CHAPTER 24 Radial Head Fracture
PART A General Considerations, Conservative Treatment, and Open Reduction and Internal Fixation
INTRODUCTION
HISTORICAL REVIEW
Before 1933,10 the literature has been well summarized by Schwartz and Young.110 The first description was probably made by Paul of Aegina (ad 625-690): “The ulna and radius are sometimes fractured together and sometimes one of them only, either in the middle or at one end as at the elbow or the wrist.”2 Early difficulty in making the diagnosis was encountered because of “thick muscle covering.”33,93 In 1891, Hoffa described two types of radial head fractures, displaced and undisplaced.55 Hoffa55 and Helferich50 recommended resection of the radial head for late deformity.
Three to 4 weeks of immobilization,122 passive motion, avoidance of “operative interference,”45 removal of the fracture fragment, and excision of the entire head for severe comminution54 were all recommended in the early 1900s. The first descriptions of a successful osteosynthesis of the fractured radial head was by Albin Lambotte in 1909.71 Other pertinent contributions include the suggestion that surgery is not a matter of election but rather of selection.54 Although much subsequently has been written about this fracture, the focus has changed to the more complex fractures.16,30,67
BIOMECHANICS AND FUNCTION OF THE RADIAL HEAD
Force Transmission
Studies in our laboratory have shown that, under the most demanding of circumstances, up to about 90% of body weight can be demonstrated across the radial head.84 The greatest amount of force transmission occurs with the forearm in pro-nation. This is because of a screw-home mechanism that occurs during pronation with proximal radial migration.
Stability
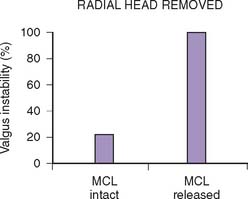
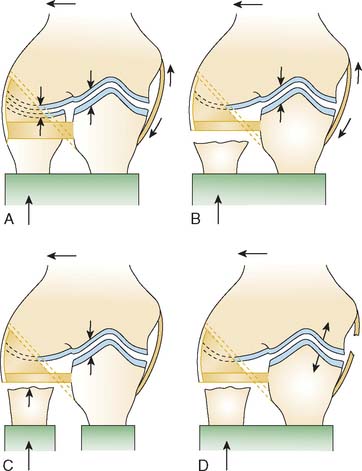
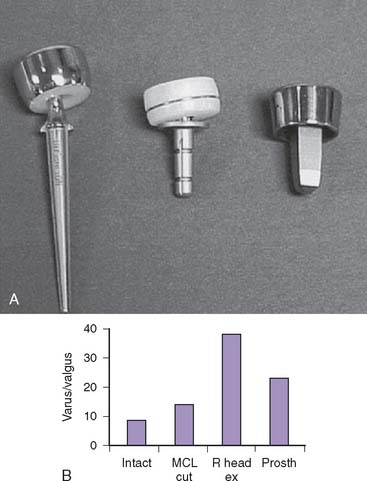
Traditional force-displacement studies have attributed 30% of the resistance to valgus stress to the radial head.57,83,96 Our studies have shown no significant resistance to valgus stability when the medial collateral ligament is intact. On the other hand, if the medial collateral ligament is deficient, the radial head is an important secondary stabilizer in preventing the elbow from dislocating.85 Other investigators115 have also shown a complementary relation of the lateral collateral ligament to the competency of the annular ligament. Therefore, the radial head may be considered a secondary stabilizer to valgus stress, and it does provide an important contribution to joint force transmission (Fig. 24-1).
INCIDENCE OF FRACTURE
Fracture of the radial head and neck has been variously reported as 1.7% to 5.4% of all fractures.27,66,86 Radial head fractures occur in about 17% to 19% of cases of elbow trauma134,137 and account for about 33% of elbow fractures.77 Approximately one in three cases is associated with another injury.127
Age and Sex
In general, about 10% to 15% of these fractures involve the neck,86,122,127 usually in children in whom the physis has not closed.15 Recent demographic data127 from our institution suggest some changes when compared with previously published reports.5,22,23,29,30,135 Gender ratio is approximately 1:1. The male population has more severe fracture types and more often sustain associated injuries. Compared with the literature,22,23,29,30 the age of patients sustaining radial head fractures has increased to a mean age of 45 years, 48 years old for women and 41 years for men.127
MECHANISM OF FRACTURE
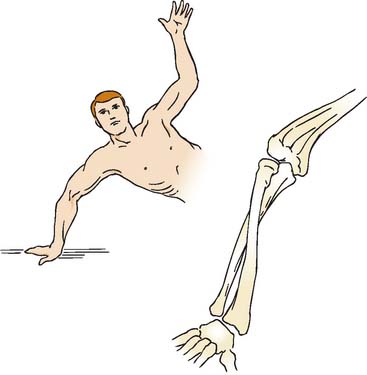
An axial load on the pronated forearm consistently produces a fracture of the radial head similar to that seen in clinical experience (Fig. 24-2).122 Odelberg-Johnsson88 observed precisely the same effect, noting that the fracture (1) occurred with posterior subluxation of the “forearm as far as the ligaments allowed,” and (2) involved the most anterior portion of the radial head when the forearm was pronated. Because the head of the radius is eccentric to the central axis of the neck,118 the posterolateral aspect of the radial head comes into intimate contact with the capitellum during pronation. The common occurrence of an anterolateral fracture fragment supports this theory.29,66 A direct blow is another uncommon cause of radial head fracture.29,41
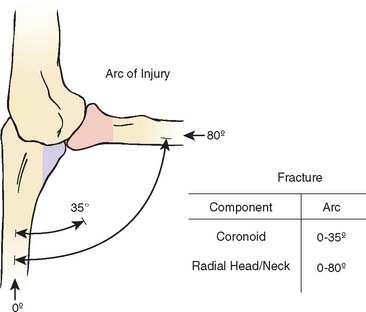
Amis and Miller3 recently enhanced our understanding of this and other fractures by correlating the fracture and the angle of flexion (Fig. 24-3). As is seen experimentally, either the coronoid or radial head may be fractured with the elbow in full extension, but the radial head can be fractured at greater degrees of flexion, approaching 80 degrees of the flexion arc.
ASSOCIATED INJURIES
CONCURRENT FRACTURES ABOUT THE ELBOW
Based on our assessment of 333 radial head fractures seen at the Mayo Clinic, we observed that the likelihood of associated injuries strongly correlates with the severity of the radial head fracture.127 The incidence of associated injuries increases from 20% in nondisplaced fractures to 80% in comminuted radial head fractures. The vast majority of these injuries (90%) are fractures about the elbow, mostly articular surface lesions. Approximately 20% of these articular injuries include the distal humerus, whereas in more than 90%, the proximal ulna is involved.
Fractures or cartilage injuries of the capitellum are common101,133 but not always appreciated.19 The associated fracture of the capitellum has been studied in some detail by Ward and Nunley.132 About one half of capitellar fractures were shown to have associated radial head fractures, whereas approximately 2% of radial head fractures had associated capitellar fractures. Thus, this combination is rather rare.127,132
Fracture of both the olecranon and the radial head is usually considered a variety of the Monteggia fracture and has been analyzed in detail by Scharplatz and Allgower108 and others.44,70,94,112
In 15% of patients, the radial head fracture is complicated by a coronoid fracture.127 Fractures of the coronoid have been discussed in detail by Regan and Morrey.100 If the fragment is large, significant elbow instability may occur.47,101,112
In our series, an elbow dislocation was found in about 15% of radial head fractures,127 as compared with approximately 10% quoted in the literature.1,7,27,29 Combined radial head and coronoid fractures are commonly seen in elbow dislocations. The coronoid process is involved in 80% of patients that sustain a radial head fracture as part of an elbow dislocation.
Bilateral radial head fractures are uncommon and occur in about 2% of patients.29,127
LIGAMENTOUS INJURY AT THE ELBOW
Some degree of ligamentous injury often occurs with radial head fracture; this association is not always fully appreciated (Fig. 24-4).17,49,65,88,133 An incompetent ulnar collateral ligament is suggested by an increased valgus position.22,86,109
Approximately 50% of associated lesions to the elbow involve clinically significant ligamentous injuries. About 10% of patients are diagnosed with a lateral or medial collateral ligament rupture, or a combination of both.127 These clinically relevant injuries are markedly less common than previously described.
Wagner130 observed 24 patients with calcification in the medial collateral ligament, and Arner and associates5 described a 12% incidence of ulnar collateral ligament calcification. Arvidsson and Johansson6 found ligament or capsular disruption by arthrography with various types of radial head fractures. Johansson65 demonstrated positive arthrographic findings in 4% of type I, 21% of type II, and 85% of type III injuries. Using magnetic resonance imaging in patients with types II or III radial head fractures, Itamura and associates63 recently found lesions in the medial collateral ligament in 54%, lateral ulnar collateral ligament in 80%, and lesions of both ligaments in 50%.
OTHER INJURIES
About 10% of patients with a radial head fracture sustain associated injuries other than elbow injuries. Fractures of the hand or wrist are found in about 6%.127 Conversely, radial head fractures are found in 6% of all scaphoid fractures.136 Shoulder injuries are uncommon (2%) and are usually found in nondisplaced radial head fractures.127
A ligamentous injury sustained at the distal radioulnar joint at the time of the radial head fracture15,28,116 is diagnosed in less than 1% of acute cases128 but is well recognized as the Essex-Lopresti injury and has been the subject of several reports.36,46,124 Shortening of 5 to 10 mm can be anticipated (Fig. 24-5).46 Open reduction and internal fixation to stabilize the proximal radius is recommended. Trousdale and associates125 reviewed Mayo experience with 20 patients. Fifteen had radial head resection without knowledge of the wrist injury. Such late detection was treated by reconstructive procedures, with a success rate of only 14%. Proper initial diagnosis was associated with an 80% satisfactory outcome and early treatment.
CLASSIFICATION OF FRACTURE
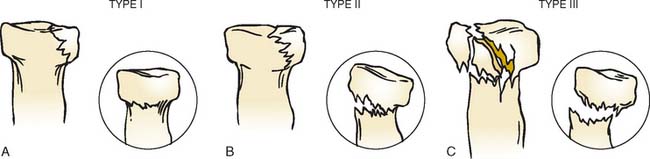
The first classifications of radial head fractures were described by Speed in 1924117 and Eliason in 1925.37 A year later, Cutler reported a second classification29 and this presented the basis for all currently used classifications. The most commonly used classification of radial head fracture is that proposed by Mason (Fig. 24-6).77 A fourth type, the fracture dislocation, was added by Johnston.66 In 1962, Johansson65 added the degree of displacement to his classification and this was later combined with the original Mason classification to form the most recent adaptation of the original Mason classification.57
MAYO MODIFICATION OF MASON CLASSIFICATION
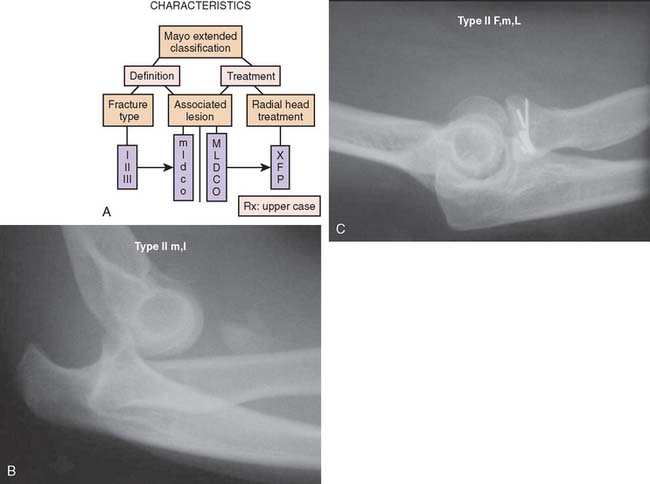
In the previous versions of this book, Morrey added a degree of sophistication to Mason’s classification of radial head fractures by dividing them into simple and complex fractures, depending on associated lesions.81,82 However, the division between simple and complex fractures can sometimes be difficult, for example, when suspected ligamentous lesions are not formally investigated due to the limited clinical implications.
Therefore, based on our clinical experience of more than 333 cases, we propose to add a suffix to the original fracture type in order to quantify associated lesions about the elbow.129
A suffix m is used if a medial collateral ligament injury is suspected or proven, but this has questionable impact on elbow stability. A capital M is used if there is an impact on stability, enough to warrant treatment. For lateral ligament injuries, l and L is used respectively. The same is done to document associated fractures to the ulna (U, u) or humerus (H, h). The suffix P is used to indicate that some sort of procedure was performed (Fig. 24-7); x for excision and F for ORIF.
FRACTURE MANAGEMENT
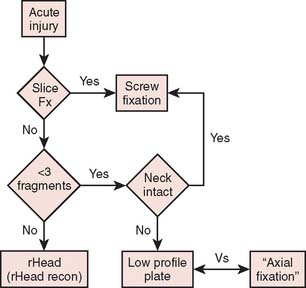
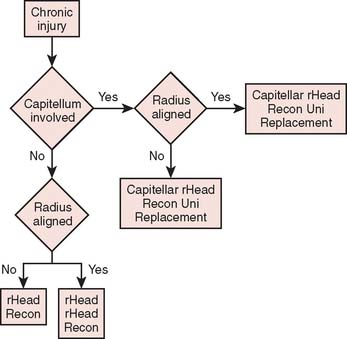
In general, the treatment of radial head fractures is based on the fracture type and the presence of any associated injury. These injuries involve the ligaments or articular elements with variable implications to prognosis and management (Fig. 24-8). Associated injuries should be treated on their own merit, and the following discussion will be limited to the treatment of the radial head fracture as such.
Clinical findings include hemarthrosis and painful rotation of the forearm, especially with palpation of the radial head. Radiographs are not always conclusive, but an elbow fat pad effusion in an otherwise normal radiograph is indicative of an occult radial head fracture in almost 90% of patients89 (Fig. 24-9). Computed tomography scanning may give additional information on the morphology of the fracture57,126 and may aid in planning and assessing the feasibility of a surgical reconstruction (Fig. 24-10).
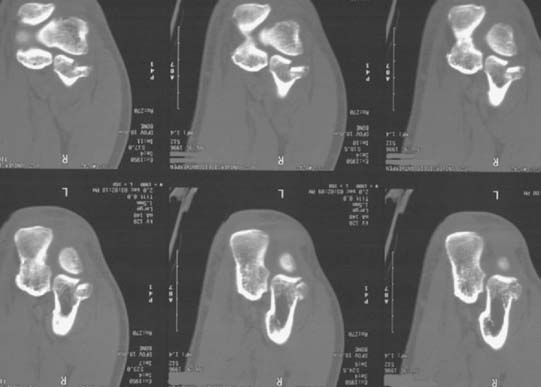
FIGURE 24-10 The computed tomography scan is extremely helpful to diagnose subtle associated articular injuries.
CONSERVATIVE TREATMENT
Conservative treatment of nondisplaced53 or minimally displaced radial head fractures52 has been shown to yield good results at a long-term follow-up of 21 and 19 years, respectively. Results of conservative treatment of displaced radial head fractures are less favorable, and patients have increased pain and decreased strength when compared with surgically managed patients.68,120
Sedation,111 mobilization,* or immobilization with78,98,114 or without111 a plaster cast have been advocated as conservative treatment options. Minor soft tissue injuries rarely need to be addressed.65,78,135
There is little question that the type I fracture (Fig. 24-11), because of its favorable prognosis and lack of concurrent soft tissue or other osseous injury, should be managed with early motion. Mason and Schutkin,76 reporting a military experience, found a mean period of disability of 4 weeks in 18 patients treated with early motion, compared with 7 weeks in seven individuals treated with 3 weeks of immobilization. Immediate mobilization is recommended, but a delay of up to 5 days has no functional implication after a 4-week follow-up.74
The major residuum is loss of extension rather than pain.29 Mason77 reported that about one third of his 62 patients with this fracture lost an average of 7 degrees of extension. This may be associated with hemarthrosis of the joint. In a cadaveric study, McGuigan and Bookout80 demonstrated a decrease in the flexion arc of 2 degrees per milliliter fluid injected into the elbow joint. To facilitate immediate motion, aspiration of the joint, is therefore recommended32,34,40,56,97 and pain relief could be increased by infiltrating some local anesthetic into the joint.27
The most frequent complication of conservative treatment of nondisplaced radial head fractures is degeneration of the articular surfaces, which is found at long-term follow-up in about 80% of patients.52,53 Other complications include displacement or nonunion102 (Fig. 24-12). Delayed excision of the entire radial head can be considered only if any of these complications become symptomatic (Fig. 24-13).26,52,53,102 Among 21 patients treated with delayed excision at the Mayo Clinic, Broberg and Morrey13 reported 75% with decreased pain and 77% with improved motion. The time to delayed excision ranged from 1 month to 20 years (Fig. 24-14).
A rare complication of nondisplaced radial head fractures treated conservatively is arthrofibrosis, which reportedly can be managed successfully with arthroscopic débridement.18,72
RESECTION OF THE RADIAL HEAD
The authors consider this issue somewhat controversial and unresolved. In general, resection is reserved for uncomplicated type III fractures (Fig. 24-15). Rochwerger and colleagues104 compared the treatment of 22 type II fractures. With mean surveillance of 5 years (2 to 23 years), osteosynthesis was found to be superior to resection, as the latter had satisfactory results in just more than 50% of cases. Similar results were found in 28 patients with type III, comminuted radial head fractures. Using a meticulous surgical technique, Ikeda et al60,61 found improved results in the group treated with open reduction and internal fixation (ORIF) over the group of patients treated with resection of the radial head.
Janssen et al64 reported 20 of 21 excellent or good results between 16 and 30 years after excision for comminuted radial head fractures. These investigators did exclude known dislocations. On the other hand, Sanchez-Sotelo et al106 described excision in the face of 10 dislocations, which is consistent with a Mason type IV classification. In this group, nine of 10 were considered satisfactory, similar to that of Janssen. However, they did note a 5-degree increased valgus carrying angle and early asymptomatic degenerative changes of the ulnohumeral joint with a mean of about 4.5 years surveillance (Fig. 24-16). There have been other recent reports regarding excision without radial head replacement that have yielded surprisingly consistent outcomes. A study from Scandinavia of 61 resections noted that the timing of the resection, whether acute or delayed, was much less important than the Mason classification of the lesion. Similar observations were made from Asia by Ikeda, who reported good results at 10 years after 15 patients (four with type II and 11 with type II treated by excision). They did, however, notice that pain was present in about a third of these patients52a and, as noted above, favor fixation.60,61 Wallenbock et al. evaluated radial head resection in 23 instances with a mean follow-up of 17 years with personal evaluation of the entire sample. They demonstrated that 22 of 27 patients had a satisfactory outcome. They observed those with resection after a type III or IV did less well than after a type II fracture. Interestingly, there was no distinction in their group and their observations whether the patients were treated by excision in the early or in the more chronic period.131 Similarly, a report from Italy by Celli of 31 fracture-dislocations noted that only 40% were satisfactory and 60% were unsatisfactory after various treatment options.24 This is consistent with Herbertsson’s observations that the fracture type has greater prognostic importance than the acuteness of the treatment.
The basic treatment rationale, therefore, of simple resection for those fractures that cannot be reduced and fixed does have some merit. This was well summarized by Wallenbock and Potsch,131 who stated that resection is recommended “as long as there are no better long-term results of prosthetic substitution of the radial head.” We hope that prosthetic substitution will prove valuable and effective. However, realistically the long-term follow-up data of those treated by resection certainly justify consideration of this as a treatment option, particularly in those that do not have an associated injury.
OPEN REDUCTION AND INTERNAL FIXATION
Surgical treatment of displaced radial head fractures has evolved from excision of fracture fragments or the entire head of the radius, to several techniques of ORIF and modern types of radial head replacement. ORIF was used sporadically in the past, largely because of the perception that it had “not proved successful in anyone’s hands.”98 The poor earlier results were probably due to an inadequate understanding of anatomy and less refined techniques for effective internal fixation.
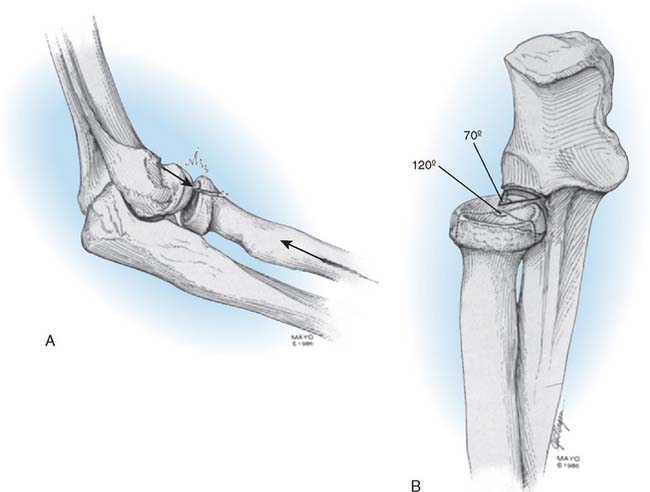
The fracture fragment frequently has a periosteal hinge, indicating that its viability is possible.48 The ideal fracture for fixation is a simple, large (constituting 30% of the head) fragment that involves the anterolateral margin of the head (Fig. 24-17). However, despite the bigger technical challenge of fixing smaller fragments, biomechanical studies have also shown a benefit of fixation of fragments smaller than one third of the radial head.8,9 The anterolateral margin of the head does not articulate with the lesser sigmoid notch; instrumented fixation of this fragment does not result in impingement (Fig. 24-18).20,113 If there are multiple but large fragments, open reduction can still be performed,48 but results can be disappointing.69,103
In general, experience with ORIF is satisfactory in more than 90% of cases.38,91,95,99,103,111
Geel and coworkers42 reported less than a 10-degree loss of extension and a 10-degree loss of pronation and supination in 19 patients who underwent ORIF. A similar outcome was observed by Sanders and French107 in eight patients treated for difficult type III fractures. In a study of 56 patients, Ring and coworkers103 reported excellent results in patients with minimally comminuted fractures with three or fewer articular fragments. However results were unfavorable in patients with more comminuted fractures or if the fracture was associated with an elbow dislocation. Ikeda et al62 reported excellent and good results in nine out of 10 patients, using low-profile mini-plates for severely comminuted radial head fractures. Nine patients required hardware removal.
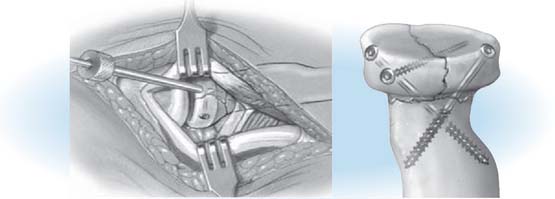
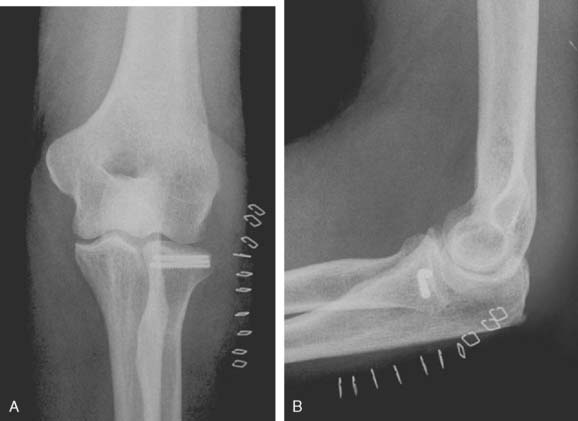
The Herbert screw has been reported to provide virtually normal function.14 The traditional AO technique using the 2.0 or 2.7 screws has been reported as satisfactory in 100% of patients with Mason type II fractures but in only 33% of those with Mason type III fractures.69 A small buttress plate can be used for radial neck fractures.73 Esser and colleagues38 reported on 26 cases of osteosynthesis, 11 with type II and nine with type III. All were graded as satisfactory after osteosynthesis (Fig. 24-19).
LOW-PROFILE FIXATION
We have recently compared the outcome of 10 patients with radial neck fracture managed by plate fixation to a comparable injury managed by a new “low-profile fixation” technique. In the latter instance, the fracture is fixed by inserting a threaded Kirschner wire (K-wire) or cannulated screw through the margin of the radial head across the fracture and engaging the opposite radial cortex (Fig. 24-20). A statistically significant better forearm arc of motion and elbow flexion arc was documented with the low-profile axial fixation technique.114 Some other technique modifications have been proposed recently. Fibrin adhesive seal was used as early as 1995, but despite excellent short-term results, this has never become a mainstream technique.4 Bioabsorbable polylactic pins have also been used since the early 1990s, for fixation of radial head fractures.51,59,92 In a recent prospective randomized study of 135 patients, results of fixation using polylactic pins have been shown to yield at least comparable results compared to other types of fixation.51 However, despite favorable results, biocompatibility may be an issue unique to this type of fixation.11,92
In comparison to resection or prosthetic replacement of the radial head, ORIF has been shown to be preferable if a stable fixation can be achieved. In a recent cadaveric study, ORIF has biomechanically been shown to be superior to resection or prosthetic radial head replacement.25
In a retrospective study by Parasa and Maffulli90 of 29 patients with radial head fractures managed with different surgical methods, ORIF showed the best re-sults in Mason type II fractures, followed by type III. Comparing different techniques, the best outcome was observed with screw fixation, followed by excision of the radial head, K-wire fixation, partial excision, Silastic implant, and plating. One prospective study by Khalfayan and associates68 compared the results of 16 patients treated by closed reduction and 20 by ORIF. The former had only 44% satisfactory results, compared with 90% in the group treated by ORIF. Boulas and coworkers12 compared results of ORIF with resection, Silastic radial head replacement, and conservative treatment in 36 patients. The best clinical scores were found in patients treated with ORIF, and the authors recommended this type of treatment for displaced radial head fractures.
DISPLACED FRACTURES
Evaluation of the number, size, and displacement of fracture fragments is extremely difficult from plain radiographs. The fracture and associated bony lesions are therefore routinely assessed using computed tomography (CT) scanning of the elbow (Fig. 24-21). If the displacement is more than 2 mm, ORIF is performed with headless screws or occasionally special plates (Fig. 24-22). The distal radioulnar joint injury is treated by ORIF of the radial head and may also require surgical stabilization by an open procedure or percutaneous cross-pinning to maintain radial length. Even with the aid of CT scanning, the severity of the fracture can sometimes be underestimated from imaging studies; therefore, it is our clinical practice to have screws and plates and also a prosthetic device available during surgery (Fig. 24-23).

FIGURE 24-21 The computed tomography scan accurately depicts subtle fractures and the precise amount of displacement.
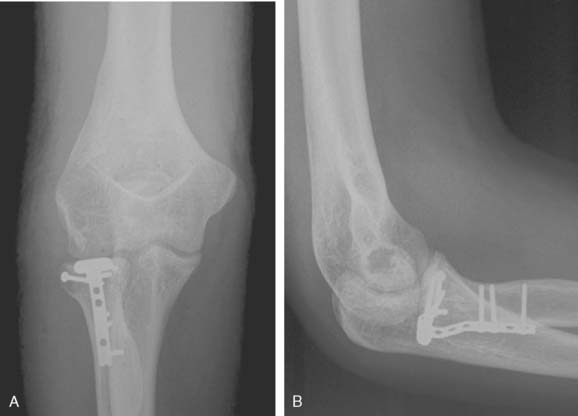
FIGURE 24-23 If the neck is involved, a mini plate may be used (A and B), but the senior author prefers low-profile fixation (see Fig. 24-20).
The surgical technique is described below.
Surgical Technique
An extended lateral incision is made over the lateral margin of the humerus, extending over the lateral epicondyle and the radial head. The incision is carried distally, parallel to the axis of the forearm. A posterior midline incision may also be used.35 This is especially helpful if associated medial-sided injuries need to be addressed surgically.
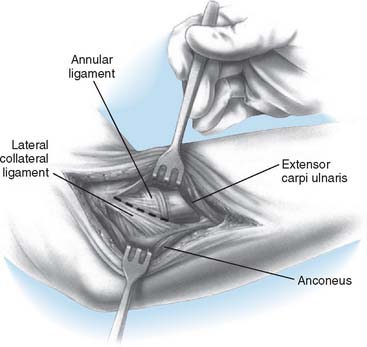
The Kocher approach between the anconeus and the extensor carpi ulnaris is the most frequently used exposure of the radiocapitellar joint. In traumatic situations, however, a musculocapsular rent is often present and should be incorporated in the approach, without further disruption of the soft tissue envelope. Care should be taken, not to disrupt the lateral ulnar collateral ligament (Fig. 24-24). Hematoma is evacuated and the forearm is rotated to expose the fragment. The forearm should be pronated, and the use of retractors behind the radial head and neck should be avoided in order to protect the posterior interosseus nerve.119 Reduction and provisional fixation can be achieved with a 0.45 K-wire. Depending on the anatomy of the fracture and size of the fragments, one or two 2.0, 2.7 AO, or Herbert screws,14,79,91 bioabsorbable pins,51,59,92 bladeplates,103 or plates and screws62 are inserted in as perpendicular a position to the joint and fracture surface as possible.39,48,61,111 If necessary, the head is counter-sunk and care is taken to ensure that the screw tip has not violated the opposite cortex (Fig. 24-25). The lateral soft tissues, including the annular ligament are repaired, and, if no associated injuries are present, immediate motion is begun. The aim of all types of ORIF is to obtain a stable fixation that allows for immediate mobilization of the elbow joint.
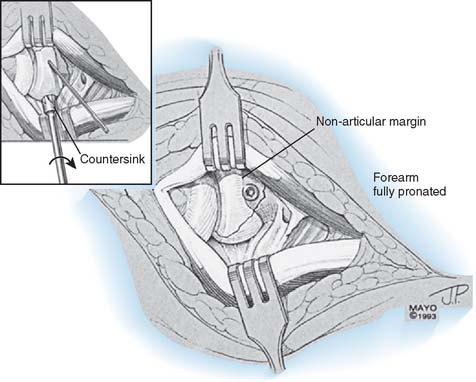
FIGURE 24-25 The head of the AO screw is countersunk to lessen the likelihood of impingement or soft tissue irritation.
In radial neck fractures, plates tend to produce excessive scar formation, necessitating removal in almost all instances.61,62 If possible, we therefore avoid plate fixation and prefer “axial, low-profile” fixation for neck fractures. Our review of 24 fractures revealed a mean forearm rotation of 113 and 160 degrees for the plate plus low-profile screw, respectively (P < .05).114 Thus, we prefer the “low-profile” screw fixation technique. The technique consists of the use of either threaded K-wires or 2.7-mm cannulated screws placed from the margin of the head, across the fracture to engage the opposite cortex (see Fig. 24-20). The development of low-profile plates such as shown in Figure 24-26 may lessen the tendency for scarring and improve forearm rotation after their use. We must await data to determine if this expectation will be realized.
TYPE III FRACTURES—AUTHORS’ PREFERENCE
In uncomplicated type III fractures, we prefer complete and early excision (within 24 hours of injury), followed by active motion in 3 to 5 days if ORIF is not possible. However, fractures are (1) almost always (>80%) associated with additional articular or ligamentous injuries,127 (2) are too comminuted for fixation, and hence, are treated most commonly by prosthetic replacement, especially if the fracture consists of more than four fragments. The growing interest and proliferation of implant designs have prompted a separate section to discuss this important topic more fully.
Long-term follow-up studies of 50 type IV fractures treated at the Mayo Clinic12,13 has provided our guidelines of treatment.
The overall treatment logic for managing radial head fractures seen acutely or in a delayed time frame is shown in Figures 24-27 and 24-28, respectively.
1 Adler J.B., Shaftan G.W. Radial head fractures, is excision necessary? J. Trauma. 1964;4:115.
2 Aegina P.. Fractures and Dislocation. Adams F.. New Sydenham Society, London, 1846.
3 Amis A.A., Miller J.H. The mechanisms of elbow fractures: an investigation using impact tests in vitro. Injury. 1995;26:163.
4 Arcalis Arce A., Marti Garin D., Molero Garin V., Pedemonte Jansama J. Treatment of radial head fractures using a fibrin adhesive seal. A review of 15 cases. J. Bone Joint Surg.. 1995;77B:422.
5 Arner O., Ekengren K., von Schreeb T. Fractures of the head and neck of the radius. A clinical and roentgenographic study of 310 cases. Acta. Chir. Scand. 1956;112:115.
6 Arvidsson H., Johansson O. Arthography of the elbow-joint. Acta. Radiol. 1955;43:445.
7 Bakalim G. Fractures of radial head and their treatment. Acta. Orthop. Scand. 1970;41:320.
8 Beingessner D.M., Dunning C.E., Beingessner C.J., Johnson J.A., King G.J. The effect of radial head fracture size on radiocapitellar joint stability. Clin. Biomech. (Bristol, Avon). 2003;18:677.
9 Beingessner D.M., Dunning C.E., Gordon K.D., Johnson J.A., King G.J. The effect of radial head fracture size on elbow kinematics and stability. J. Orthop. Res. 2005;23:210.
10 Bohrer J.V. Fractures of the head and neck of the radius. Ann. Surg. 1933;97:204.
11 Bostman O.M., Pihlajamaki H.K. Adverse tissue reactions to bioabsorbable fixation devices. Clin. Orthop. 2000;371:216.
12 Boulas H.J., Morrey B.F. Biomechanical evaluation of the elbow following radial head fracture. Comparison of open reduction and internal fixation vs. excision, silastic replacement, and non-operative management. Chir. Main. 1998;17:314.
13 Broberg M.A., Morrey B.F. Results of delayed excision of the radial head after fracture. J. Bone Joint Surg. 1986;68A:669.
14 Bunker T.D., Newman J.H. The Herbert differential pitch bone screw in displaced radial head fractures. Injury. 1985;16:621.
15 Burton A.E. Fractures of the head of the radius. Proc. R. Soc. Med. 1942;35:764.
16 Bush L.F., McLain E.J.Jr. Operative treatment of fractures of the elbow in adults. Instruct. Course Lect. 1959;16:265.
17 Buxton J.D. Ossification in the ligaments of the elbow joint. J. Bone Joint Surg. 1938;20:709.
18 Byrd J.W. Elbow arthroscopy for arthrofibrosis after type I radial head fractures. Arthroscopy. 1994;10:162.
19 Caputo A.E., Burton K.J., Cohen M.S., King G.J. Articular cartilage injuries of the capitellum interposed in radial head fractures: A report of ten cases. J. Shoulder Elbow Surg. 2006;15:716.
20 Caputo A.E., Mazzocca A.D., Santoro V.M. The nonarticulating portion of the radial head: anatomic and clinical correlations for internal fixation. J. Hand Surg. 1998;23A:1082.
21 Carr C.R., Howard J.W. Metallic cap replacement of radial head following fracture. W. J. Surg. Obstet. Gynecol. 1951;59:539.
22 Carstam N. Operative treatment of fractures of the head and the neck of the radius. Acta. Orthop. Scand. 1950;19:502.
23 Castberg T., Thing E. Treatment of fractures of the upper end of the radius. Acta. Chir. Scand. 1953;1051:62.
24 Celli A., Nicoli E. Fractures of the radial head associated with dislocation of the elbow. Chirurgia Organi Mov. 2004;89:7.
25 Charalambous C.P., Stanley J.K., Siddique I., Powell E., Ramamurthy C., Gagey O. Radial head fracture in the medial collateral ligament deficient elbow; biomechanical comparison of fixation, replacement and excision in human cadavers. Injury. 2006;37:849.
26 Cobb T.K., Beckenbaugh R.D. Nonunion of the radial neck following fracture of the radial head and neck: case reports and a review of the literature. Orthopedics. 1998;21:364.
27 Conn J., Wade P. Injuries of the elbow: a ten-year review. J. Trauma. 1961;1:248.
28 Curr J.F., Coe W.A. Dislocation of the distal radio-ulnar joint. Br. J. Surg. 1947;34:74.
29 Cutler C. Fractures of the head and neck of the radius. Ann. Surg. 1926;8:267.
30 Davidson P.A., Moseley J.B., Tullos H.S. Radial head fracture: A potentially complex injury. Clin. Orthop. Relat. Res. 1993;297:224.
31 Dawson F.A., Inostroza F. Arthroscopic reduction and percutaneous fixation of a radial neck fracture in a child. Arthroscopy. 2004;20(suppl 2):90.
32 Dehne E., Torp R.P. Treatment of joint injuries by immediate mobilization. Based upon the spinal adaptation concept. Clin. Orthop. Relat. Res. 1971;77:218.
33 Desault P.J.. Bichat X., Caldwell C., editors. Treatise on Fractures, Luxations and Affections of the Bones, 2nd ed., Philadelphia: Kimber & Conrad, 1811.
34 Dooley J.F., Angus P.D. The importance of elbow aspiration when treating radial head fractures. Arch. Emerg. Med. 1991;8:117.
35 Dowdy P.A., Bain G.I., King G.J., Patterson S.D. The midline posterior elbow incision. An anatomical appraisal. J. Bone Joint Surg. 1995;77B:696.
36 Edwards G.S.Jr., Jupiter J.B. Radial head fractures with acute distal radioulnar dislocation. Essex-Lopresti revisited. Clin. Orthop. Relat. Res. 1988;234:61.
37 Eliason E.L., North J.P. Fractures about the elbow. Am. J. Surg. 1939;44:88.
38 Esser R.D., Davis S., Taavao T. Fractures of the radial head treated by internal fixation: late results in 26 cases. J. Orthop. Trauma. 1995;9:318.
39 Firica A., Troianescu O. Fractures communitives de la tête radiale: Technique de reconstruction chirurgicale. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1979;65(suppl 2):66.
40 Fleetcroft J.P. Fractures of the radial head: early aspiration and mobilisation. J. Bone Joint Surg. 1984;66B:141.
41 Fleming C. Fractures of the head of the radius. Proc. R. Soc. Med. 1932;25:1011.
42 Geel C.W., Palmer A.K., Ruedi T., Leutenegger A.F. Internal fixation of proximal radial head fractures. J Orthop Trauma. 1990;4:270-274.
43 Gerard Y., Schernbourg F., Nerot C. Anatomical pathological and therapeutic investigation of fractures of the radial head in adults. J. Bone Joint Surg. 1984;66B:141.
44 Givon U., Pritsch M., Levy O., Yosepovich A., Amit Y., Horoszowski H. Monteggia and equivalent lesions. A study of 41 cases. Clin. Orthop. Relat. Res. 1997;337:208.
45 Hammond R. Fracture of the head and neck of the radius. N. Y. State J. Med. 1910;17:472.
46 Hargadon E.J., Porter M.L. The Essex-Lopresti injury: a variation. J. Hand Surg. 1988;13B:450.
47 Harrington I.J., Tountas A.A. Replacement of the radial head in the treatment of unstable elbow fractures. Injury. 1981;12:405.
48 Heim U., Trub H.J. Erfahrungen mit der primären Osteosynthese von Radius-Köpfchenfrakturen. Helv. Chir. Acta. 1978;45:63.
49 Hein B. Fractures of the head of the radius: An analysis of 52 cases with specific reference to disabilities. Indust. Med. 1937;6:529.
50 Helferich H. Fractures and Dislocations. Translated by Hutchinson. London: J. New Sydenham Society, 1899.
51 Helling H.J., Prokop A., Schmid H.U., Nagel M., Lilienthal J., Rehm K.E. Biodegradable implants versus standard metal fixation for displaced radial head fractures. A prospective, randomized, multicenter study. J. Shoulder Elbow Surg. 2006;15:479.
52 Herbertsson P., Josefsson P.O., Hasserius R., Karlsson C., Besjakov J., Karlsson M. Uncomplicated Mason type-II and III fractures of the radial head and neck in adults. A long-term follow-up study. J. Bone Joint Surg. 2004;86A:569.
52a Herbertsson P., Josefsson P.O., Hasserius R., Besjakov J., Nyqvist F., Karlsson M.K. Fractures of the radial head and neck treated with radial head excision. J. Bone Joint Surg. 2004;86A:1925.
53 Herbertsson P., Josefsson P.O., Hasserius R., Karlsson C., Besjakov J., Karlsson M.K. Displaced Mason type I fractures of the radial head and neck in adults: a fifteen- to thirty-three-year follow-up study. J. Shoulder Elbow Surg. 2005;14:73.
54 Hitzrot J. The treatment of simple fractures: A study of some end results. Ann. Surg. 1912;55:338.
55 Hoffa, A.: Lehrbuch der Fracturen und Luxationen für Ärtze und Studierende. Würzburg, Der Stahel’schen K. Hof- und Universitätsbuch- und Kunsthandlung., 1891, p. 354.
56 Holdsworth B.J., Clement D.A., Rothwell P.N. Fractures of the radial head—the benefit of aspiration: a prospective controlled trial. Injury. 1987;18:44.
57 Hotchkiss R.N. Displaced fractures of the radial head: internal fixation or excision? J. Am. Acad. Orthop. Surg.. 1997;5:1.
58 Hotchkiss R.N., Weiland A.J. Valgus stability of the elbow. J. Orthop. Res.. 1987;5:372.
59 Hou Z.H., Zhou J.H., Li P., Shi J.G., Shi Y.B., Xia J.J., Yao J. Treatment of displaced radial head fractures by internal fixation with absorbable pins. Chin. J. Traumatol.. 2006;9:355.
60 Ikeda M., Sugiyama K., Kang C., Takagaki T., Oka Y. Comminuted fractures of the radial head. Comparison of resection and internal fixation. J. Bone Joint Surg.. 2005;87A:76.
61 Ikeda M., Sugiyama K., Kang C., Takagaki T., Oka Y. Comminuted fractures of the radial head: comparison of resection and internal fixation. Surgical technique. J. Bone Joint Surg.. 2006;88A(suppl 1 Pt 1):11.
62 Ikeda M., Yamashina Y., Kamimoto M., Oka Y. Open reduction and internal fixation of comminuted fractures of the radial head using low-profile mini-plates. J. Bone Joint Surg.. 2003;85B:1040.
63 Itamura J., Roidis N., Mirzayan R., Vaishnav S., Learch T., Shean C. Radial head fractures: MRI evaluation of associated injuries. J. Shoulder Elbow Surg.. 2005;14:421.
64 Janssen R.P., Vegter J. Resection of the radial head after Mason type III fractures of the elbow: Follow-up at 16 to 30 years. J. Bone Joint Surg.. 1998;80B:231.
65 Johannsson O. Capsular and ligamentous injuries of the elbow joint. Acta. Chir. Scand. 287(Suppl), 1962.
66 Johnston G.W. A follow-up of one-hundred cases of fracture of the head of the radius with a review of the literature. Ulster. Med. J. 1962;31:51.
67 Keon-Cohen B.T. Fractures at the elbow. J. Bone Joint Surg. 1966;48A:1623.
68 Khalfayan E.E., Culp R.W., Alexander A.H. Mason type II radial head fractures: operative versus nonoperative treatment. J. Orthop. Trauma. 1992;6:283.
69 King G.J., Evans D.C., Kellam J.F. Open reduction and internal fixation of radial head fractures. J. Orthop. Trauma. 1991;5:21.
70 Kopp P. Zur Problematik der operativen Therapie von Radiuskopfchen und Olecranonfrakturen. Beitr. Orthop. Traumatol. 1975;22:483.
71 Lambotte A. Chirurgie Opératoire des Fractures. Bruxelles: Société Franco-Belge d’éditions scientifiques, 1924;494.
72 Lapner P.C., Leith J.M., Regan W.D. Arthroscopic debridement of the elbow for arthrofibrosis resulting from nondisplaced fracture of the radial head. Arthroscopy. 2005;21:1492.
73 Leung K.S., Tse P.Y.T. A new method of fixing radial neck fractures: Brief report. J. Bone Joint Surg. 1989;71B:326.
74 Liow R.Y., Cregan A., Nanda R., Montgomery R.J. Early mobilisation for minimally displaced radial head fractures is desirable. A prospective randomised study of two protocols. Injury. 2002;33:801.
75 Loomis L.K. Reduction and after-treatment of posterior dislocation of the elbow. Am. J. Surg. 1944;63:56.
76 Mason J.A., Shutkin N.M. Immediate active motion treatment of fractures of the head and neck of the radius. Surg. Gynecol. Obstet. 1943;76:731.
77 Mason M.L. Some observations on fractures of the head of the radius with a review of hundred cases. Br. J. Surg. 1954;42:123.
78 Mathur N., Sharma C.S. Fracture of the head of the radius treated by elbow cast. Acta. Orthop. Scand. 1984;55:567.
79 McArthur R.A. Herbert screw fixation of fracture of the head of the radius. Clin. Orthop. Relat. Res. 1987;224:79.
80 McGuigan F.X., Bookout C.B. Intra-articular fluid volume and restricted motion in the elbow. J. Shoulder Elbow Surg. 2003;12:462.
81 Morrey B.F. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. Instruct. Course Lect. 1995;44:175.
82 Morrey B.F. Fractures of the distal humerus: role of elbow replacement. Orthop. Clin. North Am. 2000;31:145.
83 Morrey B.F., An K.N. Articular and ligamentous contributions to the stability of the elbow joint. Am. J. Sports Med. 1983;11:315.
84 Morrey B.F., An K.N., Stormont T.J. Force transmission through the radial head. J. Bone Joint Surg. 1988;70A:250.
85 Morrey B.F., Tanaka S., An K.N. Valgus stability of the elbow. A definition of primary and secondary constraints. Clin. Orthop. Relat. Res. 1991;265:187.
86 Murray R.C. Fractures of the head and the neck of the radius. Br. J. Surg. 1940;28:106.
87 Neuwirth A.A. Nonsplinting treatment of fractures of the elbow joint. J. A. M. A. 1942;12:971.
88 Odelberg-Johnson G. On fractures of the proximal portion of the radius and their causes. Acta. Radiol. 1924;3:45.
89 O’Dwyer H., O’Sullivan P., Fitzgerald D., Lee M.J., McGrath F., Logan P.M. The fat pad sign following elbow trauma in adults: its usefulness and reliability in suspecting occult fracture. J. Comput. Assist. Tomogr. 2004;28:562.
90 Parasa R.B., Maffulli N. Surgical management of radial head fractures. J. R. Coll. Surg. Edinb. 2001;46:76.
91 Pearce M.S., Gallannaugh S.C. Mason type II radial head fractures fixed with Herbert bone screws. J. R. Soc. Med. 1996;89:340.
92 Pelto K., Hirvensalo E., Bostman O., Rokkanen P. Treatment of radial head fractures with absorbable polyglycolide pins: a study on the security of the fixation in 38 cases. J. Orthop. Trauma. 1994;8:94.
93 Petit J.L.. A Treatise of the Disease of the Bones; Containing an Extract and Complete Account of All Their Various Kinds, vol. 6. T. Woodward, London, 1720;288.
94 Pierce R.O.Jr., Hodurski D.F. Fractures of the humerus, radius and ulna in the same extremity. J. Trauma. 1979;19:182.
95 Pomianowski S., Sawicki G., Laskowski J. [Internal fixation in the treatment of radial head fractures]. Chir. Narzadow. Ruchu. Ortop. Pol. 2002;67:25.
96 Pribyl C.R., Kester M.A., Cook S.D., Edmunds J.O., Brunet M.E. The effect of the radial head and prosthetic radial head replacement on resisting valgus stress at the elbow. Orthopedics. 1986;9:723.
97 Quigley T.B. Aspiration of the elbow joint in the treatment of fractures of the head of the radius. N. Engl. J. Med. 1949;240:915.
98 Radin E.L., Riseborough E.J. Fractures of the radial head. A review of eighty-eight cases and analysis of the indications for excision of the radial head and non-operative treatment. J. Bone Joint Surg. 1966;48A:1055.
99 Ramon Soler R., Paz Tarela J., Soler Minores J.M. Internal fixation of fractures of the proximal end of the radius in adults. Injury. 1979;10:268.
100 Regan W., Morrey B. Fractures of the coronoid process of the ulna. J. Bone Joint Surg. 1989;71A:1348.
101 Reith P.L. Fractures of the radial head associated with chip fracture of the capitellum in adults: surgical considerations. South Surgeon. 1948;14:154.
102 Ring D., Psychoyios V.N., Chin K.R., Jupiter J.B. Nonunion of nonoperatively treated fractures of the radial head. Clin. Orthop. Relat. Res. 2002;398:235.
103 Ring D., Quintero J., Jupiter J.B. Open reduction and internal fixation of fractures of the radial head. J. Bone Joint Surg. 2002;84A:1811.
104 Rochwerger A., Bataille J.F., Kelberine F., Curvale G., Groulier P. Analyse rétrospective d’une série de 78 fractures de la tête radiale opérées. Acta. Orthop. Belg. 1996;62:87.
105 Rolla P.R., Surace M.F., Bini A., Pilato G. Arthroscopic treatment of fractures of the radial head. Arthroscopy. 2006;22:233 e1.
106 Sanchez-Sotelo J., Romanillos O., Garay E.G. Results of acute excision of the radial head in elbow radial head fracture-dislocations. J. Orthop. Trauma. 2000;14:354.
107 Sanders R.A., French H.G. Open reduction and internal fixation of comminuted radial head fractures. Am. J. Sports Med. 1986;14:130.
108 Scharplatz D., Allgower M. Fracture-dislocations of the elbow. Injury. 1975;7:143.
109 Schwab G.H., Bennett J.B., Woods G.W., Tullos H.S. Biomechanics of elbow instability: the role of the medial collateral ligament. Clin. Orthop. Relat. Res. 1980;146:42.
110 Schwartz R.P., Young F. Treatment of fractures of the head and neck of the radius and slipped radial epiphysis in children. Surg. Gynecol. Obstet. 1933;57:258.
111 Shmueli G., Herold H.Z. Compression screwing of displaced fractures of the head of the radius. J. Bone Joint Surg. 1981;63B:535.
112 Simpson N.S., Goodman L.A., Jupiter J.B. Contoured LCDC plating of the proximal ulna. Injury. 1996;27:411.
113 Smith G.R., Hotchkiss R.N. Radial head and neck fractures: anatomic guidelines for proper placement of internal fixation. J. Shoulder Elbow Surg. 1996;5:113.
114 Smith A., Morrey B.F., Steinmann S.P. Low profile fixation of radial head and neck fractures. Surgical technique and clinical experience. J. Orthop. Trauma. 2007;21:718.
115 Sojbjerg J.O., Ovesen J., Gundorf C.E. The stability of the elbow following excision of the radial head and transection of the annular ligament. An experimental study. Arch. Orthop. Trauma. Surg. 1987;106:248.
116 Speed K. Ferrule caps for the head of the radius. Surg. Gynaecol. Obstet. 1941;73:845.
117 Speed K. Traumatic lesions of the head of the radius. Relation to elbow joint dysfunction. Surg. Clin. North Am. 1924;4:651.
118 Spinner M., Kaplan E.B. The quadrate ligament of the elbow—its relationship to the stability of the proximal radio-ulnar joint. Acta. Orthop. Scand. 1970;41:632.
119 Strachan J.C., Ellis B.W. Vulnerability of the posterior interosseous nerve during radial head resection. J. Bone Joint Surg. 1971;53B:320.
120 Struijs P.A., Smit G., Steller E.P. Radial head fractures: effectiveness of conservative treatment versus surgical intervention: A systematic review. Arch. Orthop. Trauma. Surg. 2006;127:125.
121 Sudhahar T.A., Patel A.D. A rare case of partial posterior interosseous nerve injury associated with radial head fracture. Injury. 2004;35:543.
122 Thomas T.T. Fractures of the head of the radius. Univ. Pa. Med. Bull. 1905;18:221.
123 Thompson H.C.3rd, Garcia A. Myositis ossificans: aftermath of elbow injuries. Clin. Orthop. Relat. Res. 1967;50:129.
124 Trousdale R.T., Amadio P.C., Cooney W.P., Morrey B.F. Radio-ulnar dissociation. A review of twenty cases. J. Bone Joint Surg. 1992;74A:1486.
125 Van Glabbeek F., van Riet R., Jansen N., D’Anvers J., Nuyts R. Arthroscopically assisted reduction and internal fixation of tibial plateau fractures: report of twenty cases. Acta. Orthop. Belg. 2002;68:258.
126 Van Glabbeek F., van Riet R., Verstreken J. Current concepts in the treatment of radial head fractures in the adult. A clinical and biomechanical approach. Acta. Orthop. Belg. 2001;67:430.
127 van Riet R.P., Morrey B.F., O’Driscoll S.W., Van Glabbeek F. Associated injuries complicating radial head fractures: a demographic study. Clin. Orthop. Relat. Res. 2005;441:351.
128 van Riet R.P., Van Glabbeek F., Verborgt O., Gielen J. Capitellar erosion caused by a metal radial head prosthesis: Case report. J. Bone Joint Surg. 2004;86A:1061.
129 van Riet R.P., Morrey B.F.. Documentation of associated injuries occuring with radial head fractures. Clin. Orthop. Rel. Res, 2008;466:130.
130 Wagner C.J. Fractures of the head of the radius. Am. J. Surg. 1955;89:911.
131 Wallenbock F., Potsch F. Resection of the radial head: An alternative to use of a prosthesis. J. Trauma. 1997;43:959.
132 Ward W.G., Nunley J.A. Concomitant fractures of the capitellum and radial head. J. Orthop. Trauma. 1988;2:110.
133 Watson-Jones R. Discussion of minor injuries of the elbow joint. Proc. R. Soc. Med. 1930;23:323.
134 Watson-Jones R. Fractures and Other Bone and Joint Injuries, 2nd ed., Baltimore: Williams & Wilkins Co.; 1941:336.
135 Weseley M.S., Barenfeld P.A., Eisenstein A.L. Closed treatment of isolated radial head fractures. J. Trauma. 1983;23:36.
136 Wildin C.J., Bhowal B., Dias J.J. The incidence of simultaneous fractures of the scaphoid and radial head. J. Hand Surg. 2001;26B:25.
137 Wilson P.D. Fracture and dislocation in the region of the elbow. Surg. Gynecol. Obstet. 1933;56:335.
PART B Prosthetic Radial Head Replacement
INTRODUCTION
In general, indications for management of radial head fracture are well understood and accepted. As noted earlier, fixation is always preferable, but when this is not possible or not advisable, as in the presence of more than three fragments, then prosthetic replacement should be considered. Specifically, the implant should be used when the secondary stabilizing function of the radial head is required. This occurs when associated injuries have occurred (Table 24-1). Fracture of more than 25% to 50% of the coronoid with radial head fracture is an absolute indication for replacement if fixation of the head is not possible. Deficiency of the medial collateral ligament or disruption of the distal radioulnar joint are additional well-recognized indications for radial head prosthetic replacement.
Longitudinal instability of the radius (Essex-Lopresti injury) continues to be an extremely different problem, as noted earlier.16 Acute management may be adequate in up to 80%, but reconstruction is effective in only about 30% percent.4,13 The radial head implant is useful and may be even essential when reconstructing this difficult problem.
CONTRAINDICATIONS
The use of an implant is obviously contraindicated in the presence of sepsis. Malalignment that does not allow correction to allow articulation with the capitellum is a relative contraindication. If this problem cannot be addressed or solved with an articulated device, the implant must not be inserted. Articular trauma to the capitellum is a relative contraindication because some patients will do well, even with some degree of capitellar damage. If the resorption of the proximal radius is too extensive to be accommodated by the device, it obviously should not be inserted.
DESIGN CONSIDERATIONS
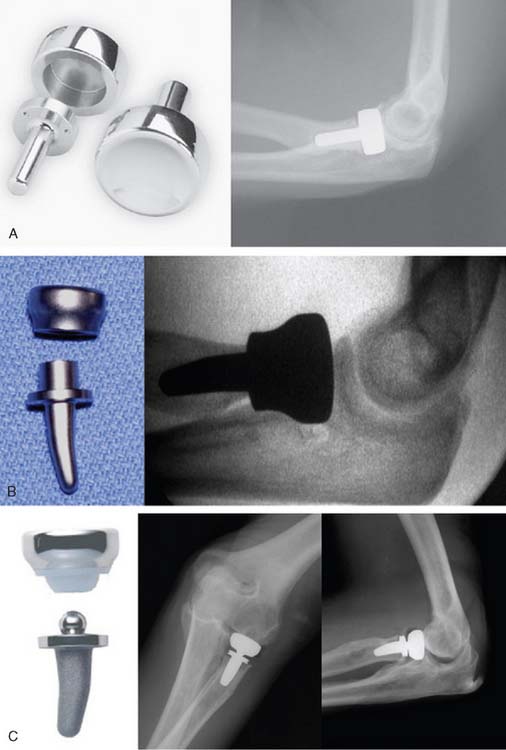
An increasing number of designs have recently appeared on the market (Fig. 24-29). There are three major considerations when selecting a prosthetic radial head implant: (1) sizing; (2) alignment, and (3) stem fixation.
STEM FIXATION
There are three basic fixation philosophies: (1) smooth, polished uncemented; (2) cemented stems, and (3) textured implants designed to either provide biologic fixation to be secured with cement. The round, smooth stem of the Evolve device (Wright Medical Technology, Inc., Arlington, TN) makes no attempt at achieving rigid fixation, but rather the stem is used only to align the articular disc with the capitellum. Motion of stems designed to be fixed are typically painful and, if loose, tend to cause osteolysis. However, the smooth polished stem is believed to avoid or lessen this problem. This system also allows for some axial motion between the stem and bone. There are favorable published results with this design philosophy to justify its value and consideration.3
ARTICULATION
What appears to be clearly emerging is that the single most important prognostic consideration is whether the implant is used to address the acute fracture or as a reconstruction device. When the radial head is being replaced as a secondary procedure to salvage a previously failed or untreated traumatic or pathologic event, alignment of the proximal radius is altered and difficult to restore. Therefore, the major requirement is that the prosthetic radial head align with and articulate with the capitellum. When pathology alters the radial/humeral relationship, the fixed articulation implants become vulnerable to subluxation, dislocation, or erosion of the capitellum. It is for this reason that designs that allow a degree of freedom at the stem/articular junction are attractive to address this circumstance. In the author’s opinion and practice, articulated implants may also be used in the acute fracture setting as well, because they provide reliable articulation in both settings. Experimental data suggest both fixed and articulated ligaments offer similar stability to valgus stress10 (Fig. 24-30). The theoretical disadvantage of the articulated radial head implant, of course, is the potential to generate wear debris. Although this has been a theoretical consideration, we are aware of no instances of this having occurred, in fact, to date; however, the clinical experience is quite limited. In summary, we believe the advantages outweigh the disadvantages.
TECHNIQUE
EXPOSURE
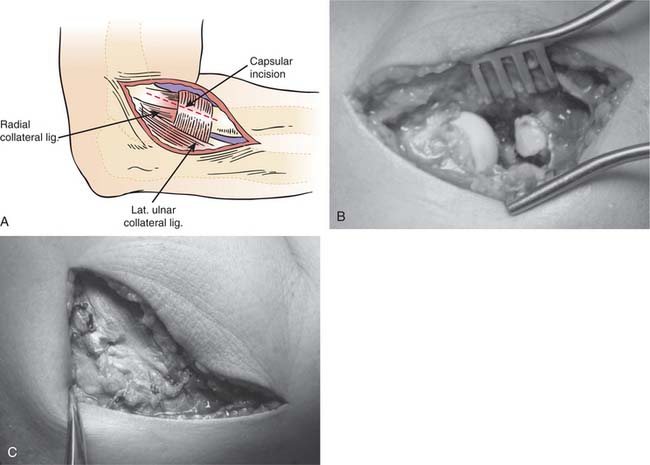
With the patient supine Kocher’s or Kaplan’s interval is employed (Fig. 24-31). The lateral capsule is entered anterior to the collateral ligament, and the annular ligament and capsule are reflected anteriorly and posteriorly to expose the radial head. A portion of the lateral collateral ligament and anterior capsule can be reflected from the lateral epicondyle and anterior humerus to facilitate exposure, if necessary, but the lateral ulnohumeral ligament is preserved. If greater exposure is required, the ligament is reflected from its humeral origin. If the ligament has been disrupted, then the exposure progresses through the site of disruption to expose the radiohumeral.
RESECTING THE RADIAL HEAD
Optimum articulation requires an accurate resection that assures precise implant placement. We employ a resection guide to replicate the anatomic axis of forearm rotation using the capitellum and ulnar styloid as landmarks (Fig. 24-32). During resection, forearm rotation should be assessed to ensure resection perpendicular to the axis of rotation. The distal extent of resection is the minimal amount that is consistent with the restoration of function as dictated by the fracture line or previous radial head resection but still compatible with implant insertion and length restoration options for the design being used.
INTRAMEDULLARY PREPARATION
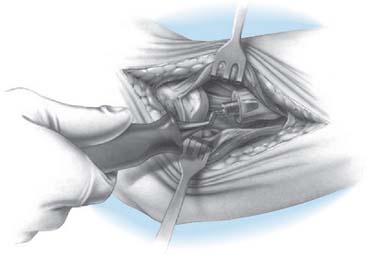
Varus stress and supination of the forearm allows exposure of the medullary canal, especially if the elbow is unstable. If the stability does not allow exposure of the proximal radius, careful reflection of the origin of the collateral ligament from the lateral epicondyle may be necessary. The canal is identified with a starter awl, with final canal preparation performed with curved rasps (Fig. 24-33).
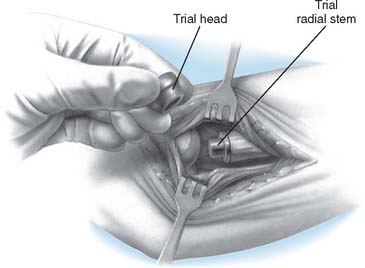
TRIAL REDUCTION
I use one size smaller stem than are to be used (Fig. 24-34). The appropriate-sized trial head is then applied (Fig. 24-35). Tracking in flexion and extension and in forearm rotation is carefully assessed.
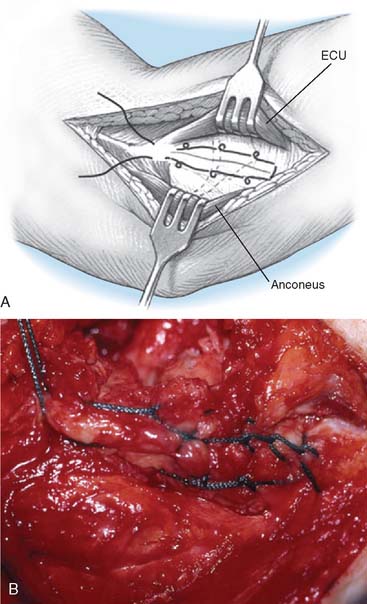
CLOSURE
Reconstitution of the lateral ulnar collateral ligament (LUCL) is essential at closure. If the ligamentous tissue appears inadequate, it should be reinforced with a No. 5 nonabsorbable Bunnell or Krackow suture (Fig. 24-36). For reconstruction applications, a formal LUCL substitute with tendon allograft (palmaris) or autograft (plantaris) may be necessary.
TECHNICAL NOTES
Overstuffing
A careful study performed by van Glabbeek et al14 in our laboratory documented the sensitivity of this articulation to precise longitudinal placement. Overstuffing of more than 2 mm caused measurable alteration of the kinematics of the elbow joint. A useful and simple means of assessing accurate restoration of radial length is to align the device with the lesser sigmoid notch of the ulna.
Malalignment
Capitellar erosion is believed to be due to malalignment or from overstuffing the joint. If the device has caused capitellar erosion, treatment is by removal of the device. In some instances, a capitellar device may solve this problem. Van Riet et al15 have also recently documented the fact that an osteoporotic capitellum may possibly predispose to capitellar erosion by a radial head implant.
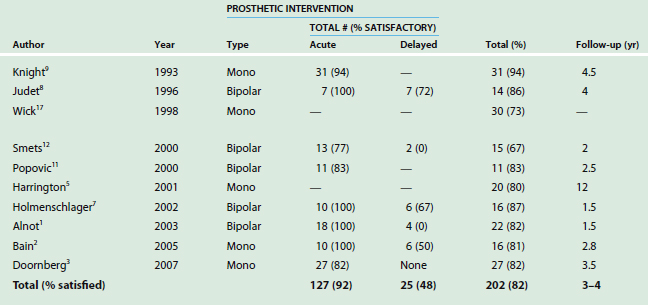
RESULTS
The most useful understanding of anticipated outcomes is realized from reviewing the literature over the past 15 years. However, because of considerable variation in the indications, acuteness of the injury, pathology being addressed, design employed, surveillance period, and tools of outcome assessment, meaningful comparisons or summaries of outcomes are difficult. Nonetheless, an attempt at a high level summary of the relevant literature is shown in Table 24-1. In general, one might anticipate a satisfactory outcome in about 85% of those treated immediately, and at best 50% to 60% of those treated in a delayed fashion (Fig. 24-37).
Regarding axial instability, we have assessed our experience with the use of a current generation radial head implant design and a capitellar replacement to stabilize the proximal migration of the radius. At 25, 63, and 175 months, all three are considered satisfactory.6 This appears to represent an important but far from final step forward in the management of this problem.
PROGNOSTIC FACTORS
Acute versus Chronic Condition
Without question, as identified in the previous edition of this book and confirmed by subsequent experience, this is the most significant determinant of outcome of radial head replacement. This observation has been confirmed in recent studies, such as that of Bain et al.2 These Australian investigators report 10 of 10 satisfactory outcomes a mean of 28 years after acute replacement for a Mason III fracture with dislocation. In contrast, three of six with delayed reconstruction did poorly. In a similar study from France, Alnot et al1 observed satisfactory function in all 18 acutely replaced radial heads but no acceptable outcomes in the four treated as a reconstructive procedure. In an unpublished review of Mayo early experience, we observed similar results.
Outcomes
Acute fractures were successfully managed in about 85%, but only about 50% were satisfactory after reconstructive procedures (see Table 24-1). Although not demonstrable as yet by objective assessment, our impression is that we are seeing improved results with the articulated prosthetic device, which avoids those failures associated with malalignment of the radiohumeral joint.
1 Alnot J.Y., Katz V., Hardy P. Guepar radial head prosthesis for recent and old fractures: A series of 22 cases. Rev Chir. Orthop. Reparatrice Appar. Mot. 2003;89:304.
2 Bain G.I., Ashwood N., Baird R., Unni R. Management of Mason type III radial head fractures with a titanium prosthesis, ligament repair, and early mobilization. Surgical technique. J. Bone Joint Surg. 2005;98A(Suppl 1 [Pt 1]):136.
3 Doornberg J.N., Parisien R., van Duijn J., Ring D. Radial head arthroplasty with a modular metal spacer to treat acute traumatic elbow instability. J. Bone Joint Surg. 2007;89:1075.
4 Edwards G.S.Jr, Jupiter J.B. Radial head fractures with acute distal radioulnar dislocation. Essex-Lopresti revisited. Clin. Orthop. Relat. Res. 1988;234:61.
5 Harrington I.J., Sekyi-Out A., Barrington T.W., Evans D.C., Tuli V. The functional outcome with metallic radial head implants in the treatment of unstable elbow fractures: A long-term review. J. Trauma. 2001;50:46.
6 Heijink A., Morrey B.F., Cooney W.P. Capitellar resurfacing arthroplasty: A case report of three patients. J. Shoulder Elbow Surg. 2007;17:e12.
7 Holmenschlager F., Halm J.P., Winckler S. Les fractures fraîches de la tête radiale. Résultants de la prothèse à cupule flottant de Judet. Rev. Chir. Orthop. Reparatrice Appar. Mot. 2002;88:387.
8 Judet T., Garreau de Loubresse C., Piriou P., Charnley G. A floating prosthesis for radial head fractures. J. Bone Joint Surg. 1996;78B:244.
9 Knight D.J., Rymaszewski L.A., Amis A.A., Miller J.H. Primary replacement of the fractured radial head with a metal prosthesis. J. Bone Joint Surg. 1993;75-B:572.
10 Pomianowski S., Sawicki G., Laskowski J. [Internal fixation in the treatment of radial head fractures]. Chir. Narzadow. Ruchu. Ortop. Pol. 2002;67:25.
11 Popovic N., Gillet P., Rodriguez A., Lemaire R. Fracture of the radial head with associated elbow dislocation: Results of treatment using a floating radial head prosthesis. J. Orthop. Trauma. 2000;14:171.
12 Smets S., Govaers K., Jansen N., van Riet R., Schaap M., Van Glabbeek F. The floating radial head prosthesis for comminuted radial head fractures: A multicentric study. Acta. Orthop. Belg. 2000;66:353.
13 Trousdale R.T., Amadio P.C., Cooney W.P., Morrey B.F. Radio-ulnar dissociation. A review of twenty cases. J. Bone Joint Surg. Am. 1992;74:1486.
14 Van Glabbeek F., van Riet R., Jansen N., D’Anvers J., Nuyts R. Arthroscopically assisted reduction and internal fixation of tibial plateau fractures: report of twenty cases. Acta. Orthop. Belg. 2002;68:258.
15 van Riet R.P., Van Glabbeek F., Verborgt O., Gielen J. Capitellar erosion caused by a metal radial head prosthesis: Case report. J. Bone Joint Surg. 2004;86A:1061.
16 van Riet R.P., Morrey B.F., O’Driscoll S.W., Van Glabbeek F. Associated injuries complicating radial head fractures: a demographic study. Clin. Orthop. Relat. Res. 2005;441:351.
17 Wick M., Lies A., Muller E.J., Hahn M.P., Muhr G. Prostheses of the head of the radius. What outcome can be expected? Unfallchirurg. 1998;101:817.