Objectives
• Describe the priorities of the nursing assessment to detect acute kidney injury (AKI).
• Explain why elevation of blood urea nitrogen (BUN) and serum creatinine signal kidney dysfunction.
![]()
Be sure to check out the bonus material, including free self-assessment exercises, on the Evolve web site at http://evolve.elsevier.com/Urden/priorities/.
A history of acute kidney injury begins with a description stated in the patient’s own words, including the onset, location, duration, and factors or strategies that lessen or aggravate the problem.1 A careful history that explores symptoms fully is an essential component of the clinical assessment.
Predisposing factors for acute kidney dysfunction include the use of over-the-counter medicines, recent infections requiring antibiotic therapy, antihypertensive medicines, and any diagnostic procedures performed using a radiopaque contrast agent.2 The history may be significant for the recent onset of nausea and vomiting, appetite loss caused by taste changes (uremia often causes a metallic taste), or rapid fluid volume gains. For example, weight gain of more than 2 pounds per day, sleeping on additional pillows, and sitting in a chair to sleep are signals of volume overload and potential cardiopulmonary stress related to kidney dysfunction.
Physical Examination
In the critical care area, nursing assessment does not routinely include a full physical examination of the kidneys and urologic system. Although a thorough kidney assessment is rarely performed in the depth described in the following sections, the critical care nurse must be aware of how to perform one if needed in patients with kidney dysfunction.
Inspection
Nursing priorities for inspection of the patient with acute kidney injury focus on (1) bleeding, (2) volume depletion or overload, and (3) edema.
Bleeding
Visual inspection related to the kidneys focuses on the patient’s flank and abdomen. Kidney trauma is suspected if a purplish discoloration is present on the flank (Grey Turner’s sign) or near the posterior 11th or 12th ribs.1 Bruising, abdominal distention, and abdominal guarding may also signal kidney trauma or a hematoma around a kidney. Individuals who have experienced a traumatic injury are carefully assessed for signs of kidney trauma.
Volume
Fluid volume assessment begins with an inspection of the patient’s jugular neck veins as described in Chapter 11. The supine position facilitates normal jugular venous distention. An absence of distention (flat neck veins) indicates hypovolemia. Assessment continues with the head of the bed elevated 45 to 90 degrees.1 Fluid overload exists when the neck veins remain distended more than 2 cm above the sternal notch when the bed is at 45 degrees.3
Inspection of hand veins for venous distention when the hand is held in the dependent position is a component of volume assessment. Venous filling that takes longer than 5 seconds suggests hypovolemia. When the hand is elevated, the distention should disappear within 5 seconds. If distention does not disappear within 5 seconds after the hand is elevated, fluid overload is suspected.
To assess skin turgor, the examiner picks up skin over the forearm and then releases it. Normal elasticity and fluid status allow an almost immediate return to shape after the skin is released. In fluid volume deficit, the skin remains raised and does not return to its normal position for several seconds. Because of the loss of skin elasticity in older adults, skin turgor assessment is not an accurate fluid assessment for this age group.
Inspection of the oral cavity provides clues to fluid volume deficit as the mucous membranes of the mouth can become dry. However, mouth breathing and some medicines (e.g., antihistamines) can also dry the oral mucous membranes. The most accurate way to assess the oral cavity is to inspect the mouth using a tongue blade.3
Edema
Edema is the presence of excess volume in the interstitial space. Edema may develop in dependent areas of the body, such as the feet and legs of an ambulatory person or the sacrum of an individual confined to bed.
The presence of edema does not always indicate fluid volume overload. A loss of albumin from the vascular space can also cause peripheral edema. A key feature that identifies edema due to excess volume or hypoalbuminemia is that the edema does not reverse with elevation of the extremity.
Presence of pitting edema is assessed by application of fingertip pressure on the swollen area over a bony prominence, such as the ankles, pretibial areas (shins), and sacrum. If the indentation made by the fingertip does not disappear within 15 seconds, pitting edema exists. Pitting edema indicates increased interstitial volume, and it usually is not evident until significant weight gain has occurred.4 Edema also may appear in the hands, around the eyes, in the cheeks, and in dependent areas, such as the feet and sacrum. One way of estimating edema is by using a subjective 1 to 4 scale, with 1 indicating only minimal pitting and 4 indicating severe pitting (Table 19-1).1
TABLE 19-1
| RATING | APPROXIMATE EQUIVALENT |
| +1 | 2-mm depth |
| +2 | 4-mm depth (lasting up to 15 sec) |
| +3 | 6-mm depth (lasting up to 60 sec) |
| +4 | 8-mm depth (lasting longer than 60 sec) |
Auscultation
Nursing priorities in auscultation of the patient with acute kidney injury focus on (1) the heart, (2) blood pressure, and (3) the lungs.
Heart
Auscultation of the heart requires assessing the rate and rhythm and listening for extra heart sounds. Fluid overload is often accompanied by a third or fourth heart sound, which is auscultated with the bell of the stethoscope.1 Increased heart rate alone provides little information about fluid volume, but combined with a low blood pressure, it may suggest hypovolemia.
The heart is auscultated for the presence of a pericardial friction rub. A rub can best be heard at the third intercostal space to the left of the sternal border while the individual leans slightly forward.1 A pericardial friction rub indicates pericarditis, and it may result from uremia in a patient with kidney failure.
Blood Pressure
Blood pressure (BP) and heart rate (HR) changes are useful in assessing fluid volume deficit. In stable critically ill patients or in patients on a telemetry unit, orthostatic vital sign measurements provide clues to blood loss, dehydration, unexplained syncope, and the effects of some antihypertensive medications.4,5 A drop in systolic BP of 20 mm Hg or more, a drop in diastolic BP of 10 mm Hg or more, or a rise in pulse rate of more than 15 beats/min from lying to sitting or from sitting to standing indicate orthostatic hypotension. Box 19-1 describes how to assess for orthostatic hypotension.
Lungs
Lung assessment is essential in gauging fluid status. Crackles indicate fluid overload. Dyspnea with mild exertion, dyspnea at night that prevents sleeping in a flat position (orthopnea), or dyspnea that awakens the individual from sleep (paroxysmal nocturnal dyspnea) may indicate pooling of fluid in the lungs.
Percussion
Nursing priorities in percussion of the patient with acute kidney injury focus on (1) the kidneys and (2) the abdomen. Percussion is performed to detect pain in the area of a kidney or to determine excess accumulation of air, fluid, or solids around the kidneys. Neither palpation nor percussion of the kidneys is a routine part of a nursing assessment in critical care.
Kidneys
Percussion of a kidney is performed with the patient in a side-lying or sitting position, with the examiner’s hand placed over the costovertebral angle (lower border of the rib cage on the flank).1 Striking the back of the hand with the other fist produces a dull thud, which is normal. Pain may indicate kidney infection, or injury resulting from trauma. Traumatic injury to the kidneys should be assessed in the presence of a penetrating abdominal wound, with blunt abdominal trauma, or with a fractured pelvis or ribs.6,7 Mortality is increased when AKI is a complication of traumatic injury.7
Abdomen
Observation and percussion of the abdomen may help in assessing fluid status. Percussing the abdomen with the patient in the supine position generally yields a dull sound (solid bowel contents or fluid) or a hollow sound (gaseous bowel).1
Ascites, or excess fluid accumulation and distention of the abdominal cavity, is an important observation in determining fluid overload. Differentiating ascites from distortion caused by solid bowel contents is accomplished by producing a fluid wave. A fluid wave is elicited by exerting pressure to the abdominal midline while one hand is placed on the right or left flank.1,4 Tapping the opposite flank produces a wave in the accumulated fluid that can be felt under the examiner’s hands (Figure 19-1). Other signs of ascites include a protuberant, rounded abdomen and abdominal striae.1
Fluid Balance Assessment
Nursing priorities for the patient undergoing fluid balance assessment focus on (1) weight, (2) intake and output, and (3) hemodynamic monitoring.
Weight
In the critical care unit, weight is monitored daily and is an important vital signs measurement. Significant fluctuations in body weight over a 1- to 2-day period indicate fluid gains and losses. Rapid weight gains or losses of more than 2 pounds per day usually indicate fluid rather than nutritional factors. One liter of fluid equals 1 kg, or approximately 2.2 pounds.
The weight is obtained at the same time each day, with the patient wearing the same amount of clothing and using the same scale. The individual’s weight is of critical importance to the dialysis nurse caring for a patient with acute or chronic kidney failure. The differences in weight from day to day are used to calculate the amount of fluid to remove during a dialysis treatment.8
Intake and Output
Intake and output are monitored for every patient in the critical care unit and can be compared with the patient’s weight to more accurately evaluate fluid gains or losses. Urinary output plus insensible fluid losses (perspiration, stool, and water vapor from the lungs) can vary by 750 to 2400 mL/day. When intake exceeds output (e.g., excessive intravenous fluid, decreased urine output), a positive fluid balance exists.
Conversely, if output exceeds intake (e.g., fever, increased respiration, profuse sweating, vomiting, diarrhea, gastric suction, diuretic therapy), a negative fluid balance exists, and volume deficit results. During a 24-hour period, fever can increase skin and respiratory losses by as much as 75 mL per 1° F increase in temperature.
Individuals with acute kidney injury (AKI) often exhibit a decrease in urine output, or oliguria (<0.5 mL/kg/hr in adults). Although urine output is a sensitive indicator, kidney function cannot be accurately determined by urine output alone.
In the maintenance of daily records of intake and output, all gains or losses must be recorded. A standard list of the fluid volumes held in various containers (e.g., milk cartons, juice containers) expedites this process. Discussions about the importance of accurate intake and output with the patient and family or friends can improve the accuracy of intake and output volumes assessment.
Hemodynamic Monitoring
Body fluid status is accurately reflected in measurements of cardiovascular hemodynamics. Measurements such as central venous pressure (CVP), pulmonary artery occlusion pressure (PAOP), cardiac index (CI), and mean arterial pressure (MAP) provide a clear picture of the increases or decreases in vascular volume returning to and being ejected from the heart.9 Volume depletion and volume overload are monitored by use of central venous and arterial catheters, from which pressure measurements are obtained (Table 19-2).
TABLE 19-2
HEMODYNAMIC ASSESSMENT OF FLUID STATUS
| MEASUREMENT | VALUE WITH VOLUME DEPLETION | VALUE WITH VOLUME OVERLOAD |
| CVP (mm Hg) | <2 | >5 |
| PAOP (mm Hg) | <5 | >12 |
| CI (L/min/m2) | <2.2 | >4 |
| MAP | Decreased | Increased |
A central venous catheter often is inserted to evaluate fluid volume status and to measure the CVP. The CVP represents the filling pressure of the right atrium and is a measurement of right ventricular preload. The CVP changes with fluctuations in volume status. A normal CVP is 2 to 5 mm Hg.
If the patient has coexisting cardiopulmonary disease or if more information about hemodynamic function is required, a pulmonary artery catheter may be inserted. This catheter provides information about left ventricular filling pressures and cardiac output. The normal PAOP, or “wedge” pressure, is 5 to 12 mm Hg. In fluid volume excess, the PAOP increases. In fluid volume deficit, the PAOP is low.9 Pulmonary artery catheters are not routinely used to diagnose AKI but may be inserted when the patient is hemodynamically unstable from other conditions, such as heart failure, trauma, and sepsis.
Severe sepsis and septic shock are common precursors of AKI in the critically ill.10 Sepsis may present with hypotension, and prolonged hypotensive episodes increase risk of AKI and increase mortality.10 Hemodynamic monitoring with skillful nursing interpretation of trends provides essential information about the effectiveness of treatment.
Laboratory Assessment
Acute kidney injury often leads to electrolyte and acid-base imbalances that result from retention of metabolic waste products. Box 19-2 summarizes important aspects that should be considered during assessment. Retention of waste products and inability to buffer hydrogen ions contribute to the acidosis that occurs with kidney failure.
Lethargy, decreased attention or memory, coma, and confusion may result from electrolyte imbalance and retained waste products (see Box 19-2). Patients with kidney failure and the accompanying systemic increases in electrolytes, fluids, and nitrogenous waste products may exhibit a range of symptoms from restlessness and confusion to apathy and withdrawal.2 The speed of onset depends on how rapidly or slowly kidney failure progresses and alters homeostasis.
Serum Components
Blood Urea Nitrogen
Blood urea nitrogen is a by-product of protein and amino acid metabolism.11 The normal value for BUN is 5 to 25 mg/dL. This value rises as kidney function deteriorates.12 BUN elevation represents a decrease in the glomerular filtration rate (GFR) and resultant decrease in urea excretion. Elevations in the BUN correlate with the clinical manifestations of uremia.2 Many conditions result in BUN elevation, including dehydration,13 nephrotoxic drugs, excessive protein intake, and catabolism.11 The BUN level also rises from hematoma resorption, gastrointestinal bleeding, excessive licorice ingestion, or steroid or tetracycline therapy.
A decrease in the BUN level may indicate volume overload, liver damage, severe malnutrition from depleted protein stores, use of phenothiazines, or pregnancy.12
Creatinine
Creatinine is a by-product of muscle and normal cell metabolism, and it appears in serum in amounts generally proportional to the body muscle mass. Although slightly higher in males than females, the normal serum creatinine level is about 0.5 to 1.5 mg/dL.12 Creatinine is freely filtered by the glomerulus, easily excreted by the renal tubules, and minimally resorbed or secreted in the tubules.2 Creatinine levels are fairly constant and are affected by fewer factors than BUN. Consequently, the serum creatinine level is a more sensitive and specific indicator of kidney function.
Elevated creatinine values may occur in muscle growth disorders such as acromegaly with skeletal muscle destruction (e.g., rhabdomyolysis in a trauma patient), and with some medications that decrease creatinine removal (e.g., trimethoprim, cimetidine) in the absence of acute kidney injury.14
Another useful diagnostic parameter in acute kidney injury is the ratio of BUN to creatinine. The usual ratio is 10 to 1, and a change in the ratio may indicate kidney dysfunction.12,15
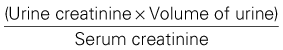
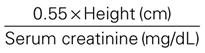
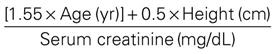
Creatinine Clearance
The creatinine clearance is a measure of how effectively the kidneys remove creatinine. Because of the relatively constant rate at which creatinine is produced and the nearly complete removal of creatinine by normal kidneys, the ability to remove (clear) creatinine from the blood is an indication of how well the glomeruli and tubules are working. The normal value for creatinine clearance is 110 to 120 mL/min; values less than 50 mL/min indicate significant kidney dysfunction. The creatinine clearance is best measured using a 12-hour or 24-hour urine collection and blood sample. In critical care, a smaller-volume urine specimen and blood sample is generally used.
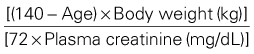
Creatinine clearance can also be estimated from the serum creatinine level.15 (Box 19-3). The estimated or calculated creatinine clearance is widely used to determine changes in drug dosing with kidney dysfunction because many medications are excreted by the kidneys.15 To adjust drug dosages, the critical care nurse should use the Cockcroft-Gault formula for estimating creatinine clearance.15,16
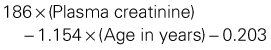
Osmolality
The serum osmolality reflects the concentration or dilution of vascular fluid and measures the dissolved particles in the serum. The normal serum osmolality is 275 to 295 mOsm/L.3 An elevated osmolality value indicates hemoconcentration or dehydration, and a decreased osmolality value indicates hemodilution or volume overload. Sodium accounts for 85% to 95% of the serum osmolality value. Multiplying the serum sodium level by 2 gives an estimate of the serum osmolality level in healthy indviduals.12 A more precise estimation of serum osmolality can be calculated from the following formula:
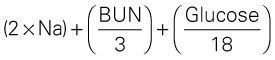
The calculated serum osmolality level is a useful tool during the wait for full laboratory results. Measured serum osmolality is a useful parameter in determining fluid replacement therapy for critically ill patients.
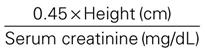
Anion Gap
The anion gap is a calculation of the difference between the measurable extracellular plasma anions (chloride and bicarbonate) and the measurable cations (sodium and potassium).3 In plasma, chloride is the predominant anion and sodium is the predominant cation. Generally, potassium is not included in the formula because the value is so small. This leaves the following equation for calculation of the anion gap:
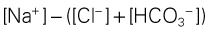
The normal anion gap is 8 to 16 mEq. The ‘gap’ represents the unmeasurable ions present in the extracellular fluid (phosphates, sulfates, ketones, lactate). An increased anion gap usually reflects overproduction of acid products and indicates metabolic acidosis.
Acute kidney injury and chronic kidney failure can increase the anion gap because of retention of acids and altered bicarbonate resorption. The anion gap is also increased in diabetic ketoacidosis (DKA) caused by ketone production. The measurement of a high anion gap is a rapid method for identifying acid-base imbalance but cannot be used to pinpoint the source of the acid-base disturbance specifically.
Hemoglobin and Hematocrit
The hemoglobin and hematocrit levels can indicate increases or decreases in intravascular fluid volume.11 An increase in the hematocrit value may occur with fluid volume deficit that produces hemoconcentration. Conversely, a decreased hematocrit can indicate fluid volume excess because of the dilutional effect of the extra fluid load.
Hemoglobin is decreased as a result of anemia, blood loss, liver damage, or hemolytic reactions.12 In individuals with acute kidney failure, anemia may occur early in the disease.
Urinalysis
Analysis of the urine provides excellent information about the patient’s kidney function and condition relative to fluids and electrolytes. Specific tests and abnormal indications are presented in Table 19-3.12,17–24 In many cases, urinalysis in the critically ill patient aids in locating the site of kidney damage or disease and therefore guides therapeutic management of the patient’s care.
TABLE 19-3
| TEST | NORMAL VALUE/RANGE | POSSIBLE CAUSES FOR INCREASED VALUES | ACIDOSIS |
| pH | 4.5-8.0 | ||
| Specific gravity | 1.003-1.030* | ||
| Osmolality | 300-1200 mOsm/kg | ||
| Protein | 30-150 mg/24 hr† | ||
| Sodium | 40-220 mEq/24 hr | ||
| Creatinine | 1-2 g/24 hr | ||
| Urea | 6-17 g/24 hr | ||
| Myoglobin | Absent | ||
| RBCs | 0-5 per low-power field | ||
| WBCs | 0-5 per low-power field | ||
| Bacteria | None to few | ||
| Casts | None to few |
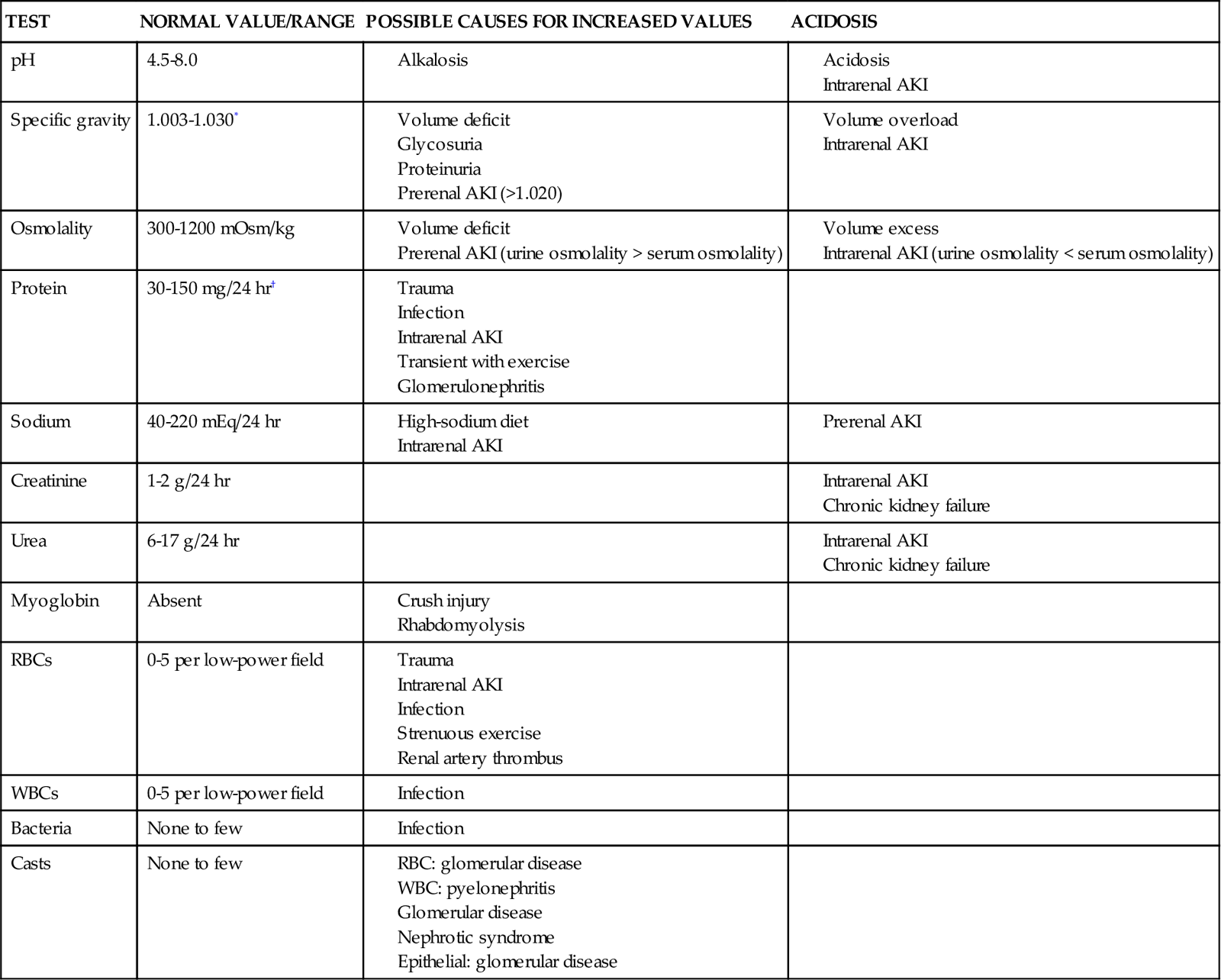
RBC, red blood cell; WBC, white blood cell.
†Higher values usually apply for persons after exercise; lower values apply for persons at rest.
Diagnostic Procedures
Imaging Studies
Although laboratory assessment is used most often in diagnosing kidney problems in the critically ill patient, imaging studies can confirm or clarify causes of particular disorders. Imaging includes the use of ultrasound and radiologic techniques. Kidney ultrasound is especially useful in determining the size, shape, and contour of the kidneys, the presence of masses or cysts, and the presence of renal artery stenosis.25,26 Radiological assessment ranges from basic to more complex (Table 19-4) and provides information about abnormal masses, abnormal fluid collections, obstructions, vascular supply alterations, and other disorders of the kidneys and urinary tract.2,24–26
TABLE 19-4
| TEST | COMMENTS |
| Kidney-ureter-bladder (KUB) radiograph | Flat-plate x-ray film of the abdomen; determines position, size, and structure of the kidneys, urinary tract, and pelvis; useful for evaluating the presence of calculi and masses; usually followed by additional tests |
| Intravenous pyelogram (IVP) | Intravenous injection of contrast with radiography; allows visualization of internal kidney tissues |
| Angiography | Injection of contrast into arterial blood perfusing the kidneys; allows visualization of renal blood flow; may also visualize stenosis, cysts, clots, trauma, and infarctions |
| Computed tomography (CT) | Radioisotope is administered by intravenous route and absorbed by the kidneys; scintillation photography is then performed in several planes; spiral or helical CT allows rapid imaging; density of the image helps evaluate kidney vessels, perfusion, tumors, cysts, stones/calculi, hemorrhage, necrosis, and trauma |
| Ultrasound | High-frequency sound waves are transmitted to the kidneys and urinary tract, and the image is viewed on an oscilloscope; noninvasive; identifies fluid accumulation or obstruction, cysts, stones/calculi, and masses; useful for evaluating kidney before biopsy |
| Magnetic resonance imaging (MRI) | A scanner produces three-dimensional images in response to the application of high-energy radiofrequency waves to the tissues; produces clear images; density of the image may indicate trauma, cysts, masses, malformation of the vessels or tubules stones/calculi, and necrosis |
Some radiologic studies require the use of a contrast agent or injection of a radiopaque dye. Because many of the dyes used in radiology are potentially nephrotoxic, they must be used carefully in patients with AKI or chronic kidney disease. An individual with AKI undergoing a test using a contrast agent may experience deterioration of kidney function caused by the dye. To prevent nephrotoxicity, adequate hydration before and after the test and careful monitoring of kidney function are indicated any time a contrast agent is used.
Kidney Biopsy
Kidney biopsy is the definitive tool for diagnosing disease processes of the kidney. Two methods are used: closed biopsy and open biopsy. Percutaneous needle biopsy (closed method) involves inserting a needle through the flank to obtain a specimen of cortical and medullary kidney tissue. An open biopsy is a surgical procedure and is rarely done in critically ill patients. In either case, biopsy is often the last choice for diagnostic assessment in the critically ill patient because of the postprocedural risks of bleeding, hematoma formation, and infection.