CHAPTER 4 Respiratory support
Respiratory distress
The most common cause is hyaline membrane disease (HMD), also known as infant respiratory distress syndrome. The most important cause is infection (see pages 107–12).
The general principles of management include:
Continuous positive airway pressure (CPAP)
The benefits of CPAP include: a reduction in the need for intermittent positive-pressure ventilation (IPPV); decreased rate and severity of apnoea; increased chance of successful extubation; and decreased respiratory acidosis and oxygen requirements post-extubation.
Nasal intermittent positivepressure ventilation (NIPPV)
Surfactant
Surfactant administration
General
Assisted ventilation
Conventional mechanical ventilation (CMV)
To improve oxygenation (i.e. ↑ PaO2 ):
To improve ventilation and CO2 clearance (i.e. ↓ PaCO2 )
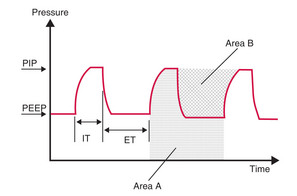
Obviously, changing Area A will change Area B. A compromise needs to be reached.
In general: adjust pressure or rate to alter PaCO2, and adjust FiO2 to alter PaO2.
Oxygen and CO2 targets
| Gestational age | SpO2 target range |
|---|---|
| <30 weeks | 85–92% |
| 30+ weeks | 90–94% |
SpO2 = oxygen saturation
Other settings
Some neonatologists use shorter ITs when ventilating babies with poorly compliant lungs.
Changes in respiratory status
Always respond to changes in respiratory status by:
Such changes in respiratory status may include:
Significant worsening ventilatory status should prompt examination and investigation for:
Volume-targeted ventilation
Volume-targeted ventilation is especially useful for small babies (<1250 g) who are more prone to the damaging effects of volutrauma and ventilator-induced lung injury.
High-frequency ventilation (HFV)
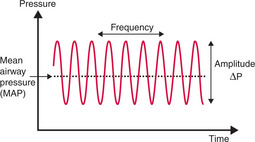
Optimal HFV is achieved by producing and maintaining optimal lung expansion. This is often referred to as a ‘highvolume strategy’. MAP is adjusted to optimise oxygenation. Increases in MAP lead to the recruitment of more alveoli and improved lung volume — this can be monitored by its effects on oxygenation, FiO2 and CXRs. The aim is to achieve maximum alveolar recruitment without overdistending the lungs.
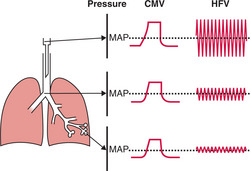
Ventilation is optimised by adjusting amplitude (ΔP) to achieve a desired PaCO2. The amplitude of each HFV ‘breath’ appears large compared with the PIPs used during CMV. However, the pressures are attenuated as they are transmitted down the ETT and airways so that the pressure oscillation is quite small at the lung periphery (Fig 4.3). Higher amplitude will increase tidal volume and improve CO2 clearance (i.e. decrease PaCO2).
Starting, changing and adjusting ventilation
Starting HFV
Changing from CMV to HFV
Fine-tuning or weaning HFV
Ventilation
To change the PaCO2 change the amplitude (or occasionally the frequency).
Oxygenation
If oxygenation remains poor (i.e. low oxygen saturations or PaO2):
Over-distension of the lungs with a MAP that is too high can impede venous return and/or pulmonary blood flow. This will decrease systemic perfusion and worsen oxygenation. If the baby is hypotensive or has a metabolic acidosis, the lungs may be over-inflated. Get a CXR. Try decreasing the MAP — does oxygenation improve?
Trigger ventilation modes
Each of these modes can be combined with volume-targeted ventilation as described above.
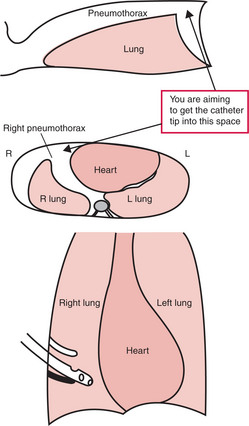
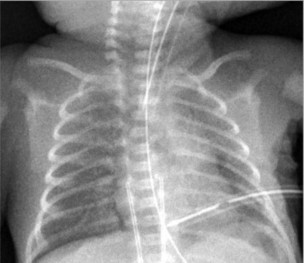
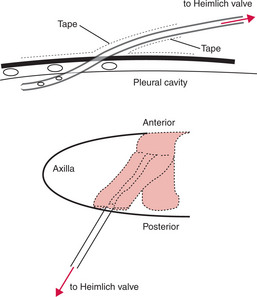
Pneumothorax (PTX)
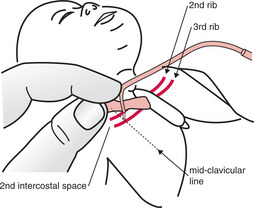
Needling the chest for a PTX
A procedure that is both diagnostic and therapeutic.
Site
Stay away from the heart, the internal mammary artery and the intercostal arteries — use either:
Insert the needle as close as possible to the upper edge of the lower rib.
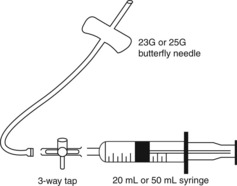
Equipment
Attach a 23G or 25G butterfly needle to a 3-way tap attached to a 20 mL or 50 mL syringe. (See Fig 4.4.)