Vessels within zone may appear normal (no mass effect)
• Region of radiation damage that is hypodense on portal venous phase may become hyperdense with prolonged enhancement on delayed phase
• MR, especially T1WI with in- and opposed-phase GRE, is best means of distinguishing RILD from steatosis
 , following external radiation therapy for lymphoma.
, following external radiation therapy for lymphoma.
 in the left lobe due to external radiation therapy for esophageal carcinoma. Note the normal appearance of the left hepatic vein
in the left lobe due to external radiation therapy for esophageal carcinoma. Note the normal appearance of the left hepatic vein  within the zone of radiation-induced liver disease (RILD).
within the zone of radiation-induced liver disease (RILD).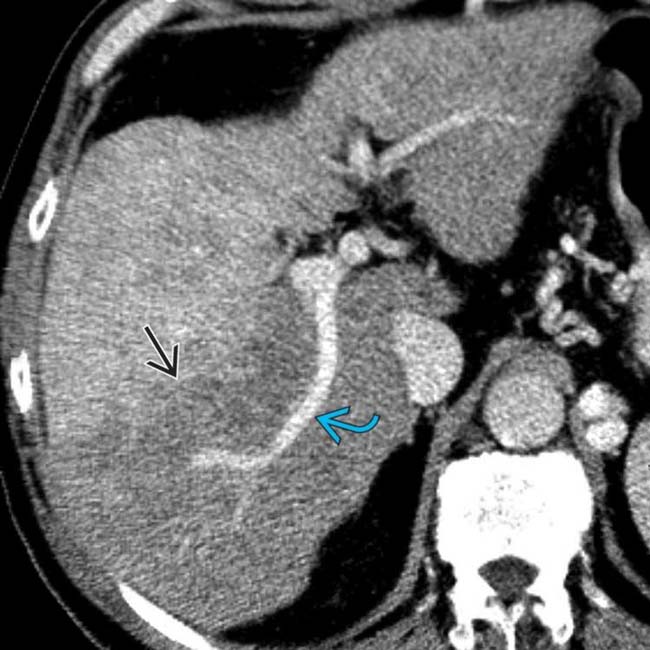
 corresponding to the segments that had received yttrium-90 microsphere embolization for hepatocellular carcinoma (HCC). Note the normal appearance of the posterior right portal vein
corresponding to the segments that had received yttrium-90 microsphere embolization for hepatocellular carcinoma (HCC). Note the normal appearance of the posterior right portal vein  within the damaged liver.
within the damaged liver.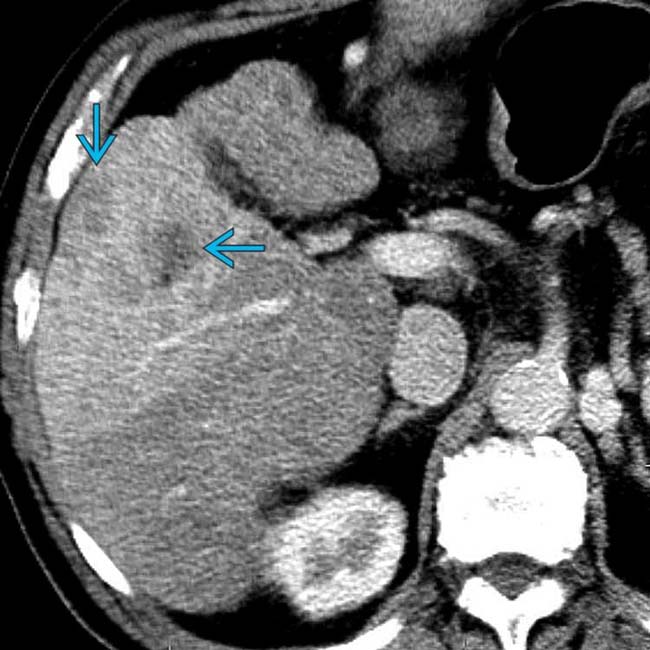
 .
.IMAGING
General Features
CT Findings
• NECT

 in a 66-year-old man with HCC, prior to the onset of therapy.
in a 66-year-old man with HCC, prior to the onset of therapy.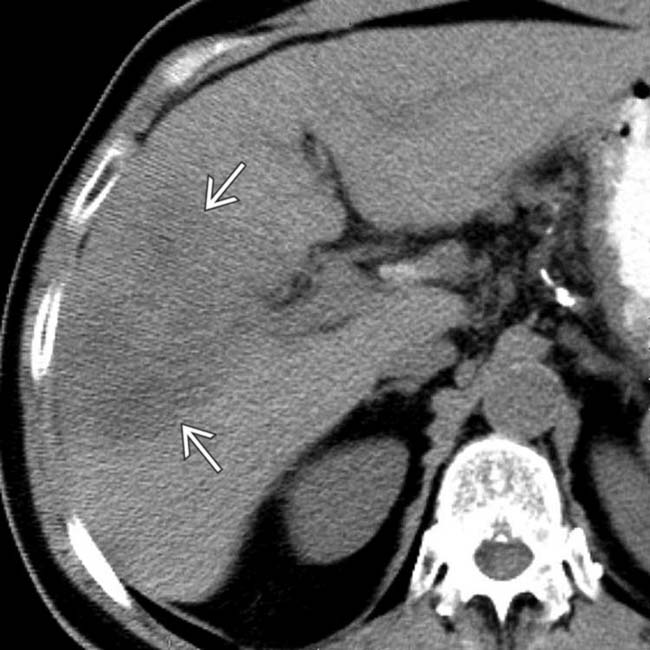
 in the distribution of the right anterior hepatic artery in which the radioactive microspheres had been placed.
in the distribution of the right anterior hepatic artery in which the radioactive microspheres had been placed.
 .
.
 is less vascular than on pretreatment images. Note persistence of the straight line of demarcation
is less vascular than on pretreatment images. Note persistence of the straight line of demarcation  of the treated segment of liver.
of the treated segment of liver.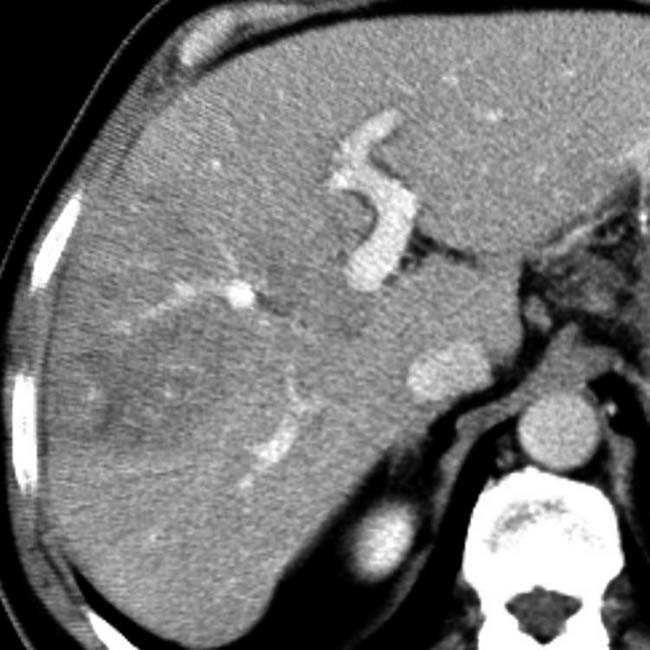
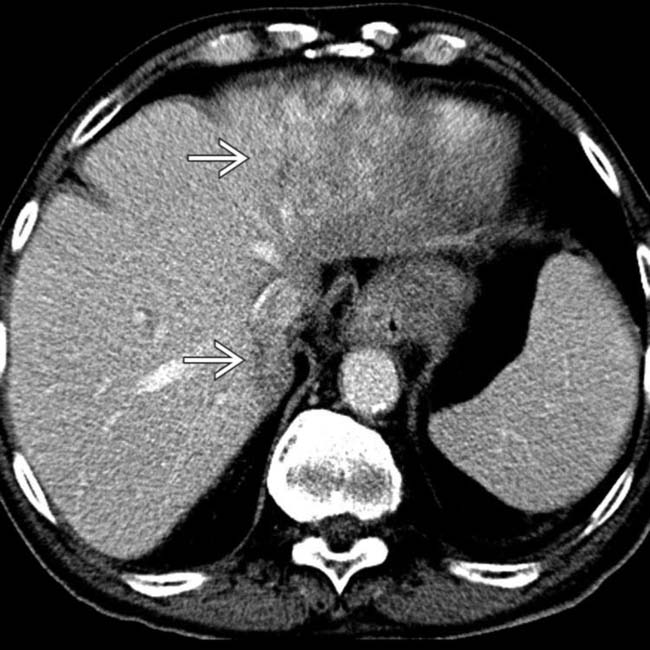
 corresponding to the radiation therapy port.
corresponding to the radiation therapy port.
 , not corresponding to any anatomical divisions of the liver, all due to radiation hepatitis.
, not corresponding to any anatomical divisions of the liver, all due to radiation hepatitis.
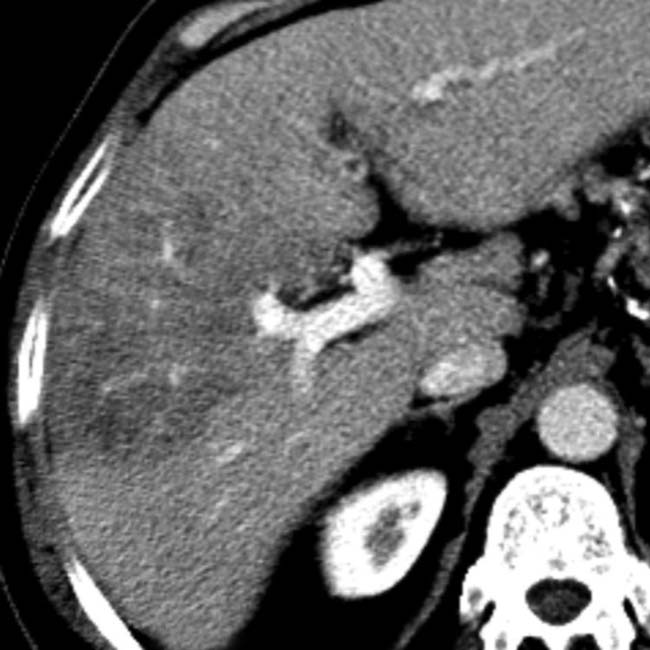
 from nasopharyngeal carcinoma shows a peculiar low-attenuation band through the center of the liver
from nasopharyngeal carcinoma shows a peculiar low-attenuation band through the center of the liver  . Note the lack of mass effect on the large hepatic and portal vein branches traversing this zone.
. Note the lack of mass effect on the large hepatic and portal vein branches traversing this zone.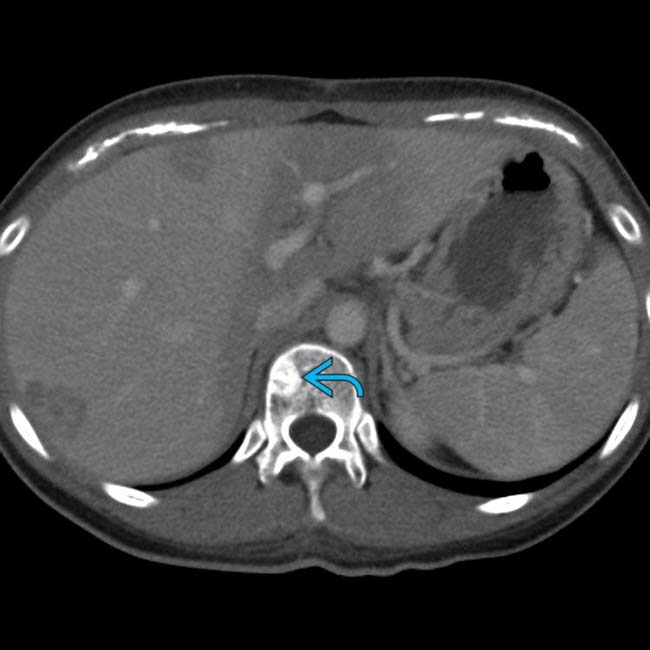
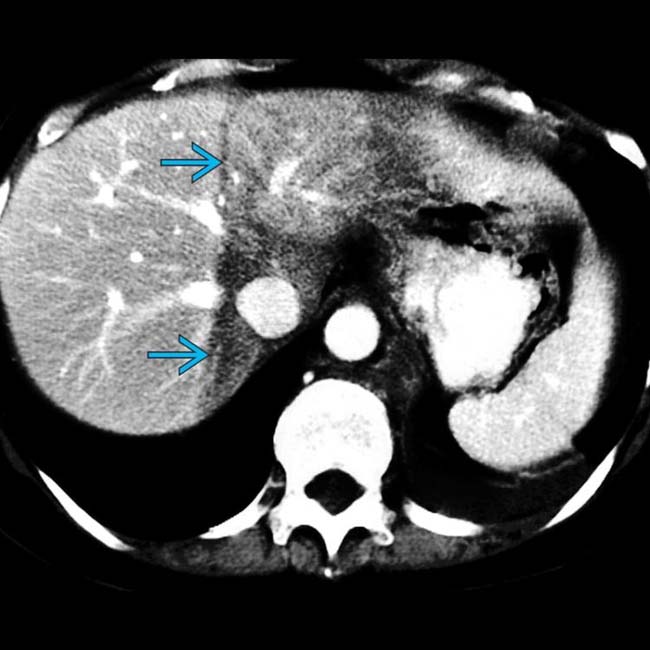
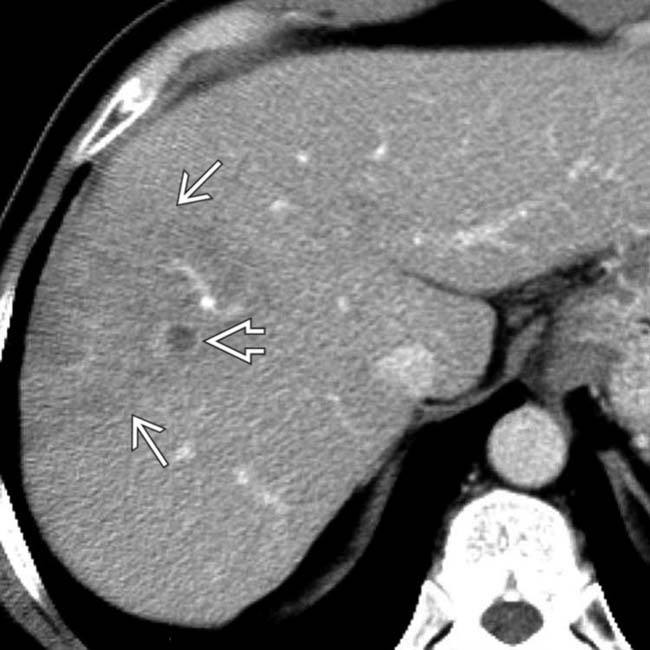
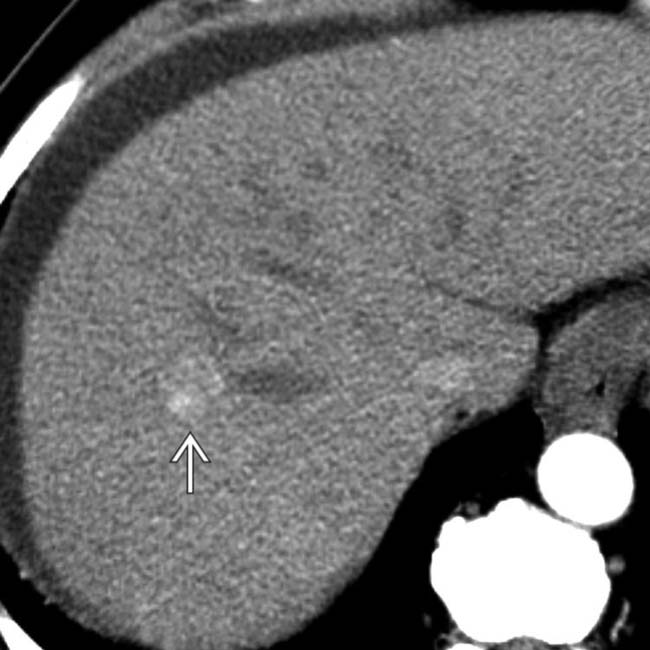
 that had been treated with external beam radiation therapy.
that had been treated with external beam radiation therapy.
 that represents radiation-induced injury. Again, note the lack of mass effect on vessels within the injured liver, as well as hepatic metastases
that represents radiation-induced injury. Again, note the lack of mass effect on vessels within the injured liver, as well as hepatic metastases  .
.
 , the latter representing the effects of chemotherapy rather than the radiation therapy.
, the latter representing the effects of chemotherapy rather than the radiation therapy.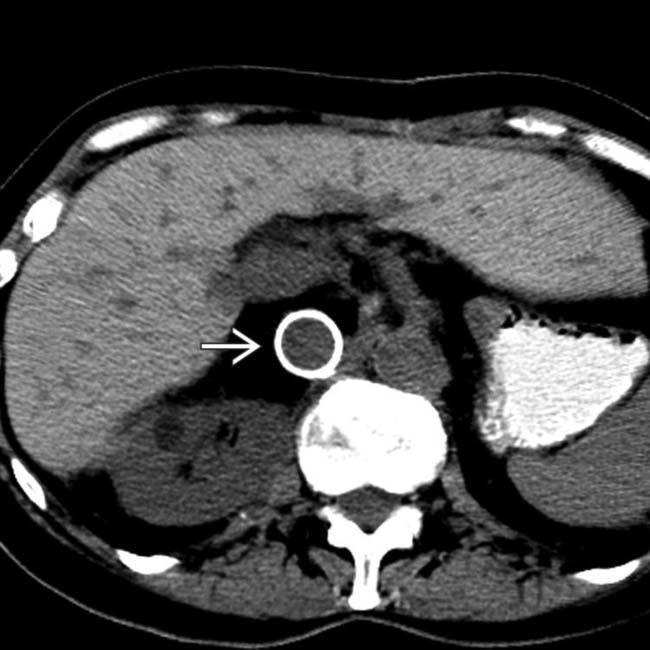
 .
.
























 enhancing during the arterial phase, demonstrating hepatocellular carcinoma.
enhancing during the arterial phase, demonstrating hepatocellular carcinoma.