Chapter 68 Proprioception and Anterior Cruciate Ligament Reconstruction
The human ACL has been shown to contain mechanoreceptors including Golgi tendon organs, Pacinian corpuscles, and Ruffini nerve endings.1,2 These receptors contribute to proprioception about the knee joint and are also believed to form part of a reflex arc in which an anterior displacement of the tibia results in hamstring muscle contraction. Such a reflex presumably serves to protect the knee, and the ACL in particular, from such stresses. ACL rupture can therefore be expected to result in disruption or alterations of these pathways.
Using a threshold to detection of passive movement test, Barrack et al3 demonstrated a significantly higher threshold value in ACL deficient limbs compared with the normal contralateral limb in a group of 11 patients tested 3 months following ACL rupture. A group of control subjects showed virtually identical threshold values for both knees. The higher threshold values were attributed to a loss of proprioceptive function. Numerous authors have also described the presence of deficits attributable to loss of proprioception in ACL deficient knees, whereas some authors have shown no differences between injured and contralateral or healthy control subject knees (for review, see Reider et al4). For instance, Pap et al5 found a higher rate of failure to detect passive movement in ACL deficient knees compared with the contralateral knee or healthy control subjects’ knees. However, unlike Barrack et al, they did not find any difference in the threshold to detect passive movement among any of the knees.
Beard et al6 measured the latency of reflex hamstring contraction in response to an anteriorly directed shear force to the upper calf in 30 patients with an ACL rupture. They found significantly greater latencies in the ACL deficient knees compared with the contralateral knees. Interestingly, the frequency of giving-way episodes reported by the patients correlated with the latency differential between their two limbs.
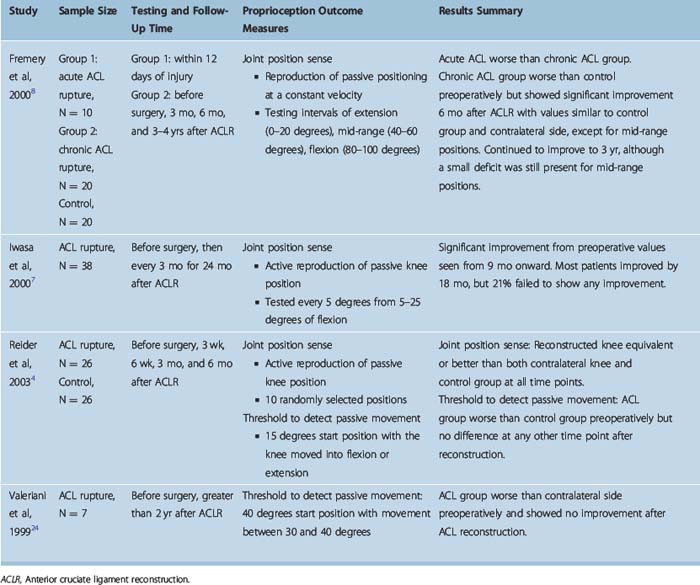
Many authors have evaluated proprioception following ACL reconstruction, but they have reported conflicting results. This may be due in part to the different methodologies employed. Various tests of proprioception have been used (joint position sense, threshold to detect passive movement, reaction time, and stabilometric testing). ACL reconstructed knees have been compared with either the contralateral knee, healthy control subject knees, or in some instances to both. Most studies have evaluated patients at only one time point, although some have followed patients over time from preoperatively to as long as 3.5 years postoperatively. The results of studies that have either used a control group of subjects or provided longitudinal follow-up have been summarized in Tables 68-1 and 68-2.
Table 68-1 Studies Comparing Proprioception Between Patients after Anterior Cruciate Ligament Reconstruction (ACLR) and Controls
| Study | Sample Details | Proprioception Outcome Measure |
|---|---|---|
| ACLR Group Equivalent to Control Group | ||
| Al-Othman, 200415 | 22 ACLR, all male, all PT graft, 1–6 yr post surgery (mean 3.6 yr), 30 controls | Joint position sense (standing position) |
| Ochi et al, 199916 | 23 ACLR, 13M:10F, 22 HS graft, 1 fascia lata graft, minimum 18 mo postsurgery, 14 controls (9M:5F) | Joint position sense |
| Roberts et al, 200017 | 20 ACLR, 15M:5F, all PT grafts, mean 24 mo postsurgery, 19 controls (14M:5F) | Joint position sense |
| Co et al, 199318 | 10 ACLR, 5M:5F; 8 PT grafts, 2 HS grafts, mean 31.6 mo postsurgery, 10 controls (5M:5F) | Joint position sense Threshold to detect passive movement |
| Risberg et al, 199919 | 20 ACLR, 8M:12F, all PT grafts, 11–32 mo postsurgery (mean 24 mo), 10 controls (5M:5F) | Threshold to detect passive movement |
| ACLR Group Worse than Control Group | ||
|---|---|---|
| Barrett et al, 199120 | 45 ACLR, 33M:12F, all PT grafts, 1–7 yr postsurgery (mean 3.2 yr), 20 age-matched controls | Joint position sense |
| Bonfim et al, 200321 | 10 ACLR, 7M:3F, 12–30 mo postsurgery (mean 18 mo), 10 controls (7M:3F), height and weight matched | Joint position sense Hamstring muscle latency Performance at maintaining upright stance Threshold to detect passive movement |
| Roberts et al, 200017 | 20 ACLR, 15M:5F, all PT grafts, mean 24 mo postsurgery, 19 controls (14M:5F) | Threshold to detect passive movement |
| Kaneko et al, 200222 | 17 ACLR, 8M:9F, all HS/Leeds-Keio grafts, 2–3 mo post surgery, 18 controls, 20 athletes (training control group) | Maximum voluntary isometric contraction |
| Shiraishi et al, 199623 | 53 ACLR, 22M:31F, all facia lata grafts, minimum 2 yr post surgery, 30 controls (15M:15F) | Stabilometric assessment |
F, Female; HS, hamstring; M, male; PT, patellar tendon.
From Table 68-1 it can be seen that the ACL reconstructed knees have been shown to be either equivalent to or worse than healthy control subject knees. The length of follow-up does not appear to explain the disparate findings. Four of the five studies that found no difference used joint position sense as a measure of proprioception, whereas only two of the five studies that found the ACL reconstructed knees to be inferior used this method of testing proprioception.
Two of the longitudinal studies used joint position sense as a measure of proprioception, whereas one used threshold to detect passive movement and another used both joint position sense and threshold to detect passive movement. Iwasa et al7 evaluated joint position sense in 38 subjects before ACL reconstruction using a hamstring tendon graft and every 3 months after surgery to 24 months. There was an improvement in joint position sense from 9 months through 18 months, but there was a small group of eight in whom joint position sense did not improve. A correlation was observed between better stability and better joint position sense.
Fremerey et al8 measured joint position sense in 20 patients with chronic ACL deficiency who underwent a patellar tendon ACL reconstruction as well as in 20 control subjects and 20 patients with an acute ACL rupture. Preoperatively the chronic ACL deficient knees had significantly better joint position sense than acute ACL deficient knees but were worse than control subjects’ knees. Following surgery there was an improvement, most of which occurred between 3 and 6 months. There was some further improvement at 3 years, although a small deficit remained in the operated knee for mid-range positions.
Reider et al4 undertook a longitudinal study of 26 patients undergoing ACL reconstruction and measured both joint position sense and threshold to detect passive movement preoperatively at 3 and 6 weeks and at 3 and 6 months postoperatively. They used both the contralateral knees as well as the knees of healthy volunteers as controls. The authors concluded that threshold to detect passive movement was a more reliable method than joint position sense for testing proprioception. In the patient group there was no significant difference in the threshold between the injured and contralateral knee at any of the time points. Both knees were significantly worse than the healthy controls preoperatively. However, both knees improved postoperatively such that they were not significantly different than healthy control knees at 6 months postoperatively.
The authors noted that improvements in proprioception were seen as early as 6 weeks following ACL reconstruction. Such a short time period is not consistent with reinnervation of the graft being the basis of the improvement. The authors, as well as Iwasa et al,7 suggest that the improvement is probably due to the provision of a static restraint that reduces abnormal afferent activity from the capsule and other ligaments.
A number of authors have investigated the role of rehabilitation protocols designed to improve proprioception and neuromuscular function in patents with ACL ruptures (for review, see Cooper at al9). Such protocols have been associated with some limited improvements in joint position sense and hop testing as well as muscle strength and subjective rating when compared with traditional strengthening programs. In a group of 50 patients with ACL deficiency, Beard et al10 compared a muscle-strengthening rehabilitation protocol with a program designed to enhance proprioception and reduce the latency of reflex hamstring contraction. The proprioceptive program was associated with greater improvements in reflex hamstring contraction latency and functional scores compared with the strengthening program.
Perhaps as a result of the use of such proprioceptive programs in patients with ACL rupture, proprioception-related exercises are now frequently included in rehabilitation programs following ACL reconstruction (for an example, see Risberg et al11). However, there is very little literature on the effects of the inclusion of such exercises.
Liu-Ambrose et al12 studied 10 patients at a minimum of 6 months following ACL reconstruction with a semitendinosus tendon graft. They were randomly allocated to an isotonic strength-training program or a proprioceptive training program. Both programs involved three sessions per week for a period of 12 weeks. The proprioceptive training program was based on previously described exercises. Progression was achieved by decreasing the base of support, decreasing the stability of the surfaces on which the exercises were performed, increasing the number of repetitions, reducing visual feedback, and increasing the speed and complexity of the tasks. Progression of the strength-training program was achieved by increased loading.
In a larger study of 29 patients, Cooper et al13 compared two different rehabilitation protocols following primary ACL reconstruction. Thirteen subjects in each group had undergone a four-strand hamstring tendon reconstruction, with the remainder having had a patellar tendon reconstruction. The patients were randomized to one of two 6-week physiotherapy programs, commencing between 4 and 14 weeks postoperatively, once they had achieved the following criteria: ability to walk without aids, 0 to 120 degrees of range of motion in the operated knee, straight leg raising without any extensor lag, and no or minimal joint effusion.
Not only do the effects of such training need to be more clearly established, but also the question of whether proprioception per se can be trained at all still needs to be answered. As Aston-Miller et al14 have noted, scenarios in which proprioception might be improved remain largely theoretical. If proprioception can indeed be improved by training, there remains the issue of what such improvement might achieve. The time required to develop protective muscle contraction in response to a stimulus is such that successful proprioceptive training might only be able to prevent injury as a result of relatively slow provocations, rather than the more rapidly applied forces that occur in a sporting situation. Thus the aim of proprioceptive training following ACL reconstruction needs to be clarified. Is it to restore normal function, to improve function beyond the individual’s preinjury level, or to prevent reinjury? If it is the latter, perhaps it is the improved patterns of muscular contraction as well as the awareness of and attention to various cues that are the real benefits of such training. Clearly, further studies are required to establish the role of proprioceptive training following ACL reconstruction.
1 Schultz RA, Miller DC, Kerr CS, et al. Mechanoreceptors in human cruciate ligaments. A histological study. J Bone Joint Surg. 1984;66A:1072-1076.
2 Schutte MJ, Dabezies EJ, Zimny ML, et al. Neural anatomy of the human anterior cruciate ligament. J Bone Joint Surg. 1987;69A:243-247.
3 Barrack RL, Skinner HB, Buckley SL. Proprioception in the anterior cruciate deficient knee. Am J Sports Med. 1989;17:1-6.
4 Reider B, Arcand MA, Diehl LH, et al. Proprioception of the knee before and after anterior cruciate ligament reconstruction. Arthroscopy. 2003;19:2-12.
5 Pap G, Machner A, Nebelung W, et al. Detailed analysis of proprioception in normal and ACL-deficient knees. J Bone Joint Surg. 1999;81B:764-768.
6 Beard DJ, Kyberd PJ, Fergusson CM, et al. Proprioception after rupture of the anterior cruciate ligament. An objective indication of the need for surgery? J Bone Joint Surg. 1993;75B:311-315.
7 Iwasa J, Ochi M, Adachi N, et al. Proprioceptive improvement in knees with anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2000;Dec:168-176.
8 Fremerey RW, Lobenhoffer P, Zeichen J, et al. Proprioception after rehabilitation and reconstruction in knees with deficiency of the anterior cruciate ligament: a prospective, longitudinal study. J Bone Joint Surg. 2000;82B:801-806.
9 Cooper RL, Taylor NF, Feller JA. A systematic review of the effect of proprioceptive and balance exercises on people with an injured or reconstructed anterior cruciate ligament. Res Sports Med. 2005;13:163-178.
10 Beard DJ, Dodd CA, Trundle HR, et al. Proprioception enhancement for anterior cruciate ligament deficiency. A prospective randomised trial of two physiotherapy regimens. J Bone Joint Surg. 1994;76B:654-659.
11 Risberg MA, Mork M, Jenssen HK, et al. Design and implementation of a neuromuscular training program following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2001;31:620-631.
12 Liu-Ambrose T, Taunton JE, MacIntyre D, et al. The effects of proprioceptive or strength training on the neuromuscular function of the ACL reconstructed knee: a randomized clinical trial. Scand J Med Sci Sports. 2003;13:115-123.
13 Cooper RL, Taylor NF, Feller JA. A randomised controlled trial of proprioceptive and balance training after surgical reconstruction of the anterior cruciate ligament. Res Sports Med. 2005;13:217-230.
14 Ashton-Miller JA, Wojtys EM, Huston LJ, et al. Can proprioception really be improved by exercises? Knee Surg Sports Traumatol Arthrosc. 2001;9:128-136.
15 Al-Othman AA. Clinical measurement of proprioceptive function after anterior cruciate ligament reconstruction. Saudi Med J. 2004;25:195-197.
16 Ochi M, Iwasa J, Uchio Y, et al. The regeneration of sensory neurones in the reconstruction of the anterior cruciate ligament. J Bone Joint Surg. 1999;81B:902-906.
17 Roberts D, Friden T, Stomberg A, et al. Bilateral proprioceptive defects in patients with a unilateral anterior cruciate ligament reconstruction: a comparison between patients and healthy individuals. J Orthop Res. 2000;18:565-571.
18 Co FH, Skinner HB, Cannon WD. Effect of reconstruction of the anterior cruciate ligament on proprioception of the knee and the heel strike transient. J Orthop Res. 1993;11:696-704.
19 Risberg MA, Beynnon BD, Peura GD, et al. Proprioception after anterior cruciate ligament reconstruction with and without bracing. Knee Surg Sports Traumatol Arthrosc. 1999;7:303-309.
20 Barrett DS. Proprioception and function after anterior cruciate reconstruction. J Bone Joint Surg. 1991;73:833-837.
21 Bonfim TR, Jansen Paccola CA, Barela JA. Proprioceptive and behavior impairments in individuals with anterior cruciate ligament reconstructed knees. Arch Phys Med Rehabil. 2003;84:1217-1223.
22 Kaneko F, Onari K, Kawaguchi K, et al. Electromechanical delay after ACL reconstruction: an innovative method for investigating central and peripheral contributions. J Orthop Sports Phys Ther. 2002;32:158-165.
23 Shiraishi M, Mizuta H, Kubota K, et al. Stabilometric assessment in the anterior cruciate ligament-reconstructed knee. Clin J Sport Med. 1996;6:32-39.
24 Valeriani M, Restuccia D, Di Lazzaro V, et al. Clinical and neurophysiological abnormalities before and after reconstruction of the anterior cruciate ligament of the knee. Acta Neurol Scand. 1999;99:303-307.