest
Increasing or persistent back pain despite analgesia and rest
 Immunocompromised patient or intravenous drug abuse
Immunocompromised patient or intravenous drug abuse
 Bowel or bladder incontinence or saddle anesthesia
Bowel or bladder incontinence or saddle anesthesia
21 What are the causes of central nervous system (CNS) vasculitis? What specific investigations should be performed?
23 In the ICU, patients are seen acutely with an elevated creatine kinase (CK) level. What is the differential of an elevated CK level?
 Drug and toxin induced: statins, colchicine, ethanol, cocaine, antimalarials, corticosteroid-induced myopathy, barbiturates, zidovudine
Drug and toxin induced: statins, colchicine, ethanol, cocaine, antimalarials, corticosteroid-induced myopathy, barbiturates, zidovudine
 Infectious myositis: bacterial, viral, fungal, mycobacterial, or parasitic
Infectious myositis: bacterial, viral, fungal, mycobacterial, or parasitic
 Endocrine disorders: hypothyroidism, hyperthyroidism, acromegaly, Cushing or Addison disease
Endocrine disorders: hypothyroidism, hyperthyroidism, acromegaly, Cushing or Addison disease
 Metabolic myopathies: glycogen storage or lipid metabolism disorders, electrolyte disorders
Metabolic myopathies: glycogen storage or lipid metabolism disorders, electrolyte disorders
 Miscellaneous: seizures, malignant hyperthermia, motor neuron disease, rhabdomyolysis, organ failure
Miscellaneous: seizures, malignant hyperthermia, motor neuron disease, rhabdomyolysis, organ failure
 Autoimmune or rheumatologic disorders: PM or dermatomyositis (DM), PMR, systemic vasculitis, sarcoidosis, inflammatory arthritides
Autoimmune or rheumatologic disorders: PM or dermatomyositis (DM), PMR, systemic vasculitis, sarcoidosis, inflammatory arthritides
24 What are the clinical signs and symptoms that suggest an inflammatory myopathy? What other investigations may be helpful in diagnosing an inflammatory myopathy?
Key Points Rheumatologic Emergencies in the Intensive Care Unit
1. An acute swollen joint indicates septic arthritis until proved otherwise. Crystal-induced arthropathy and septic arthritis can occur simultaneously in a joint.
2. Patients with severe peripheral RA are at higher risk for spinal cord compression from AAS during intubation. Beware of cricoarytenoid obstruction also occurring in these patients.
3. Prompt treatment with an ACEi should be initiated in patients with SRC.
4. Patients taking biologic medications are at a higher risk for typical bacterial infections and atypical infections such as reactivation of TB, hepatitis B, herpes zoster, PCP, listeriosis, and disseminated fungal infections.
5. In a patient in the ICU who is seen with multiorgan failure or a clinical picture resembling fulminant sepsis, consider the diagnosis of SLE or vasculitis.
1 Corwell B.N. The emergency department evaluation, management and treatment of back pain. Emerg Med Clin N Am. 2010;28:811–839.
2 Denton C.P., Lapadula G., Mouthon L., et al. Renal complications and scleroderma renal crisis. Rheumatology. 2009;48:iii32–iii35.
3 Hajj-Ali R.A. Primary angiitis of the central nervous system: differential diagnosis and treatment. Best Pract Res Clin Rheumatol. 2010;24:413–426.
4 Hoffman G.S., Specks U. Antineutrophil cytoplasmic antibodies (ANCA). Arthritis Rheum. 1998;41:1521–1537.
5 Jacobs J.W.G., Bijlsma J.W.J. Glucocorticoid therapy. Firestein G.S., Budd R.C., Harris E.D., et al, eds. Kelley’sTextbook of Rheumatology, 8th ed, 1. Philadelphia: Saunders, 2009;863–881.
6 Janka G. Hemophagocytic syndromes. Blood Rev. 2007;21:245–253.
7 Lara A.R., Schwarz M.I. Diffuse alveolar hemorrhage. Chest. 2010;137:1164–1171.
8 Mathews C.J., Weston V.C., Jones A., et al. Bacterial septic arthritis in adults. Lancet. 2010;375:846–855.
9 Rendt K. Inflammatory myopathies: narrowing the differential diagnosis. Cleve Clin J Med. 2001;68:505–519.
10 Ruiz-Irastorza G., Crowther M., et al. Antiphospholipid syndrome. Lancet. 2010;376:1498–1509.
11 Sorokin R. Management of the patient with rheumatic disease going to surgery. Med Clin North Am. 1993;77:453–464.
12 Tassiulas I.O., Boumpas D.T. Clinical features and treatment of systemic lupus erythematosus. Firestein G.S., Budd R.C., Harris E.D., et al, eds. Kelley’sTextbook of Rheumatology, 8th ed, 1. Philadelphia: Saunders, 2009;1263–1300.
13 Tokunaga D., Hase H., Mikami Y., et al. Atlantoaxial subluxation in different intraoperative head position in patients with rheumatoid arthritis. Anesthesiology. 2006;104:675–679.