CHAPTER 261 Radiosurgery for Functional Disorders
The origin of stereotactic radiosurgery parallels the developmental history of functional neurosurgery. Leksell initially conceived the idea of closed-skull, single-session irradiation of a precisely defined intracranial target in 1951. He applied this concept immediately to functional neurosurgery.1 At that time, functional destruction of normal brain required thermal energy or injection of a chemical such as phenol. Leksell cross-fired photon or proton radiation beams to achieve a similar goal. The initial radiosurgical concept was to create a small, precisely defined focal lesion that was defined by image guidance. Contrast-enhanced encephalography provided relative identification of such targets. Even though the ganglionic portion of the trigeminal nerve could be indirectly located with plain radiographs or cisternograms, deep brain targets required air or positive contrast-enhanced ventriculography; direct visualization of the target for functional radiosurgery required the later development of computed imaging technology. Thus, radiosurgical techniques were used to create image-guided physiologic inactivity or focally destructive brain lesions without neurophysiologic guidance. This concept was controversial, and the lack of neurophysiologic guidance remained the greatest argument against the use of radiosurgery for selected disorders. Nevertheless, the use of radiosurgery as a “lesion generator” is based on extensive animal studies that defined the dose, volume, and temporal response of the irradiated tissue. The utility of radiosurgery has now been compared with that of the microsurgical, percutaneous, and electrode-based techniques used for functional neurologic disorders. Current anatomic targets include the trigeminal nerve (for trigeminal neuralgia), the thalamus (for tremor or pain), the cingulate gyrus or anterior internal capsule (for pain or psychiatric illness), the hypothalamus (for cancer pain), and the hippocampus (for epilepsy).2,3 Current indications and expected outcomes after radiosurgery are discussed in this chapter.
Leksell first coupled an orthovoltage x-ray tube to his early-generation stereotactic frame.1 Later, he worked with physicist Borje Larsson to cross-fire proton beams5 and subsequently used a modified linear accelerator. His decision to build the first Gamma Knife in 1967 reflected his frustration with particle beam technology, which required that the patient travel to a special cyclotron center. The first Gamma Knife collimator helmets created a discoid volume of focal irradiation that could “section” white matter tracts or brain tissue in a manner similar to a leukotome or other instrument. Later models of the Gamma Knife have provided more flexibility in the creation of lesions or effects of different volumes, together with precise robotic capability.
The Early Years of Functional Radiosurgery
Before 1978, all uses of radiosurgery remained limited because of the lack of high-resolution neuroimaging techniques to identify brain lesions or functional brain regions. Angiographic targeting of arteriovenous malformations proved successful but was limited by the two-dimensional estimates of complex three-dimensional target volumes. Functional radiosurgery was performed for a limited number of patients with intractable pain related to malignancy,6,7 movement disorders,8 psychiatric dysfunction,9,10 and trigeminal neuralgia.4 On the sidelines, percutaneous retrogasserian glycerol rhizotomy was developed from an observation made during refinement of the Gamma Knife technique for trigeminal neuralgia. After injection of the glycerol to localize the trigeminal nerve before radiosurgery, the trigeminal neuralgia pain was relieved.
For intractable pain related to malignancy, radiosurgery was used both for hypophysectomy and for medial thalamotomy. Although the procedure was noninvasive, the latency interval for lesion generation and pain relief was one obvious drawback. Steiner and colleagues presented results from an autopsy study after radiosurgery for cancer pain in 1980.7 The ablative dose for tissue volumes had been estimated during animal experiments through the 1960s involving the use of protons and photons.5,11,12 The initial patients who underwent radiosurgery for tissue ablation received maximum doses of 100 to 250 Gy. With small volumes, doses in excess of 150 Gy provided consistent tissue necrosis in animal models. Because these first patients were treated for pain from a terminal malignancy, they did not live long enough to sustain a potential complication from such high doses. The clinical use of such doses proved to be the foundation for later use in tremor management.
Dose Selection for Parenchymal Functional Radiosurgery
Early animal experiments showed consistent creation of lesions with doses at or higher than 150 Gy.11,12 Clinical data showed that pain relief usually occurred within 3 weeks after radiosurgery.7 In rat experiments at 200 Gy with a single 4-mm isocenter, we found a consistent relationship for lesion generation that substantiated observations from that human study.13 Doses of 200 Gy were delivered to the rat frontal brain, and then the brain was studied at 1, 7, 14, 21, 60, and 90 days after irradiation. At 1 and 7 days, the brain continued to appear normal. By 14 days, the parenchyma appeared slightly edematous within the target volume. However, by 21 days, a completely circumscribed volume of necrosis was identified within the radiation volume (4-mm diameter). This remained consistent thereafter. Thus, the clinical observation of pain relief at 21 days noted by Steiner and colleagues was correlated with laboratory findings at the 200-Gy dose.
An ablative radiosurgical lesion appears as a punched-out, circumscribed volume of complete parenchymal necrosis with cavitation. Within a 1- to 3-mm rim that characterizes the steep falloff in radiation dose, normalization of tissue appearance is found. In this zone, blood vessels appear thickened and hyalinized, and protein extravasation can often be identified. The brain is edematous in this region, either from an increase in extracellular fluid or from intracellular swelling secondary to gliosis. Acute or chronic inflammatory cells are present. Magnetic resonance imaging (MRI) demonstrates all these features after radiosurgical thalamotomy—a sharply defined, contrast-enhanced rim that defines the low-signal lesion (on short TR images) surrounded by a zone of high-signal brain tissue (on long TR images).14 Friehs and colleagues collected imaging data from four centers that created functional radiosurgical lesions (N = 56). They found that maximum doses in excess of 160 Gy were more likely to produce lesions larger than expected and recommended single 4-mm-isocenter lesions at doses below 160 Gy.15
Studies at the University of Pittsburgh found that in both large- and small-animal models, doses of 100 Gy or higher caused necrosis but the delay until necrosis was longer.13,16,17 To identify the effect of increasing volume, we used an 8-mm collimator in a baboon model and found that an 8-mm-diameter necrotic lesion developed in half the animals at doses as low as 50 Gy.18 Dose, volume, and time are the three key factors that determine the nature of the functional ablative lesion. Once created, this lesion remains stable for years.11
The limitation of radiosurgical technology as a lesion generator stems from the inability to reliably control the effects of dose and volume. When a larger brain target may be desirable, the sharp falloff in dose outside the target becomes less steep with increasing volume. The risk for an adverse radiation effect outside the target volume becomes problematic.19 At small volumes (i.e., single 4-mm collimator), the radiosurgery-created lesion appears more consistent.
Imaging in Functional Surgery
Because physiologic information is excluded from the targeting component of a functional radiosurgical procedure, high-quality stereotactic neuroimaging must be performed. The imaging must be accurate because small volumes are irradiated. In addition, the imaging must have sufficient resolution to identify the target structure but also show important regional tissues. MRI is the preferred imaging tool for functional radiosurgery.20–23
Accurate stereotactic MRI-based localization should be confirmed at each institution.24 The use of fast inversion recovery or other long–relaxation time MRI sequences helps separate gray and white matter structures. However, to this day, targeting of physiologically abnormal brain regions such as groups of kinesthetic thalamic tremor cells or epileptic foci with imaging alone remains indirect.
Trigeminal Neuralgia
Leksell first used radiosurgical techniques for trigeminal nerve irradiation in 1953.4 He later stated that, “from these observations no definite conclusion should be drawn concerning the optimal dose of radiation or the exact mechanism in site of action in the route or ganglion, or even the general applicability of the method.”4 In 1983, Leksell reported that 63 patients had undergone Gamma Knife radiosurgery for trigeminal neuralgia. The use of gasserian ganglion radiosurgery was reported by Lindquist and coauthors (46 patients) and Rand and associates (12 patients), but inconsistent results were obtained.2,25 These authors concluded that the ganglion was probably not appropriate as the primary radiosurgical target.
Initially, the Pittsburgh group sought to reevaluate the early anecdotal success of trigeminal neuralgia radiosurgery reported by Leksell. They reported a multicenter study in which Gamma Knife radiosurgery was used for trigeminal nerve radiosurgery.21 Targeting the nerve at this location was suggested by Hakänsson and Lindquist as one potential way to improve outcomes. At this location, the nerve could be imaged with high-resolution MRI and was suitable for radiosurgical targeting with a 4-mm collimator (Fig. 261-1). This location offered a great advantage over ganglion irradiation in Meckel’s cave, where the nerve proper could not be imaged readily. In an initial multicenter 50-patient study with 18-month median follow-up, 58% became pain free, 36% had significant improvement (50% to 90% relief), and 6% failed.21 Patients with significant improvement were satisfied, especially in view of the fact that in most patients the pain had been recurrent after multiple previous surgeries. A maximum radiosurgical dose higher than 70 Gy (70 to 90 Gy) was associated with a greater chance of complete pain relief than was 60 or 65 Gy (P = .0003). After publication of this study, centers worldwide have performed trigeminal neuralgia radiosurgery, and there are many reports that have documented the results.
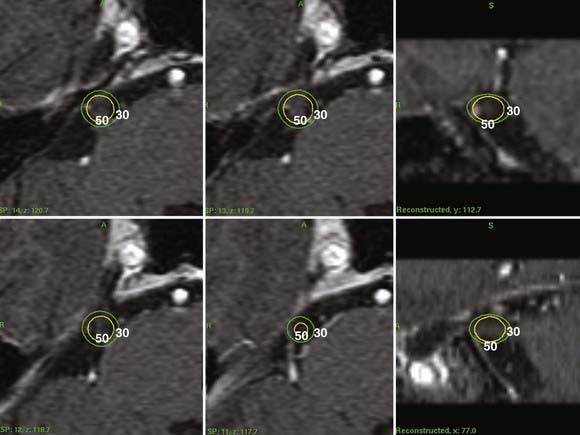
Radiosurgery Technique for Trigeminal Neuralgia
Stereotactic radiosurgery is performed under local anesthesia. High-resolution trigeminal nerve imaging is necessary for accurate radiosurgical targeting. After a sagittal scout sequence, spoiled GRASS (gradient recalled acquisition in a steady state) gradient recombinant (SPGR) axial volume acquisition sequences using 512 × 512 matrices are targeted to the pons and midbrain level. They are divided into 1-mm image slices to provide graphic depiction of the trigeminal nerve (Fig. 261-1). The nerve can be identified in its course from the brainstem to Meckel’s cave. Some patients who have previously undergone surgery (microvascular decompression or percutaneous surgery) present greater imaging challenges because the nerve may be more difficult to identify (as a result of either nerve atrophy or regional fibrosis). In such patients long TR MRI sequences are added to contrast the nerve against the high-signal background of cerebrospinal fluid. An initial concept was to place a 4-mm isocenter 2 to 4 mm anterior to the junction of the trigeminal nerve and pons so that the brainstem surface was usually irradiated at no more than the 30% isodose. Other centers chose a midnerve or anterior nerve target. Computed tomography–based targeting can be performed, with or without contrast-enhanced cisternography, in patients who cannot undergo MRI. The range of the maximum radiosurgical dose is typically 75 to 90 Gy.26 De Salles and coworkers used a modified linear accelerator to irradiate the trigeminal nerve in patients with neuropathic pain related to skull base cancer and for trigeminal neuralgia.27
Clinical Response
Improvement after radiosurgery has been defined as a reduction in both the frequency and severity of trigeminal neuralgia attacks. Although some physicians believe that only total pain relief with no further need for medication should be considered management success, many of our patients believe otherwise. Because so many patients have failed other treatments, many were grateful for any significant relief even if occasional pain persisted. Numerous studies have reported outcomes after radiosurgery for trigeminal neuralgia; however, the definition of improvement in pain is not uniform.8,21,28–33,35–41 Pain relief (according to the patient) can be generally coded into three categories, including poor response or treatment failure (<50% pain relief), good pain response (>50% pain relief), and complete pain relief with or without medications.
The maximum level of pain relief is typically achieved within 1 month after radiosurgery.21,38,40,42–46 Disappearance of the trigger areas or frank pain relief occurs within 24 hours of treatment in up to a third of treated patients.8 Complete pain relief within 1 week of treatment is reported in over 40% of eventual responders.46 More than three quarters of partial and complete responders will have responded within 3 months of treatment and more than 90% of responders by 6 months.43 Kondziolka and coauthors reported in their multi-institutional studies that initial improvement in trigeminal neuralgia was noted in 91 patients (86%).21,26 There were 64 patients who had complete pain relief without medication, 18 who had a good pain response, 9 who were slightly improved, and 15 with no improvement. At last follow-up, significant pain relief was noted by 77% of patients (good response plus complete pain relief). Young and associates reported a 74% rate of complete pain relief with cessation of medical therapy in their 60-patient series, with better results seen in patients with no previous surgical history.47
However, approximately 15% of patients do not experience greater than 50% pain relief. If treatment failure is defined as failure to obtain complete pain relief, the failure rate is doubled.38,46,48,49 We believe that it is safe to consider the treatment a failure if no response has taken place after 3 to 6 months.8 In addition, recurrences are most common in the first year. Rates of recurrence ranged from 5% to 42% in the studies.21,28,31,35–38,40,42,43,49,78 Kondziolka and coauthors reported that relapse of pain was noted in just 6 of 64 patients who attained complete relief (10%) and that this relapse occurred within 10 months after the onset of complete relief.21 Maesawa and colleagues stated that 71% of patients achieved or maintained complete or greater than 50% relief at 2 years and 56% maintained the relief 5 years after initial response; the rate of achieving and maintaining complete pain relief was 59% at 2 years and 38% at 5 years.43 The number of patients with good or complete pain relief has decreased over years, indicative of some lessening of the effect over time. More series with extended follow-up past 5 years are required to study this issue more definitively.
Prognostic Factors
Different investigators have tried to determine specific patient factors related to relief of pain. The absence of previous surgery was suggested as a significant factor associated with achieving and maintaining complete pain relief.38,39,43 However, one study found no differences with respect to previous surgery.51 Atypical features of pain may be associated with a poorer response to treatment and a greater probability of pain recurrence.40,43,46 Rogers and associates reported complete pain relief rates of 49% in patients with typical pain and 9% in patients with atypical features of pain.40 However, Pollock and colleagues did not find any differences in these groups, but the development of new facial sensory loss was found to correlate with sustained complete pain relief in their study.38 In addition, they found two factors at or near statistical significance for achieving and maintaining an excellent outcome: younger patient age and longer length of the irradiated portion of the nerve; however, Régis and coworkers noted that the probability of being pain free was lower in patients younger than 60 years (55.7% versus 90.9%, P = .01).78 To date, increasing the radiosurgical dose from 70 to 90 Gy or the number of lesions (from one to two isocenters) has not produced a definite improvement in pain outcomes, although there is a trend to more relief with higher doses. Nonetheless, a higher dose or increase in the volume of irradiated nerve has led to an increase in the rate of sensory complications.
Complications
Anesthesia dolorosa, a condition of disabling, painful facial numbness, is a potential side effect of irradiating the trigeminal nerve, but this finding has been extremely rare after radiosurgery. In the Pittsburgh series, one patient complained of this problem (she had undergone microvascular decompression before radiosurgery) and then had a dorsal root entry zone (DREZ) lesion made at another institution. Complications from radiosurgery are uncommon and primarily limited to new or increased trigeminal paresthesias or sensory loss.48 Rates of facial dysesthesia of 0% to 10% have been associated with varying doses of less than 90 Gy.78 In the multi-institution study, increased facial paresthesia developed in 3 of 50 patients (6%) after radiosurgery.21 Using similar techniques, Young and coworkers noted that only 1 of their 60 patients had increased facial sensory loss; this patient had a trigeminal schwannoma.49 In the last Pittsburgh review, the rate was 10%. However, Nicol and coauthors reported that 16.7% of their patients experienced increased or new facial numbness after the procedure and four instances of dysgeusia; such a high rate of facial numbness and the development of a rare adverse effect could be due to the higher dose of radiation used in this study.36 Treating longer segments of the trigeminal nerve may lead to a higher incidence of hypoesthesia, with Villavicencio and associates reporting numbness in 47% of patients after radiosurgery in their multicenter study.52 The absence of infection, cerebrospinal fluid leakage, anesthesia complications, hearing loss, facial hematoma, facial weakness, or brainstem injury has established radiosurgery as a low-morbidity surgical alternative for many patients.
Physiologic Effect of Radiosurgery
It was speculated that high-dose single-fraction irradiation leads to an electrophysiologic block of ephaptic transmission without producing tissue destruction. This is supported by the observation that most patients maintain normal trigeminal function.21,47 MRI studies performed 4 to 24 months after radiosurgery show contrast enhancement at the target, perhaps indicating transient opening of the blood-nerve barrier. Because the nerve is myelinated by oligodendrocytes and perhaps is more sensitive than Schwann cell myelin to irradiation, it was hypothesized that a stronger radiobiologic effect would occur at this portion of the nerve.26
Histologic and ultrastructural studies performed in a baboon model showed nonspecific effects on different trigeminal nerve axons. Normal nerves were irradiated with a 4-mm collimator to maximum doses of 80 or 100 Gy.17 Although focal necrosis was found 6 months after 100-Gy radiosurgery, 80 Gy induced partial axonal degeneration.
Radiosurgical Thalamotomy
Ventrolateral thalamic surgery for the management of tremor related to Parkinson’s disease remains a proven and time-honored concept within functional neurosurgery. Traditionally, it has involved imaging definition of the thalamic target, placement of an electrode into the thalamus, physiologic recording and stimulation at the target site, and creation of a lesion or provision of electrical stimulation. Radiosurgical thalamotomy by definition avoids placement of an electrode and evaluation of the physiologic response. In radiosurgery, imaging definition alone is used to determine lesion placement. Through the use of contrast-enhanced ventriculography, computed tomography, and more recently, stereotactic MRI, thalamotomy with the Gamma Knife has been performed at centers across the world.8,20,53–55 As discussed earlier, the issues of lesion volume and dose selection remain important. Even though radiosurgery can abolish tremor, many surgeons currently believe that although adequate results might be obtained, better results may be possible with deep brain stimulation (DBS). The challenges inherent in choosing the best possible ablative target by imaging alone are significant. Radiosurgical thalamotomy, if attempted, should be performed by surgeons experienced in radiofrequency thalamotomy or DBS.
Because of the absence of electrophysiologic information, inability to stop the lesion during surgery, and latency until a clinical response occurs, most surgeons perform radiosurgery primarily in patients with advanced age or medical disorders in which electrode placement would be associated with higher risk. Ohye’s group began to perform radiosurgical thalamotomy contralateral to a previous radiofrequency lesion or to enlarge a previously mapped lesion.53 Duma and colleagues reported a 5-year experience consisting of 38 Gamma Knife thalamotomies with a 28-month mean follow-up.20 Complete tremor abolition was noted in 24%, excellent relief in 26%, good improvement in 29%, and little to no benefit in 21%. The median time to improvement was 2 months, consistent with data from previous animal experiments. They used a dose range of 110 to 165 Gy but achieved better results at higher doses. Such high doses may exert effects on a larger surrounding tissue volume of kinesthetic tremor cells (outside the sharply defined necrotic volume), which translates into tremor reduction and overcomes any limitations in target selection. Young and coworkers reported that 88% of 27 patients who underwent radiosurgical thalamotomy for tremor (120 to 160 Gy) became tremor free or “nearly” tremor free.22 Hirato and associates also found tremor suppression after Gamma Knife thalamotomy in a small patient series.53 Friehs and coauthors reported their experience with radiosurgical thalamotomy (n = 3) and caudatotomy (n = 10); clinical improvement was achieved in most patients with no morbidity.56
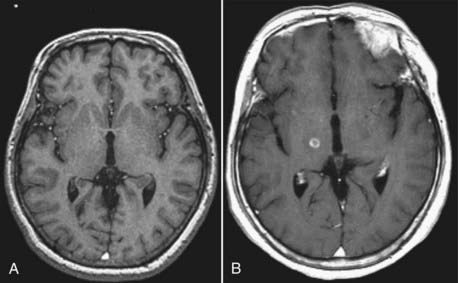
The mean age of 77 years in the Pittsburgh radiosurgical series is older than the mean age of 60 years in their DBS series.57 Gamma Knife radiosurgery proved to be effective in improving medically refractive essential tremor in a predominantly elderly patient series. Eighteen patients (69%) improved in both action tremor and writing scores, and an additional six (23%) improved in action tremor scores. Thirteen patients (50%) had either no or only slight intermittent tremor in the affected extremity, and 90% had some degree of clinically significant improvement in tremor. Overall, the mean Fahn-Tolosa-Marin tremor score improved from 3.8 to 1.7 (P < .000015). After radiosurgery, MRI usually showed a 4- to 5-mm round, well-circumscribed lesion with peripheral contrast enhancement surrounding a low-signal region (Fig. 261-2). A localized area of high signal (seen on long–relaxation time studies) demonstrated the peripheral neuronal effect, which was manifested as an increase in intracellular or extracellular water. Two patients with complications had different MRI findings. Although the enhancing lesion created in one patient was unexpectedly large, complete resolution was seen on subsequent imaging. This finding indicated that the response was related to temporary changes in the blood-brain barrier and not to permanent radiation necrosis.
As noted earlier, the target volume is crucial. Early results with larger target volumes using an 8-mm collimator were reported by Lindquist and colleagues.2 Delayed cerebral edema and regions of radiation necrosis at high doses testified to the volume effects of radiosurgery.14 Similar problems have been noted with combinations of 4-mm isocenters to construct a cylindrical rather than spherical target volume.19,22 Nevertheless, the ability to create a small-volume lesion with radiosurgery without performance of a craniostomy or invasive placement of an electrode remains an attractive consideration. To that end, several surgeons have evaluated the use of radiosurgery for medial thalamotomy and for pallidotomy, procedures in which the usefulness of physiologic recording or stimulation was initially less clear.
Radiosurgical Pallidotomy
There was a resurgence in the use of radiofrequency-based stereotactic pallidotomy for patients with advanced Parkinson’s disease beginning in 1992. Some investigators then performed Gamma Knife pallidotomy under image guidance alone as an alternative to electrode techniques. Rand and coauthors reported their preliminary results after radiosurgical pallidotomy and noted relief of contralateral rigidity in four of eight patients.58 No patient in their series sustained a complication. Friedman and associates reported on four patients after Gamma Knife pallidotomy (180 Gy), with improvement in just one patient.59 They noted heterogeneity in lesion volumes on MRI, a finding also documented by others. In contrast to the thalamus, where small radiosurgical lesions appeared consistent, pallidotomy lesions may be more variable because of effects on perforating arteries that supply that region of the basal ganglia. Lesion volumes and contrast enhancement patterns seem less consistent.22 At our center, only one radiosurgical pallidotomy has been performed. At present, this technique is performed rarely and DBS remains a much more valuable therapy for most patients with an array of parkinsonian symptoms.60
Radiosurgery for Pain
The use of radiosurgery as an ablative tool to treat pain has a long history. Unfortunately, too few patients have been managed to draw any strong conclusions. Since the case report by Leksell in 1968 and the larger series by Steiner and coworkers in 1980, little has been written.6,7 In Leksell’s 2 patients with carcinoma, the centrum medianum target received doses of 250 and 200 Gy. The second patient underwent bilateral radiosurgery spaced 2 months apart and became pain free. In Steiner and colleagues’ series, doses as high as 250 Gy were believed unnecessary because of the sharp dose gradient. Young and associates performed medial thalamotomy for the treatment of chronic noncancer pain in patients who had failed comprehensive medical, surgical, and behavioral therapies.61 In 1996 they reported that two thirds of their 41 patients had at least a 50% reduction in pain intensity estimates along with improvement in physical and social functioning.3 As might be expected, patients with deafferentation pain responded poorly, but more encouraging results were identified in patients with nociceptive syndromes. Again, they advocated caution when using volumes larger than those obtained with a single 4-mm isocenter and when using doses higher than 160 Gy.
Hayashi and colleagues performed pituitary gland-stalk ablation by Gamma Knife radiosurgery and targeted the border between the pituitary stalk and gland with a maximum dose of 160 Gy via the 8-mm collimator to control cancer pain. They enrolled nine patients with bone metastases and pain controlled well by morphine, a Karnofsky Performance Scale score higher than 40, and no previous radiation therapy.62 All patients had failed previous pain treatments except morphine. All patients became pain free within a few days after radiosurgery, and the pain relief was maintained as long as they lived. No recurrence of pain was seen. In addition, in no patient did panhypopituitarism or diabetes insipidus develop. This strategy of pituitary gland-stalk ablation for pain control also showed a good initial response (87.5%) in eight patients with thalamic pain syndrome; however, the majority of patients (71.4%) experienced recurrence of pain during the 6 month follow-up.63
Radiosurgery for Psychiatric Disorders
There is renewed interest in radiosurgical lesioning of the anterior internal capsule (anterior capsulotomy) in patients with medically refractory obsessive-compulsive disorder (OCD). Radiosurgery for OCD and anxiety neurosis has been performed for more than 45 years.9 The first radiosurgical capsulotomy was performed by Leksell and colleagues in 1953 with 300-kV x-rays.64 Initially, pneumoencephalography was used to define the target for placement of bilateral anterior internal capsule lesions. Five of the initial 7 patients had long-term benefit after 7 years of follow-up.2 Since 1988, an additional 10 patients were treated at the Karolinska Institute under stereotactic MRI guidance. The initial use of an 8-mm collimator resulted in excessive edema, so these authors recommended the use of only 4-mm isocenters.2 The results seem to be as efficacious as when conventional radiofrequency lesioning is performed.65 Kihlstrom and associates reported a stable imaging appearance of radiosurgical lesions 15 to 18 years after capsulotomy.66 Oval-shaped radiosurgical lesions in the anterior internal capsule or cingulate gyrus may have an impact on affective disorders or anxiety neuroses.
Radiosurgery for Epilepsy
There is current interest in the use of radiosurgery for patients with focal epilepsy. The observation that brain irradiation (via radiation therapy or radiosurgery) could lead to cessation of seizures has spurred several groups to work in this field despite the lack of a consistent approach to defining the target volume. In 1985, Barcia-Salorio and coauthors reported on 6 patients with epilepsy who underwent low-dose radiosurgery. The epileptic focus was localized by means of conventional scalp electroencephalography (EEG), subarachnoid electrodes, and depth electrodes. Radiosurgery (a 10-mm collimator to deliver an estimated 10-Gy dose) was performed with a cobalt unit coupled to a stereotactic localizer. They hypothesized that this low radiation dose provided a specific effect on epileptic neurons without inducing tissue necrosis. In 1994 they provided a long-term analysis in a series of 11 patients who received doses ranging from 10 to 20 Gy. Five patients had complete cessation of seizures, and an additional 5 were improved. Seizures began to decrease gradually 3 to 12 months after radiosurgery.67 After this work, Lindquist and colleagues at the Karolinska Institute began to perform epilepsy radiosurgery with advanced localization techniques that included magnetoencephalography (MEG) to define interictal activity.2,68 In some patients, the epileptic dipole activity identified on MEG before radiosurgery later resolved along with cessation of seizures. Other forms of functional imaging can also be of value in radiosurgery. At the same time, radiosurgery was evaluated in animal models of epilepsy. We used the kainic acid model of hippocampal epilepsy in the rat and were able to stop seizures and improve animal behavior.18,69 Rats were randomized to control or radiosurgical arms (20, 40, 60, or 100 Gy) and then evaluated with serial EEG, behavioral studies, functional MRI, and histology.
More recently, radiosurgery has been of value in patients with gelastic or generalized seizures related to hypothalamic hamartomas.70 A larger indication may involve the creation of an amygdalohippocampal lesion in patients with mesial temporal sclerosis–related epilepsy as proposed by Régis and associates.50,71 In 1993, Régis and associates in Marseille performed selective amygdalohippocampal radiosurgery for mesial temporal lobe epilepsy. Gamma Knife radiosurgery was used to create a conformal volume of radiation for the amygdala and hippocampus. This approximate 7-cc volume represented the largest functional target irradiated to that time. They delivered a margin dose of 25 Gy to the 50% isodose line, a dose that later caused target necrosis. The first patient became seizure free immediately and the second after a latency of almost 1 year. Serial MRI showed target contrast enhancement that corresponded to the 50% isodose line.71 Patients managed at their center have been part of a multidisciplinary prospective evaluation and treatment protocol. A recently published longer term evaluation with 8-year mean follow-up (margin dose of 24 Gy) found that 9 of 16 patients were seizure free.72
Current issues that remain important for epilepsy radiosurgery include dose selection (necrotizing versus non-necrotizing), localization methods for nonlesional epilepsy, the target volume necessary for irradiation, and the expected short- and long-term outcomes. It is not known what kind of tissue effect is required to stop the generation or propagation of seizures. Some groups have used low doses (i.e., 10 to 20 Gy), in which case few if any histologic changes would be expected. Others have used doses as high as 100 Gy, which causes target necrosis and regional brain edema.73 A typical amygdalohippocampal radiosurgical maximum dose to a volume of less than 7.5 cc is 40 to 50 Gy.
If focal hippocampal (or any other brain tissue) irradiation can eliminate seizures without the need for complete tissue destruction, radiosurgery may become an important therapy for patients with intractable epilepsy. At the same time we await improvements in tools for localization of the seizure focus.23
Other Indications
There are isolated reports on the use of radiosurgery for other functional disorders. Pollock and Kondziolka first irradiated the sphenopalatine ganglion in a patient with sphenopalatine neuralgia by using an 8-mm collimator and maximum dose of 90 Gy. They found prompt relief of vasomotor symptoms but a latency of several months in relief of pain.74
In 1998, Ford and coauthors reported positive results after radiosurgery targeting the trigeminal nerve in patients with chronic cluster headaches.75,76 However, two subsequent studies did not support further use of radiosurgery targeting the trigeminal nerve for chronic cluster headache because of the high recurrence rate of attacks and potentially severe side effects.77 Recently, a favorable outcome of radiosurgery targeting the pterygopalatine ganglion in a patient with medically intractable cluster headache was reported.78 Additional studies with longer follow-up data are mandatory to determine the long-term efficacy and late side effects.
Bartolomei F, Hayashi M, Tamura M, et al. Long-term efficacy of gamma knife radiosurgery in mesial temporal lobe epilepsy. Neurology. 2008;70:1658-1663.
Flickinger JC, Pollock BE, Kondziolka D, et al. Does increased nerve length within the treatment volume improve trigeminal neuralgia radiosurgery? A prospective double-blind, randomized study. Int J Radiat Oncol Biol Phys. 2001;51:449-454.
Hayashi M, Taira T, Chernov M, et al. Role of pituitary radiosurgery for the management of intractable pain and potential future applications. Stereotact Funct Neurosurg. 2003;81:75-83.
Henson CF, Goldman HW, Rosenwasser RH, et al. Glycerol rhizotomy versus Gamma Knife radiosurgery for the treatment of trigeminal neuralgia: an analysis of patients treated at one institution. Int J Radiat Oncol Biol Phys. 2005;63:82-90.
Kondziolka D, Lacomis D, Niranjan A, et al. Histologic effects of trigeminal nerve radiosurgery in a primate model: Implications for trigeminal neuralgia radiosurgery. Neurosurgery. 2000;46:971-977.
Kondziolka D, Lunsford LD, Flickinger JC, et al. Stereotactic radiosurgery for trigeminal neuralgia: A multi-institution study using the gamma unit. J Neurosurg. 1996;84:940-945.
Kondziolka D, Ong J, Lee JYK, et al. Gamma knife thalamotomy for essential tremor. J Neurosurg. 2008;108:111-117.
Lopez BC, Hamlyn PJ, Zakrzewska JM. Stereotactic radiosurgery for primary trigeminal neuralgia: state of the evidence and recommendations for future reports. J Neurol Neurosurg Psychiatry. 2004;75:1019-1024.
Maesawa S, Kondziolka D, Dixon E, et al. Subnecrotic stereotactic radiosurgery controlling epilepsy produced by kainic acid injection in rats. J Neurosurg. 2000;93:1033-1040.
Massager N, Lorenzoni J, Devriendt D, et al. Gamma Knife surgery for idiopathic trigeminal neuralgia performed using a far-anterior cisternal target and a high dose of radiation. J Neurosurg. 2004;100:597-605.
Mathieu D, Kondziolka D, Niranjan A, et al. Gamma knife radiosurgery for epilepsy caused by hypothalamic hamartomas. Stereotact Funct Neurosurg. 2006;84:82-87.
Petit JH, Herman JM, Nagda S, et al. Radiosurgical treatment of trigeminal neuralgia: evaluating quality of life and treatment outcomes. Int J Radiat Oncol Biol Phys. 2003;56:1147-1153.
Pollock B, Kondziolka D. Stereotactic radiosurgical treatment of sphenopalatine neuralgia. J Neurosurg. 1997;87:450-453.
Pollock BE, Phuong LK, Gorman DA, et al. Stereotactic radiosurgery for idiopathic trigeminal neuralgia. J Neurosurg. 2002;97:347-353.
Régis J, Metellus P, Hayashi M, et al. Prospective controlled trial of Gamma Knife surgery for essential trigeminal neuralgia. J Neurosurg. 2006;104:913-924.
Régis J, Rey M, Bartolomei F, et al. Gamma knife surgery in mesial temporal lobe epilepsy: a prospective multicenter study. Epilepsia. 2004;45:504-515.
Sheehan J, Pan HC, Stroila M, et al. Gamma Knife surgery for trigeminal neuralgia: outcomes and prognostic factors. J Neurosurg. 2005;102:434-441.
Villavicencio AT, Lim M, Burneikiene S, et al. CyberKnife radiosurgery for trigeminal neuralgia treatment: A preliminary multicenter experience. Neurosurgery. 2008;62:647-655.
1 Leksell L. The stereotaxic method and radiosurgery of the brain. Acta Chir Scand. 1951;102:316-319.
2 Lindquist C, Kihlstrom L, Hellstrand DE. Functional neurosurgery—a future for the Gamma Knife? Stereotact Funct Neurosurg. 1991;57:72-81.
3 Young RF, Vermeulen S, Posewitz A, et al. Functional neurosurgery with the Leksell Gamma Knife. Radiosurgery. 1996;1:218-228.
4 Leksell L. Stereotaxic radiosurgery in trigeminal neuralgia. Acta Chir Scand. 1971;137:311-314.
5 Larsson B, Leksell L, Rexed B, et al. The high-energy proton beam as a neurosurgical tool. Nature. 1958;182:1222-1223.
6 Leksell L. Cerebral radiosurgery I. Gammathalamotomy in two cases of intractable pain. Acta Chir Scand. 1968;134:585-595.
7 Steiner L, Forster D, Leksell L, et al. Gammathalamotomy in intractable pain. Acta Neurochir. 1980;52:173-184.
8 Lopez BC, Hamlyn PJ, Zakrzewska JM. Stereotactic radiosurgery for primary trigeminal neuralgia: state of the evidence and recommendations for future reports. J Neurol Neurosurg Psychiatry. 2004;75:1019-1024.
9 Leksell L, Backlund EO. Stereotactic gammacapsulotomy. In: Hitchcock ER, Ballantine HT, Meyerson BA, editors. Modern Concepts in Psychiatric Surgery. Amsterdam: Elsevier; 1979:213-216.
10 Rylander G. Stereotactic radiosurgery in anxiety and obsessive-compulsive states: Psychiatric aspects. In: Hitchcock ER, Ballantine HT, Meyerson BA, editors. Modern Concepts in Psychiatric Surgery. Amsterdam: Elsevier; 1979:235-240.
11 Andersson B, Larsson B, Leksell L, et al. Histopathology of late local radiolesions in the goat brain. Acta Radiol. 1970;9:385-394.
12 Rexed B, Mair W, Sourander P, et al. Effect of high energy protons on the brain of the rabbit. Acta Radiol. 1960;53:289-299.
13 Kondziolka D, Lunsford LD, Claassen D, et al. Radiobiology of radiosurgery. Part I: The normal rat brain model. Neurosurgery. 1992;31:271-279.
14 Leksell L, Herner T, Leksell D, et al. Visualization of stereotactic radiolesions by nuclear magnetic resonance. J Neurol Neurosurg Psychiatry. 1985;48:19-20.
15 Friehs G, Noren G, Ohye C, et al. Lesion size following Gamma Knife treatment for functional disorders. Stereotact Funct Neurosurg. 1996;66(suppl 1):320-328.
16 Kondziolka D, Linskey ME, Lunsford LD. Animal models in radiosurgery. In: Alexander E, Loeffler JS, Lunsford LD, editors. Stereotactic Radiosurgery. New York: McGraw-Hill; 1993:51-64.
17 Kondziolka D, Lacomis D, Niranjan A, et al. Histologic effects of trigeminal nerve radiosurgery in a primate model: Implications for trigeminal neuralgia radiosurgery. Neurosurgery. 2000;46:971-977.
18 Maesawa S, Kondziolka D, Dixon E, et al. Subnecrotic stereotactic radiosurgery controlling epilepsy produced by kainic acid injection in rats. J Neurosurg. 2000;93:1033-1040.
19 Kihlstrom L, Guo WY, Lindquist C, et al. Radiobiology of radiosurgery for refractory anxiety disorders. Neurosurgery. 1995;36:294-302.
20 Duma CM, Jacques DB, Kopyov OV, et al. Gamma Knife radiosurgery for thalamotomy in Parkinsonian tremor: a five-year experience. J Neurosurg. 1998;88:1044-1049.
21 Kondziolka D, Lunsford LD, Flickinger JC, et al. Stereotactic radiosurgery for trigeminal neuralgia: A multi-institution study using the gamma unit. J Neurosurg. 1996;84:940-945.
22 Young RF, Shumway-Cook A, Vermeulen S, et al. Gamma Knife radiosurgery as a lesioning technique in movement disorder surgery. Neurosurg Focus. 1997;2(3):e11.
23 Witt TC, Kondziolka D, Baumann S, et al. Pre-operative cortical localization with functional MRI for use in stereotactic radiosurgery. Stereotact Funct Neurosurg. 1996;66:24-29.
24 Kondziolka D, Dempsey PK, Lunsford LD, et al. A comparison between magnetic resonance imaging and computed tomography for stereotactic coordinate determination. Neurosurgery. 1992;30:402-407.
25 Rand RW, Jacques DB, Melbye RW, et al. Leksell Gamma Knife treatment of tic douloureux. Stereotact Funct Neurosurg. 1993;61(suppl):93-102.
26 Kondziolka D, Lunsford LD, Habeck M, et al. Gamma Knife radiosurgery for trigeminal neuralgia. Neurosurg Clin N Am. 1997;8:79-85.
27 DeSalles A, Buxton W, Solberg T, et al. Linear accelerator radiosurgery for trigeminal neuralgia. Radiosurgery. 1998;2:173-182.
28 Brisman R. Gamma Knife surgery with a dose of 75 to 76.8 gray for trigeminal neuralgia. J Neurosurg. 2004;100:848-854.
29 Cheuk AV, Chin LS, Petit JH, et al. Gamma Knife surgery for trigeminal neuralgia: outcome, imaging, and brainstem correlates. Int J Radiat Oncol Biol Phys. 2004;60:537-541.
30 Drzymala RE, Malyapa RS, Dowling JL, et al. Gamma Knife radiosurgery for trigeminal neuralgia: the Washington University initial experience. Stereotact Funct Neurosurg. 2005;83:148-152.
31 Flickinger JC, Pollock BE, Kondziolka D, et al. Does increased nerve length within the treatment volume improve trigeminal neuralgia radiosurgery? A prospective double-blind, randomized study. Int J Radiat Oncol Biol Phys. 2001;51:449-454.
32 Henson CF, Goldman HW, Rosenwasser RH, et al. Glycerol rhizotomy versus Gamma Knife radiosurgery for the treatment of trigeminal neuralgia: an analysis of patients treated at one institution. Int J Radiat Oncol Biol Phys. 2005;63:82-90.
33 Kim YH, Park CK, Chung HT, et al. Anatomical considerations in Gamma Knife radiosurgery for Idiopathic trigeminal neuralgia. J Korean Neurosurg Soc. 2006;40:148-153.
34 Lunsford LD, Altschuler EM, Flickinger JC, et al. In vivo biological effects of stereotactic radiosurgery: A primate model. Neurosurgery. 1990;27:373-382.
35 Massager N, Lorenzoni J, Devriendt D, et al. Gamma Knife surgery for idiopathic trigeminal neuralgia performed using a far-anterior cisternal target and a high dose of radiation. J Neurosurg. 2004;100:597-605.
36 Nicol B, Regine WF, Courtney C, et al. Gamma Knife radiosurgery using 90 Gy for trigeminal neuralgia. J Neurosurg. 2000;93(Suppl 3):152-154.
37 Petit JH, Herman JM, Nagda S, et al. Radiosurgical treatment of trigeminal neuralgia: evaluating quality of life and treatment outcomes. Int J Radiat Oncol Biol Phys. 2003;56:1147-1153.
38 Pollock BE, Phuong LK, Gorman DA, et al. Stereotactic radiosurgery for idiopathic trigeminal neuralgia. J Neurosurg. 2002;97:347-353.
39 Regis J, Metellus P, Hayashi M, et al. Prospective controlled trial of Gamma Knife surgery for essential trigeminal neuralgia. J Neurosurg. 2006;104:913-924.
40 Rogers CL, Shetter AG, Fiedler JA, et al. Gamma Knife radiosurgery for trigeminal neuralgia: the initial experience of The Barrow Neurological Institute. Int J Radiat Oncol Biol Phys. 2000;47:1013-1019.
41 Sheehan J, Pan HC, Stroila M, et al. Gamma Knife surgery for trigeminal neuralgia: outcomes and prognostic factors. J Neurosurg. 2005;102:434-441.
42 Fountas KN, Lee GP, Smith JR. Outcome of patients undergoing Gamma Knife stereotactic radiosurgery for medically refractory idiopathic trigeminal neuralgia: Medical College of Georgia’s experience. Stereotact Funct Neurosurg. 2006;84:88-96.
43 Maesawa S, Salame C, Flickinger JC, et al. Clinical outcomes after stereotactic radiosurgery for idiopathic trigeminal neuralgia. J Neurosurg. 2001;94:14-20.
44 Urgosik D, Vymazal J, Vladyka V, et al. Gamma Knife treatment of trigeminal neuralgia: clinical and electrophysiological study. Stereotact Funct Neurosurg. 1998;70(Suppl 1)):200-209.
45 Zheng LG, Xu DS, Kang CS, et al. Stereotactic radiosurgery for primary trigeminal neuralgia using the Leksell Gamma unit. Stereotact Funct Neurosurg. 2001;76:29-35.
46 Young RF, Vermulen S, Posewitz A. Gamma Knife radiosurgery for the treatment of trigeminal neuralgia. Stereotact Funct Neurosurg. 1998;70(Suppl 1)):192-199.
47 Young RF, Vermeulen S, Grimm P, et al. Gamma Knife radiosurgery for treatment of trigeminal neuralgia. Idiopathic and tumor related. Neurology. 1997;48:608-614.
48 Guo S, Chao ST, Reuther AM, et al. Review of the treatment of trigeminal neuralgia with Gamma Knife radiosurgery. Stereotact Funct Neurosurg. 2008;86:135-146.
49 Young RF, Vermeulen SS, Grimm P, et al. Electrophysiological target localization is not required for the treatment of functional disorders. Stereotact Funct Neurosurg. 1996;66(Suppl 1)):309-319.
50 Régis J, Rey M, Bartolomei F, et al. Gamma knife surgery in mesial temporal lobe epilepsy: a prospective multicenter study. Epilepsia. 2004;45:504-515.
51 Brisman R. Gamma knife radiosurgery for primary management for trigeminal neuralgia. J Neurosurg. 2000;93(Suppl 3)):159-161.
52 Villavicencio AT, Lim M, Burneikiene S, et al. CyberKnife radiosurgery for trigeminal neuralgia treatment: A preliminary multicenter experience. Neurosurgery. 2008;62:647-655.
53 Hirato M, Ohye C, Shibazaki T, et al. Gamma Knife thalamotomy for the treatment of functional disorders. Stereotact Funct Neurosurg. 1995;64(suppl 1):164-171.
54 Otsuki T, Jokura H, Takahashi K, et al. Stereotactic gamma-thalamotomy with a computerized brain atlas: Technical case report. Neurosurgery. 1994;35:764-768.
55 Pan L, Dai J, Wang BJ, et al. Stereotactic gamma thalamotomy for the treatment of Parkinsonism. Stereotact Funct Neurosurg. 1996;66(suppl 1):329-332.
56 Friehs G, Ojakangas CL, Pachatz P, et al. Thalamotomy and caudatomy with the Gamma Knife as a treatment for Parkinsonism with a comment on lesion sizes. Stereotact Funct Neurosurg. 1995;64(suppl 1):209-221.
57 Kondziolka D, Ong J, Lee JYK, et al. Gamma knife thalamotomy for essential tremor. J Neurosurg. 2008;108:111-117.
58 Rand RW, Jacques DB, Melbye RW, et al. Gamma Knife thalamotomy and pallidotomy in patients with movement disorders: Preliminary results. Stereotact Funct Neurosurg. 1993;61(suppl):65-92.
59 Friedman J, Epstein M, Sanes J, et al. Gamma Knife pallidotomy in advanced Parkinson’s disease. Ann Neurol. 1996;39:535-538.
60 Kwon Y, Whang CJ. Stereotactic Gamma Knife radiosurgery for the treatment of dystonia. 2. Stereotact Funct Neurosurg. 1995;64(suppl 1):222-227.
61 Young RF, Jacques DB, Rand RW, et al. Medial thalamotomy with the Leksell Gamma Knife for treatment of chronic pain. Acta Neurochir Suppl. 1994;62:105-110.
62 Hayashi M, Taira T, Chernov M, et al. Gamma Knife surgery for cancer pain—pituitary gland-stalk ablation: a multicenter prospective protocol since 2002. J Neurosurg. 2002;97:433-437.
63 Hayashi M, Taira T, Chernov M, et al. Role of pituitary radiosurgery for the management of intractable pain and potential future applications. Stereotact Funct Neurosurg. 2003;81:75-83.
64 Leksell L, Herner T, Liden K. Stereotaxic radiosurgery of the brain. Report of a case. Kungl Fysiogr Sallsk Lund Forhandl. 1955;25:1-10.
65 Alexander E, Lindquist C. Special indications: Radiosurgery for functional neurosurgery and epilepsy. In: Alexander E, Loeffler JS, Lunsford LD, editors. Stereotactic Radiosurgery. New York: McGraw-Hill; 1993:221-225.
66 Kihlstrom L, Hindmarsh T, Lax I, et al. Radiosurgical lesions in the normal human brain 17 years after Gamma Knife capsulotomy. Neurosurgery. 1997;41:396-402.
67 Barcia-Salorio JL, Barcia JA, Hernandez G, et al. Radiosurgery of epilepsy. Long-term results. Acta Neurochir Suppl. 1994;62:111-113.
68 Hellstrand DE, Abraham-Fuchs K, Jernberg B, et al. MEG localization of interictal epileptic focal activity and concomitant stereotactic radiosurgery. A non-invasive approach for patient with focal epilepsy. Physiol Meas. 1993;14:131-136.
69 Mori Y, Kondziolka D, Balzer J, et al. Effects of stereotactic radiosurgery on an animal model of hippocampal epilepsy. Neurosurgery. 2000;46:157-168.
70 Mathieu D, Kondziolka D, Niranjan A, et al. Gamma knife radiosurgery for epilepsy caused by hypothalamic hamartomas. Stereotact Funct Neurosurg. 2006;84:82-87.
71 Régis J, Peragut JC, Rey M, et al. First selective amygdalohippocampal radiosurgery for mesial temporal lobe epilepsy. Stereotact Funct Neurosurg. 1995;64(suppl 1):193-201.
72 Bartolomei F, Hayashi M, Tamura M, et al. Long-term efficacy of gamma knife radiosurgery in mesial temporal lobe epilepsy. Neurology. 2008;70:1658-1663.
73 Whang CJ, Kim CJ. Short-term follow-up of stereotactic Gamma Knife radiosurgery in epilepsy. Stereotact Funct Neurosurg. 1995;64(suppl 1):202-208.
74 Pollock B, Kondziolka D. Stereotactic radiosurgical treatment of sphenopalatine neuralgia. J Neurosurg. 1997;87:450-453.
75 Ford RG, Ford KT, Swaid S, et al. Gamma Knife treatment of refractory cluster headache. Headache. 1998;38:3-9.
76 McClelland S3rd, Barnett GH, Neyman G, et al. Repeat trigeminal nerve radiosurgery for refractory cluster headache fails to provide long-term pain relief. Headache. 2007;47:298-300.
77 Donnet A, Tamura M, Valade D, et al. Trigeminal nerve radiosurgical treatment in intractable chronic cluster headache: unexpected high toxicity. Neurosurgery. 2006;59:1252-1257.
78 Lad SP, Lipani JD, Gibbs IC, et al. Cyberknife targeting the pterygopalatine ganglion for the treatment of chronic cluster headaches. Neurosurgery. 2007;60:E580-581.
79 Regis J, Bartolomei F, Meteltus P, et al. Radiosurgery for trigeminal neuralgia and epilepsy. Neurosurg Clin N Am. 1999;10:359-377.