Chapter 45 Revision Total Elbow Arthroplasty in the Presence of Bone Deficiency
Background/aetiology
An alternative classification1 which is also helpful divides bone deficiency into: (1) deficient humeral or ulnar bone length; (2) compromised bone quality with ballooning of an intact cortex; and (3) periprosthetic fractures.
Presentation, investigations and treatment options
Surgical techniques and rehabilitation
Minimal bone loss
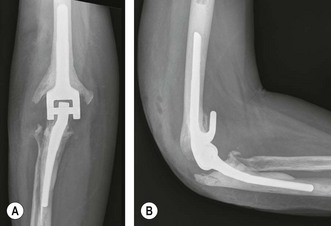
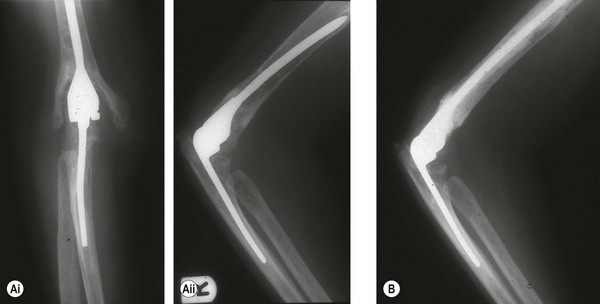
Minimal bone loss is most often encountered in cases of aseptic loosening where the arthroplasty has been in place for several years. The patient will usually present with intermittent symptoms of pain and discomfort around the elbow or pain that is precipitated by certain activities. Radiographs show loosening of either the humeral (Fig. 45.1), ulnar (Fig. 45.2) or both components. Humeral component loosening is thought to result from the posteriorly directed resultant forces that affect the elbow during flexion and extension,7 whereas at least some cases of ulnar component loosening result from ulnar component pistoning.8 Early revision prior to progressive bone loss is advised (Fig. 45.3).
Impaction bone grafting
This method of reconstruction is most useful where there has been extensive loss of medullary bone but with an intact cortical envelope (Fig. 45.4). It can also be used if there are small areas of cortical bone loss provided that these are controlled at the time of impaction grafting. This technique was described by Loebenberg et al9 who used a tube system to enable impaction of morcellized auto and allograft bone to restore the medullary bone while maintaining a central canal for insertion of the prosthesis.
Customized prostheses
Custom-made prostheses can be used for more extensive bone loss.10 With this technique it is important to obtain good-quality, size-marked radiographs together with radiographs of the contralateral elbow so that the manufacturer is able to produce an appropriately sized arthroplasty.
Autograft
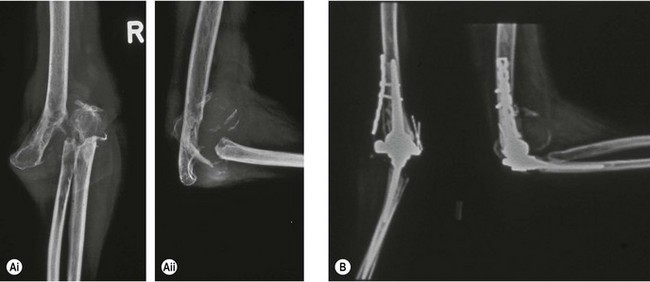
Autograft can be used effectively for small bone defects. Larger defects can be treated using fibular strut grafts (Fig. 45.5), although this increases morbidity. I have no personal experience of this technique and prefer to use allograft when dealing with these difficult problems.
Allograft
Lexer was the first to describe allografts in joint reconstruction.11 He transplanted fresh whole and partial joints removed at amputation into patients with joint deficiencies. Although he claimed a 50% success rate detailed follow-up was incomplete. No further publications on allografts appeared in the literature until the mid to late 1900s, when improvements in bone preservation resulted in renewed interest.12,13 Infection, graft non-union and fractures, however, remained serious complications.
Urbaniak and Black14 published their experience of ten partial and total cadaveric elbow reconstructions, nine of which were undertaken for trauma. The authors advised rigid internal fixation. Two years after insertion, however, degenerative changes were present in the joints, with two patients having allograft nonunion and two patients demonstrating elbow instability. One patient had a radial nerve palsy. A further study of 23 allograft elbow replacements followed for 20 years revealed seven allograft non-unions, six unstable elbows, four radial nerve palsies, three infections and one graft resorption.15 These results suggest that, although early benefit may be achieved by this technique, it is not a viable long-term option for elbow reconstruction. More recently allograft prosthesis joint combinations have been reported,16 some of which have been reinforced with strut grafts. This technique appears more successful and is my preferred option when bone loss is associated with significant cortical deficiency.
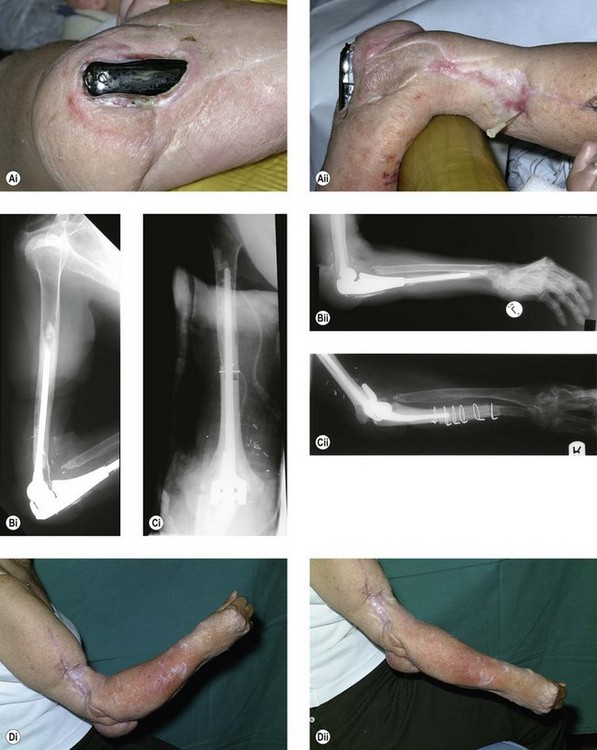
The second-stage procedure involves removal of the antibiotic beads and reconstruction of the joint with allograft and a total elbow arthroplasty. It is important at this stage to avoid any further resection of the patient’s bone. Any bone resection that is required to allow insertion of the allograft must be from the allograft otherwise the patient will end up with a more extensive bone deficit. Having approximately corrected the arm length a small step cut should be made in the allograft bone (Fig. 45.6) with a corresponding cut in the patient’s bone. This will help provide rotational stability when the reconstruction has been completed. The allograft is then prepared for insertion of the arthroplasty. Once complete the arthroplasty is cemented into the allograft (Fig. 45.7). This is undertaken outside the patient. The arthroplasty I use for these reconstructions is the Coonrad–Morrey replacement. The allograft prosthesis combination is then cemented into the patient with bone and wires placed around the junctional step cut zone in order to provide additional rotational stability (Fig. 45.8). Strut grafts can also be placed at the allograft host junction to provide additional strength (Fig. 45.9). These are wired in place. The wound is closed and a full-arm backslab applied with the elbow in extension. The arm is elevated in a Bradford sling and two doses of a third-generation cephalosporin are prescribed. The wound is inspected at 48 hours and provided that it is satisfactory the patient is allowed to gently mobilize the elbow.
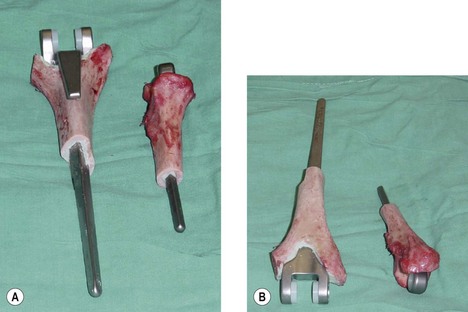
Figure 45.7 (A,B) Massive humeral and ulnar allograft prosthesis composite prior to insertion into the patient.

Figure 45.8 (A) Pre- and (B) post-operative radiographs following a massive allograft prosthesis reconstruction.
Mansat et al16 reported their experience of using allograft implant reconstructions in 13 patients reviewed after an average of 42 months. The Mayo Elbow Performance Score was excellent in four, good in three, fair in one and poor in five. Five revision procedures were performed, two allograft implants were removed and four patients developed deep infections. My own experience with humeral and ulnar allografts has been encouraging. To date I have managed to restore useful elbow function and have only removed one ulnar allograft for infection.
When osseous deficiency is predominantly on the ulnar side of the joint, Kamineni and Morrey17 have found strut allografts useful for reconstruction. They noted in 21 patients followed for an average of 4 years a mean Mayo Elbow Performance Score improvement of 34 points. Four osseous and four soft tissue complications were, however, noted in eight patients.
1 Morrey BF, Sanchez-Sotelo J. Revision of failed total elbow arthroplasty with osseous deficiency. In: Morrey BF, Sanchez-Sotelo J, editors. The Elbow and its Disorders. Philadelphia: WB Saunders/Elsevier; 2009:899-910.
2 Campbell WC. Incision for exposure of the elbow joint. Am J Surg. 1932;15:65-67.
3 Bryan RS, Morrey BF. Extensive posterior exposure of the elbow: A triceps sparing approach. Clin Orthop. 1982;166:188-192.
4 Wolfe SW, Ranawat CS. The osteo-anconeus flap: an approach for total elbow arthroplasty. J Bone Joint Surg (Am). 1990;72:684-688.
5 Shahane SA, Stanley D. A posterior approach to the elbow joint. J Bone Joint Surg (Br). 1999;81:1020-1022.
6 Steiger JU, Gschwend N, Bell S. GSB elbow arthroplasty: A new concept and six years experience. In: Kashiwagi D, editor. Elbow Joint. Amsterdam: Elsevier Science Publishers BV (Biomedical Division); 1985:285-294.
7 Amiss AA, Dowson D, Wright V. Elbow joint force predictions for some strenuous isometric actions. J Biomech. 1980;13:765-775.
8 Cheung EV, O’Driscoll SW. Total elbow prosthesis loosening caused by ulnar component pistoning. J Bone Joint Surg (Am). 2007;89:1269-1274.
9 Loebenberg MI, Adams RA, O’Driscoll SW, et al. Impaction grafting in revision total elbow arthroplasty. J Bone Joint Surg (Am). 2005;87:99-106.
10 Figgie HE, Inglis AE, Mow C. Total elbow arthroplasty in the face of significant bone stock or soft tissue losses: preliminary results of custom-fit arthroplasty. J Artroplasty. 1986;1:71-81.
11 Lexer E. Joint transplantations and arthroplasty. Surg Gynecol Obstet. 1925;60:782-809.
12 Gross AE, Silverstein EA, Falk J, et al. The allotransplantation of partial joints in the treatment of osteoarthritis of the knee. Clin Orthop. 1975;108:7-14.
13 Mankin HJ, Doppelt SH, Sullivan TR, et al. Osteoarticular and intercalary allograft transplantation in the management of malignant tumours of bone. Cancer. 1982;50:613-630.
14 Urbaniak JR, Black KE. Cadaveric elbow allografts. Clin Orthop. 1985;197:131-140.
15 Dean GS, Holliger EH, Urbaniak JR. Elbow allograft for reconstruction of the elbow with massive bone loss. Long term results. Clin Orthop Relat Res. 1997;341:12-22.
16 Mansat P, Adams RA, Morrey BF. Allograft-prosthesis composite for revision of catastrophic failure of total elbow arthroplasty. J Bone Joit Surg (Am). 2004;86:724-735.
17 Kamineni S, Morrey BF. Proximal ulnar reconstruction with strut allograft in revision total elbow arthroplasty. J Bone Joint Surg (Am). 2004;86:1223-1229.