23.12 Rectal drug administration
Background
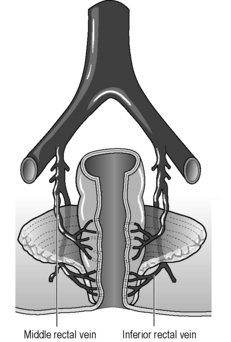
Status epilepticus is a major paediatric medical emergency that requires emergency treatment. Although the first priority is airway and breathing, additional therapy includes termination of the seizure. Cannulating a peripheral vein in a child in status epilepticus limits timely delivery of essential advanced life support (ALS) drugs, especially in infants and toddlers. However, intravenous (IV), intramuscular (IM), or intraosseous drug administration is not necessary because rectal benzodiazepine administration is probably as effective and has no added complications. Rectal drug administration is a time-honoured drug-delivery technique in children and is useful for many medications, including antipyretics and anticonvulsants. The rectum is highly vascularised, and lipid-soluble drugs are rapidly absorbed when correctly administered (Fig. 23.12.1). Diazepam is a lipid-soluble benzodiazepine that is reliably absorbed through the rectum and will terminate most seizures without further treatment. Lorazepam is an effective alternative drug choice.
Preparation
Procedure
 Position the patient in the decubitus position, knee–chest position, or supine position (Fig. 23.12.2) and have a second person hold the legs apart.
Position the patient in the decubitus position, knee–chest position, or supine position (Fig. 23.12.2) and have a second person hold the legs apart.Complications
Tips
Appleton R., Martland T., Phillips B. Drug management for acute tonic-clonic convulsions including convulsive status epilepticus in children. Cochrane Database Syst Rev. 4, 2002. CD001905
Dieckmann R.A., Brownstein D., Gausche M. Textbook for paediatric education for prehospital professionals. Sudbury, MA: Jones & Bartlett. 2001:291-292.
Dieckmann R.A., Fiser D., Selbst S. Illustrated textbook of paediatric emergency and critical care procedures. St Louis, MO: Mosby. 1997:274-278.
Dieckmann R.A. Rectal diazepam for prehospital paediatric status epilepticus. Ann Emerg Med. 1994;23(2):216-224.
Fitzgerald B.J., Okos A.J., Miller J.W. Treatment of out-of-hospital status epilepticus with diazepam rectal gel. Seizure. 2003;12(1):52-55.
Mitchell W.G., Conry J.A., Crumrine P.K., et al. An open-label study of repeated use of diazepam rectal gel (Diastat) for episodes of acute breakthrough seizures and clusters: Safety, efficacy, and tolerance. North American Diastat Group. Epilepsia. 1999;40(11):1610-1617.