40 Radiofrequency Kyphoplasty: A Novel Approach to Minimally Invasive Treatment of Vertebral Compression Fractures
KEY POINTS
Introduction
Percutaneous treatment of vertebral compression fractures (VCFs) was first performed in France in 1984 by Galibert and Deramond.1 The two most commonly performed minimally invasive VCF procedures are known as vertebroplasty and kyphoplasty. The primary difference is that in kyphoplasty, commonly referred to as percutaneous vertebral augmentation, a cavity using a mechanical device is created before cement delivery.∗ Both procedures have been shown to provide dramatic pain relief in vertebral body fractures associated with underlying osteoporosis or malignancy, and have been successfully applied in cases in which conservative management has failed and surgery is undesirable.1–7, 10–14 Because they have a higher incidence of osteoporosis, most patients referred for this procedure are women. However, men with vertebral body fractures from osteoporosis also present for treatment. Many of the characteristics of the male population with osteoporotic vertebral body fractures have recently been described.4,7 Vertebral body fractures are the most common osteoporotic fractures in men. Like those in women, they are associated with significant morbidity and restriction of activities of daily living.8 The economic impact of osteoporotic fractures was estimated at nearly $2.7 billion in 1995 for men alone,9 making this a substantial health care problem from the standpoint of both cost and morbidity.
Minimally invasive treatment of vertebral compression fractures requires the image-guided insertion of a needle or working cannula through or adjacent to the pedicle into the vertebral body. Acrylic or calcium phosphate bone cement is then injected into the vertebral body (either with or without performing cavity creation) where it solidifies, providing structural support and preventing the movement associated with pain.3,14
The StabiliT Vertebral Augmentation System (DFine Inc., San Jose, CA, USA) is a novel product intended for the treatment of VCFs associated with osteoporotic fractures and tumors of the spine in a procedure known as radiofrequency (RF) kyphoplasty. RF kyphoplasty is designed to minimize leakage, enable height restoration of mobile fractures, and provide pain relief through fracture stabilization by way of site- and size-specific cavity creation and extended, controlled delivery of an ultrahigh viscosity cement. This new percutaneous vertebral augmentation system combines the following unique attributes: navigational cavity creation device; RF energy modulated, ultra-high viscosity cement; unique, hydraulic delivery system; and a remotely controlled delivery mechanism to offer additional control to the physician in treatment of a VCF. The use of RF energy to modulate bone cement polymerization immediately before entering the patient permits the system to maintain cement in a reservoir at ambient temperature with a very long working time, yet deliver cement of a viscosity many times higher than conventionally delivered polymethyl methacrylate (PMMA) cement. This control during the cement delivery results in the potential for reduced venous extravasation and yet retains the ability to move bone fragments and restore height.
Materials and Methods
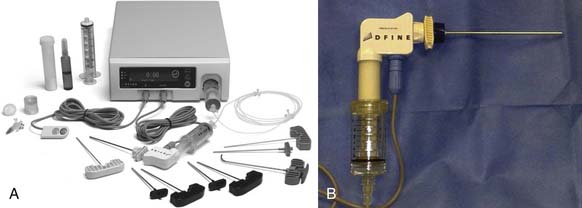
The StabiliT Vertebral Augmentation System
The StabiliT Vertebral Augmentation System is a unique RF controlled cement delivery system for the treatment of vertebral compression fractures. It has been cleared for use in the United States for percutaneous delivery of StabiliT ER (Energy Responsive) Bone Cement in kyphoplasty procedures in the treatment of painful vertebral compression fractures, which may result from osteoporosis, benign lesions (hemangioma), and malignant lesions (metastatic cancers, myeloma). It contains the following components: a proprietary energy-responsive PMMA bone cement (StabiliT ER Bone Cement); a unique vacuum saturation cement mixing system (Saturate Mixing System); a controller (Mulitplex Controller) that contains both a radiofrequency generator and a hydraulic drive; introducer/working cannulae for access to the vertebral body; straight and navigational cavity creation devices to permit specificity of the site and size of the cavity; a PFA (Teflon-like)-lined heating element (Activation Element) and delivery cannulae to permit the delivery of uniquely high viscosity PMMA cement; and a 3-m-long cable to permit remote-control delivery of the cement, thereby controlling the operator’s radiation exposure (Figure 40-1). Following cavity creation using the articulated arm of the MidLine Osteotome, the StabiliT System (DFine Inc., San Jose, CA, USA) preferentially delivers cement to the cavity but further permits interdigitation of the ultra-high viscosity cement into the adjacent trabecular beds (Figure 40-2).
In Vitro Evaluation of Height Restoration and Intravertebral Pressure in Three Minimally Invasive Procedures Using an Osteoporotic Cadaver Bone Model
The potential to restore height in mobile vertebral compression fractures and the possible impact on intravertebral pressure have been reported in various studies.17,18 Cadaver spines obtained from women between 66 and 87 years of age were used. The specimens in each study had bone mineral densities (BMDs) of 0.687 ± 0.136 g/cm3 and 0.707 ± 0.136 g/cm3 respectively. Individual vertebral bodies (VBs) were prepared by transecting the pedicles and removing all disc material from the endplates. Cephalac and caudal surfaces of each vertebral body were rigidly embedded in a urethane potting compound (Smooth ON, Easton, Penn.).
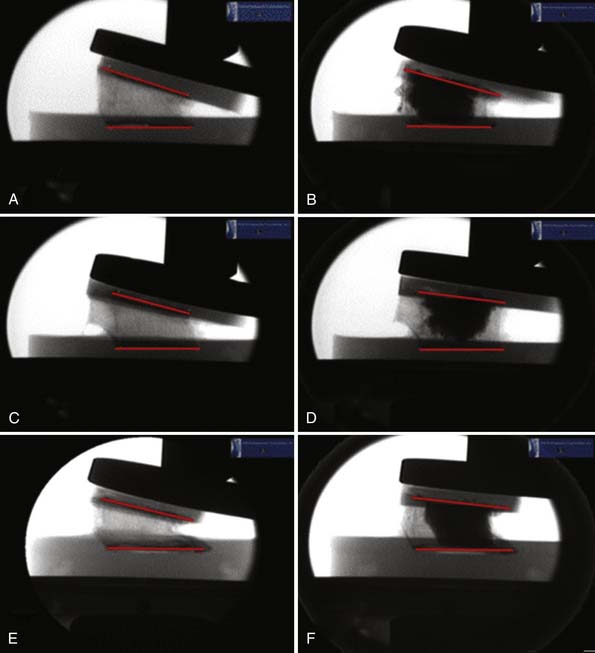
Each vertebral body was mounted in a custom semiconstrained fixture and rigidly attached to a servohydraulic load frame (8521S, Instron Corp, Canton, Mass.). A 500-N offset load was applied to the specimen and a radiograph taken to determine prefracture anterior vertebral body height (GE OEC Diasonics Model 9000, Fairfield, Conn.). Offset loads were applied at a displacement rate of 5 mm/min with a data acquisition rate of 20 Hz. Monotonic testing was performed until the height of the vertebral body had been reduced by 30%. Postfracture height was determined using radiographic images under a 500-N compressive offset loads. Each treatment, conventional balloon kyphoplasty (BKP) (KyphX, Medtronic Inc., Memphis, Tenn.), RF kyphoplasty (RFK) (StabiliT Vertebral Augmentation System) and vertebroplasty (Vertebroplastic, DePuy Spine Inc., Raynham, Mass.), was performed on randomly assigned vertebral bodies.
All three procedures (BKP, RFK, and vertebroplasty) were utilized by physicians skilled in these minimally invasive techniques. Standard bipedicular technique was used in the BKP specimen. RFK was performed using a unipedicular technique and the MidLine Osteotome. A total of 6 ml bone cement was used in all specimens. After each treatment, vertebral bodies were incubated in a 37° C water bath for a minimum of 2 hours before posttreatment radiographic evaluation. Posttreatment radiographs were taken while a 500-N offset load was applied to the specimen. Anterior height was measured from the prefracture, postfracture, and posttreatment radiographs using Photoshop (Adobe Systems, Inc., San Jose, Calif.). Each measurement was done by five different individuals blinded to the treatment performed on the specimens (Figure 40-3). Statistical comparisons between the treatment groups were performed, and statistical significance was defined as p < .05. In one of the studies, a pressure transducer was placed into the venous plexus through the posterior cortex to measure the intravertebral pressure during cement delivery.
Results
A significant difference in height was found between the prefracture and postfracture specimens for all three groups. Mechanical VCF height elevation equivalent to that observed in BKP was achieved using RFK. In contrast, conventional vertebroplasty procedure, in which cement simply fills existing VCF voids before extravasation via the path of least resistance, was unable to restore comparable height. The mean anterior height restorations for the conventional BKP, RFK, and vertebroplasty systems were 74.8 ± 9.4%, 83.7 ± 17.5%, and 32.8 ± 8.1%, respectively.17 There was no significant difference between the BKP and RFK groups (p = .40). The BKP and RFK procedures both restored significantly more height than that achieved with the vertebroplasty procedure (p ≤ .001 and p ≤ .002 respectively). The mean maximum intravertebral pressures recorded during RFK, BKP, and vertebroplasty were 9.8 ± 0.1 kPa, 9.8 ± 0.0 kPa, and 14.7 ± 9.7 kPa, respectively. Wilcoxon signed rank tests did not yield any significant differences between the RF kyphoplasty and vertebroplasty (p = .5), balloon kyphoplasty, and vertebroplasty (p = 1.0) or RF kyphoplasty and balloon kyphoplasty (p = 1.0) treatment groups.16 These data demonstrate that the use of an ultra-high viscosity cement and an appropriate delivery system can provide an alternative to currently available methods to restore height in a VCF without adverse increases in intravertebral pressure.
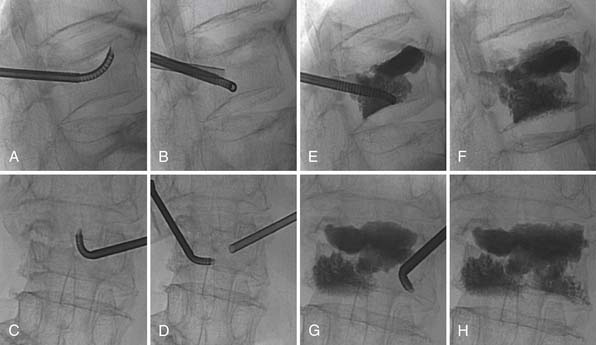
RF Kyphoplasty Clinical Experience with the Stabilit Vertebral Augmentation System
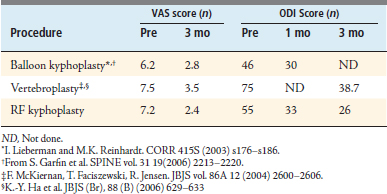
To date, over 2000 vertebral levels and 1200 RF kyphoplasty cases have been performed using the StabiliT Vertebral Augmentation System. No cement-related symptomatic adverse events have been reported to date. The procedure involves a site-specific cavity creation using the MidLine Osteotome under fluoroscopic guidance, followed by controlled delivery of an ultra high viscosity cement (Figure 40-4). The ultra-high viscosity cement preferentially fills the site-specific cavity before driving into the fracture planes and interdigitating into the adjacent trabeculae. Because only the cement that is delivered into the patient is exposed to RF energy, cement delivery can be delayed for extended periods of time if need be to minimize extravasation in cases of large fractures planes or lytic lesions. The initial clinical experience included a prospective controlled clinical trial performed under an Ethics Committee–approved protocol at three sites in two countries (Hungary and Austria) and performed by physicians of three disciplines: neurosurgery, interventional radiology, and orthopedic surgery. Patients in this study (SPACE—Spinal Augmentation with Cement and Energy) were eligible for enrollment if they had one to three vertebral fractures from T7 through L5. Clinical results of the first 104 fractures in 73 patients treated to date with the StabiliT system were reported in the 2009 Scientific Meeting of the Society for Interventional Radiology.17 The study demonstrated pain relief (measured by visual analogue scale [VAS]) and improved function (measured by Oswestry Disability Index [ODI]) consistent with published data for conventional balloon kyphoplasty and vertebroplasty (Table 40-1). As has been reported for conventional balloon kyphoplasty and vertebroplasty, RF kyphoplasty reduced pain scores greater than 50% when measured by the VAS, a validated instrument.
TABLE 40-1 Clinical Results from the European Prospective Clinical Trial with the StabiliT Vertebral Augmentation System Compare Favorably with Previously Documented Pain Relief and Functional Scores for Conventional Balloon Kyphoplasty and Vertebroplasty
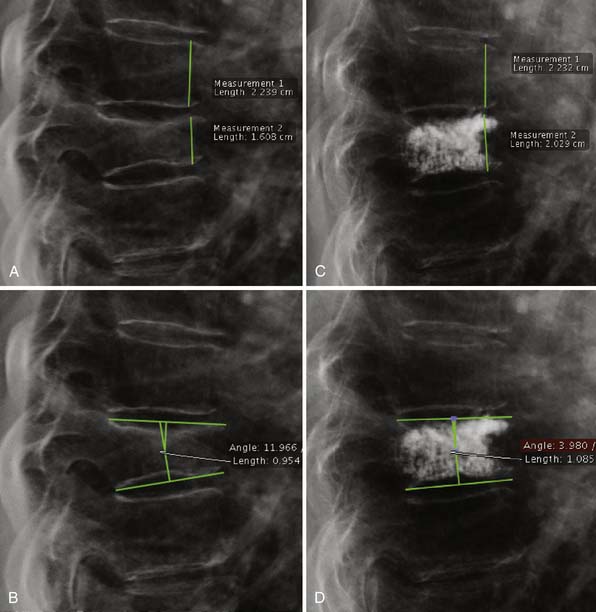
Additionally, in a series of 20 VCFs in 14 patients, Elgeti reported height restoration and kyphosis correction in 50% of the fractures, with an average height restoration of 4 mm and kyphosis correction of 5.6 degrees (Figure 40-5).18
Discussion
Since 1984, technology has converged in a way that impacts the traditional use of the term kyphoplasty. Initially kyphoplasty was defined as the “balloon procedure.” Today, there are additional technologies designed for minimally invasive, cavity creating VCF treatment. Consequently, procedure terminology has evolved, as evidenced by CMS recently replacing the ICD-9 code title of “Kyphoplasty” with “Percutaneous Vertebral Augmentation,” with examples of this procedure category including conventional kyphoplasty and other various technologies commercially available at the time of publishing, included in the description. High viscosity cement has the ability to combine the minimalism of vertebroplasty with the mechanical potential benefits of a vertebral implant or balloon. Our data show an ability to deliver cement in a more controlled manner and to create height-restorative forces based on location and the cohesive properties of the cement. Ultimately this new method will find its place in a modern buffet of options for repair of these VCFs with benefits for the patient and simplicity for the physician.
1. Galibert P., Deramond H., Rosat P., et al. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie. 1987;33(2):166-168. French
2. Zoarski G.H., Snow P., Olan W.J., et al. Percutaneous vertebroplasty for osteoporotic compression fractures: quantitative prospective evaluation of long-term outcomes. J. Vasc. Interv. Radiol.. 2002;13:139-148.
3. Weill A., Chiras J., Simon J.M., et al. Spinal metastases: indications for and results of percutaneous injection of acrylic surgical cement. Radiology. 1996;199:241-247.
4. Cotton A., Dewatre F., Cortet B., et al. Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up. Radiology. 1996;200:525-530.
5. McGraw J.K., Lippert J.A., Minkus K.D., et al. Prospective evaluation of pain relief in 100 patients undergoing percutaneous vertebroplasty: results and follow-up. J. Vasc. Interv. Radiol.. 2002;13:883-886.
6. Evans A.J., Jensen M.E., Kip K.E., et al. Vertebral compression fractures: pain reduction and improvement in functional mobility after percutaneous polymethylmethacrylate vertebroplasty retrospective report of 245 cases. Radiology. 2003;226(2):366-372.
7. Vasconcelos C., Gailloud P., Beauchamp N.J., et al. Is percutaneous vertebroplasty without pretreatment venography safe? Evaluation of 205 consecutive procedures. AJNR Am. J. Neuroradiol.. 2002;23(6):913-917.
8. O’Neill T.W., Felsenberg D., Varlow J., et al. The prevalence of vertebral deformity in European men and women: the European vertebral osteoporosis study. J. Bone Miner. Res.. 1996;11:1010-1018.
9. Ray N.F., Chan J.K., Thamer M., et al. Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. J. Bone Miner. Res.. 1997;12:24-35.
10. McGirt M.J., Parker S.L., et al. Vertebroplasty and kyphoplasty for the treatment of vertebral compression fractures: an evidenced-based review of the literature. Spine J.. 2009;9:501-508.
11. Lieberman I.H., Dudeney S., Reinhardt M.K., et al. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001;26(14):1631-1638.
12. Garfin S.R., Yuan H.A., Reiley M.A. Kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001;26:1511-1515.
13. Truumees E., Hilibrand A., Vaccaro A.R. Percutaneous vertebral augmentation. Spine J.. 2004;4:218-229.
14. Resnick D.K., Garfin S.R. Vertebroplasty and kyphoplasty. New York: Thieme; 2005.
15. K. Murphy, E.Wong, R. Poser, et al., Comparison of intravertebral pressure and height restoration in three minimally invasive treatments of vertebral compression fractures. 2009 SIR Annual Scientific Meeting, Abstract #34.
16. Raley T., Poser R., Kohm A. Comparative Height restoration of three vertebral augmentation systems for treatment of vertebral compression fractures. 55th Annual Meeting of the Orthopedic Research Society. 2009:0639.
17. L. Miko, I. Szikora, J. Grohs, et al., Initial clinical experience with radio-frequency based vertebral augmentation in treatment of vertebral compression fractures. 2009 SIR Annual Scientific Meeting, Abstract #35.
18. Fourth Symposium Vertebroplastie/Kyphoplastie. 26 September 2009. Potsdam, Germany.
∗ AMA Current Procedural Terminology (CPT) 2009 for Vertebral Augmentation Procedures reads: “Percutaneous vertebral augmentation, including cavity creation (fracture reduction and bone biopsy included when performed) using mechanical device, one vertebral body, unilateral or bilateral cannulation (e.g., kyphoplasty)”. ICD-9-CM procedure code addendum (ICD-9 CM 2009 Volumes 1 & 2) for Percutaneous Vertebral Augmentation reads: Insertion of inflatable balloon, bone tamp, or other device displacing (removing) (compacting) bone to create a space (cavity) (void) prior to the injection of bone void filler (cement) (polymethylmethacrylate) (PMMA) or other substance.