11 Proprietary Peels
Overview of Treatment Strategy
• Modified trichloroacetic acid peels
In an attempt to obtain more consistent results while giving the physician more control over the peel, variations of the TCA peel (Monheit’s Jessner-TCA peel, Coleman’s glycolic acid-TCA peel, Obagi’s blue peel) have been developed (Table 11.1). Anatomically, they are designed to peel through the papillary dermis and into the most superficial aspect of the reticular dermis (Obagi’s blue peel). Their main indications are for epidermal and upper dermal pathology: photodamage, actinic keratoses, lentigines, ephelides, fine rhytides, and very superficial, non-fibrotic scars. Deeper cutaneous abnormalities such as expression lines, deep furrows, or deep scars are not amenable to correction with these peels.
| Modified TCA peels | Peel components | Speed of TCA peel |
|---|---|---|
| Jessner’s solution + TCA | Jessner’s solutiona Followed by the application of a light coat of 35% TCA |
Stratum corneum is disrupted. Faster TCA penetration |
| Glycolic acid + TCA | 70% glycolic acid Followed by the application of a light coat of 35% TCA |
Stratum Corneum is disrupted. Faster TCA penetration |
| Obagi’s blue peel | Obagi’s blue peel baseb 2 mL Mixed with a specific volume of 30% TCA to achieve 15%, 20% or 25% TCA-blue peel |
Stratum corneum is left intact and a lower concentration of TCA is used. TCA peel speed is slowed down |
a Jessner’s solution: 14% resorcinol, 14% salicylic acid and 14% lactic acid mixed in ethanol
b Obagi’s blue peel base: non-ionic blue dye, glycerin, saponin
• Modified phenol peels
Both Stone and Hetter evaluated the role of the different components in the various phenol solutions and they both came to the conclusion that the croton oil concentration was the most important factor in predicting the depth of skin injury (Table 11.2). Croton oil is a very strong desiccant with cytotoxic properties even in minute concentrations. Croton oil is not water-soluble but is soluble in alcohol, benzene, ethyl acetate, and chloroform. Thus it is believed that phenol, which has a benzene ring in its structure, acts as a carrier for the croton oil.
Table 11.2 Summary of various phenol-croton oil peel solutions
| Modified phenol peels | Phenol (%) | Croton oil (%) |
|---|---|---|
| Baker-Gordon | 50 | 2.1 |
| Fintsi | 64 | 0.6–0.7 |
| Stone-2 | 60 | 0.2 |
| Stone V-K | 62 | 0.16 |
| Hetter | 50 | 0.7 |
| Hetter ‘all around’ | 35 | 0.4 |
| Hetter neck/eyelid | 30 | 0.1 |
Modified from: Rullan et al. 2004 The 2-Day Light Phenol Chemabrasion for Deep Wrinkles and Acne Scars: A Presentation of Face and Neck Peels. American Journal of Cosmetic Surgery 21:15–26
Treatment Techniques
• Modified TCA peels and modified phenol peels
Continued application of acid will result in vasospasm of the capillary loops in the papillary dermis. Blood flow to the area will cease, and the pink sign will disappear. The frost will appear as a solid white sheet (absence of the ‘pink sign’; Fig. 11.1). This is the endpoint for a superficial reticular dermis peel. The loss of the ‘pink sign’ implies that the entire papillary dermis is involved and the upper reticular dermis has been reached but not penetrated. In darker-skinned individuals, the ‘pink sign’ may be difficult to visualized, thereby ‘epidermal sliding’ must be used instead to gauge depth.
‘Epidermal sliding’ refers to the exaggerated wrinkling of the skin when it is pushed or pinched, occurring when papillary dermal edema formation disrupts the anchoring fibrils and allows the epidermis to move freely (Fig. 11.2). The ‘epidermal sliding’ sign indicates the peel has progressed through the epidermis and has entered the papillary dermis. As the papillary dermal proteins become coagulated and adhere to the epidermal coagulated proteins, the ‘epidermal sliding’ will disappear. Therefore, one must pay attention as this sign can be easily missed. As epidermal sliding disappears, so does the ‘pink sign’. In thick skin, ‘epidermal sliding’ may not be very obvious and the ‘pink sign’ must be used alone to determine depth. This sign is usually missed during phenol peels due to the quick nature by which they penetrate through the epidermis and into the dermis.
• Modified TCA Peels
• Modified phenol peels
It is important to keep ‘swirling’ the phenol solution prior to applying it since the croton oil will separate out from solution (Fig. 11.3). Once the entire cosmetic unit has been treated, deeper rhytids or scars can be retreated if needed to achieve a slightly deeper peel in this area. This can be done using the pointed end of a cotton tipped applicator stick that has been ‘snapped’ in half (Fig. 11.4).
Case Studies
• Case study 1
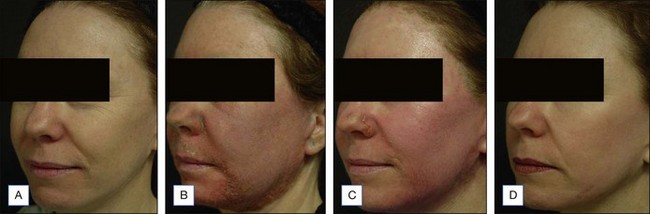
This case illustrates a healthy female patient in her late forties. She has light Caucasian skin with mild dyschromia, fine rhytides with heavier rhytides in the periorbital, glabellar, and perioral region (Fig. 11.5A). She underwent a full face 25% Obagi’s blue peel and a Hetter VL peel of the periorbital region, glabella, and focal perioral rhytides (Fig. 11.5B). At postoperative day 4 the patient shows edema and erythema. The areas treated with the phenol solution show crusting and more pronounced erythema. At one week (Fig. 11.5C) she is fully reepithelialized from the blue peel and is still healing from the Hetter VL peel. She is shown 3 months postoperatively (Fig. 11.5D) with nice firming of the skin, rhytid reduction, and a nice blending of the areas treated with the two different solutions.
• Case study 2
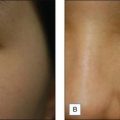
A 70-year-old female with solar lentigines, seborrheic keratosis, and rhytides is shown at baseline and at 2 months after a full face 25% Obagi’s blue peel (Fig. 11.6). The seborrheic keratosis were treated with light electrodessication prior to the start of the peel. She shows a dramatic improvement in solar lentigines and her seborrheic keratoses. Additionally she has nice tightening and rhytid reduction.
• Case study 3
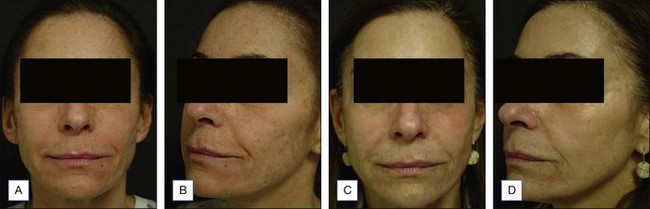
This case illustrates a healthy female patient in her mid fifties. She has medium Caucasian skin with moderate dyschromia, rhytides with heavier rhytides in the periorbital region (Fig. 11.7A, C). She underwent a full face 25% Obagi’s blue peel and a Hetter VL peel of the periorbital region. She is shown 5 months postoperatively (Fig. 11.7 B, D) with nice firming of the skin, rhytid reduction, and a nice blending of the areas treated with the two different solutions.
Coleman WP, Futrell JM. The glycolic acid and trichloroacetic acid peel. Journal of Dermatologic Surgery and Oncology. 1994;20:76-80.
Hetter G. Examination of the phenol-croton oil peel: part IV. Face peel results with different concentrations of phenol and croton oil. Plastic and Reconstructive Surgery. 2001;105:1061-1083.
Larson DL, Karmo F, Hetter GP. Phenol-croton oil peel: establishing an animal model for scientific investigation. Aesthetic Surgery Journal. 2009;29:47-53. Comment in: Aesthetic Surgery Journal 2009;29:446; author reply 446
Monheit GD. The Jessner’s-trichloroacetic acid peel. An enhanced medium-depth chemical peel. Dermatology Clinics. 1995;13:277-283.
Obagi Z, Obagi S, Alaiti S, Stevens M. TCA-based blue peel: a standardized procedure with depth control. Dermatologic Surgery. 1999;25:773-780.
Stone PA. the use of modified phenol for chemical face peeling. Clinics in Plastic Surgery. 1998;25:21-44.
Stone PA, Lefer LG. Modified phenol chemical face peels: recognizing the role of application technique. Clinics in Plastic Surgery. 2001;28:13-36. Erratum in: Clinics in Plastic Surgery 2001 Jul;28(3):preceding xi