Other procedures
A Burns
Burn injuries, regardless of their origin, are classified according to the depth and the extent of the skin and tissue destruction as well as the total body surface area (TBSA) involved. The degrees of burn injury with classification, tissue involvement, and appearance are shown in the following table.
| Classification | Tissue Level Involvement | Appearance |
| Superficial, first-degree burn | Epidermis destroyed | Skin, red tone (sunburn); painful with erythema and blisters; heals spontaneously with no scarring |
| Partial-thickness, second-degree burn | ||
| Superficial dermal | Epidermis and some (upper) dermis destroyed | Red or pale ivory with a moist, shiny surface; painful, immediate blisters with minimal scarring |
| Deep dermal | Epidermis and deep dermis | Mottled with white, waxy, dry surface; blisters may or may not appear; significant scarring |
| Full-thickness, third-degree burn | All epidermis and dermis | White, cherry red, or black; dry, tissue-paper skin; grafting necessary; decreased scarring with early excision |
| Fourth-degree burn | Muscle, fascia, bone | Complete excision required; limited function |
Modified from Faldmo L, Kravitz M. Management of acute burns and burn shock resuscitation. AACN Clin Issues Crit Care Nurs 1993;4:351-366.
A major burn is defined as a second-degree burn involving more than 10% of the TBSA in adults or 20% at extremes of age, a third-degree burn involving more than 10% of the TBSA in adults, and any electrical burn or one complicated by smoke inhalation. A burn formula derived from the National Burn Registry estimating mortality is as follows: If the age of the patient plus the percentage of the TBSA burned exceeds 115, the mortality rate is greater than 80%. Additionally, from clinical observations, it is estimated that the mortality rate of a burn victim is approximately doubled if there is an inhalation injury sustained in conjunction with a thermal burn.
Patients who sustain full-thickness burns are seen in the operating room, often repeatedly, for débridement and grafting. The initial assessment of an emergency patient with a burn injury is initiated as for any trauma patient and begins with airway intubation. Keep in mind that airway edema occurs rapidly in a burn patient, and intubation after the edema occurs is difficult. Burn patients must have aggressive fluid resuscitation in the first 48 hours. Burns are described according to the rule of nines, which divides the body into areas of 9% or multiples thereof. For example, the head and neck combined, each arm, each leg, the posterior surface of the upper trunk, and the posterior surface of the lower trunk are each considered to be 9% of the surface area of the body. Survival is influenced by the percentage of the surface area involved and the age of the patient.
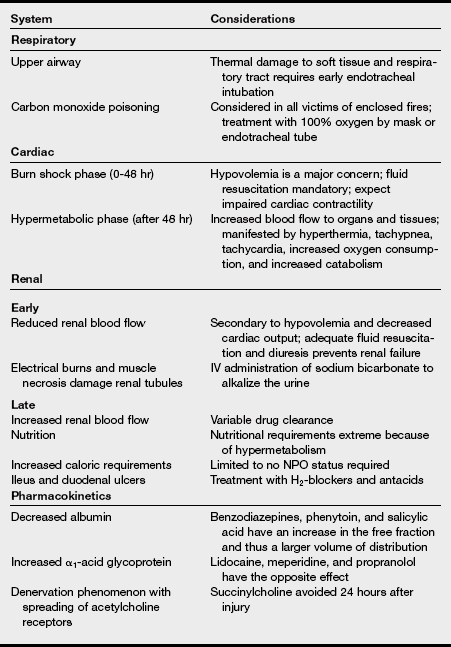
The pathophysiologic effects of major burns on each organ system are listed in the table below.
a) Burn patients require a thorough and complete preoperative assessment. A complete medical history, including laboratory studies, and a brief physical examination with lung auscultation, assessment of chest compliance, and inspection of the neck and oral cavity to evaluate for difficulties with intubation or reintubation should be implemented.
b) There are specific data unique to burn patients that anesthesia providers should know, including knowledge regarding the underlying trauma, the mechanism of burn (electrical, inhalation), the percentage of TBSA burned, the location of the burn sites, the area and the amount that the surgeon intends to débride, and whether the patient will undergo skin grafting during the perioperative course. The assimilation of this information affects the anesthetic plan in terms of anesthetic agents selected, appropriate monitoring, positioning, vascular access, and blood product requirements.
c) A review of prior anesthetic records can be helpful in determining the anesthetic plan. Quite often, this is possible to do because, more often than not, these patients make several trips to the operating room.
3. Pharmacologic considerations
a) Burn injury causes considerable changes in plasma protein levels, with significant consequences for the protein binding of drugs. In general, patients with burns exhibit decreased albumin and increased α1-acid glycoprotein levels.
b) Because the pharmacologic effect is often related to the unbound fraction of a drug, alterations in protein binding can also affect the efficacy and tolerability of drug treatment in patients with burns. This alteration causes the plasma binding of predominantly albumin-bound drugs, such as benzodiazepines, phenytoin, and salicylic acid, to be decreased, resulting in an increase in the free fraction and thus a larger volume of distribution (Vd) for the drug and possibly increased duration of action.
c) Drugs primarily bound to α1-acid glycoprotein (e.g., lidocaine, meperidine, propranolol) have the opposite effect.
d) Vd may be increased or decreased in patients with burns. In general, two factors may cause alteration in Vd: changes in extracellular fluid volume and changes in protein binding.
e) Fluid loss to the burn wound and edema can decrease plasma concentrations of many drugs. After the initial resuscitation state, cardiac output increases as the hypermetabolic phase develops. This increases blood flow to the kidneys and liver with increased drug clearance. Dosage requirements may change if the drug has a small Vd and a narrow therapeutic range. Overall, there is significant patient variability based on fluid status and phase of recovery.
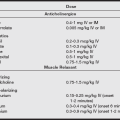
a) A successful anesthetic for the excision and grafting of a burn wound requires planning and preparing needed equipment. Specific anesthetic interventions should be done for these patients before their arrival into the operating room.
b) Plan preoperative anesthesia for the burn patient.
(1) Warm up the operating room ahead of time well before the patient arrives.
(2) Check on the patient’s blood status and order more blood and blood products if necessary based on the patient’s preoperative hemoglobin and hematocrit values, the size of the burn, and the extent of the planned débridement.
(3) Have the blood in the operating room and checked before surgical débridement is initiated. This is critical in pediatric patients.
(4) Have at least one blood warmer primed, plugged in, and turned on. If the burn is large, have two available.
(5) Make sure that you have adequate intravenous (IV) access before the surgeon begins débriding the burn.
(6) Because of hypermetabolism and pharmacologic tolerance that occurs, narcotic requirements may be extreme.
(7) Know whether invasive lines will need to be placed and plan ahead of time.
c) Complete blood count, electrolytes, blood urea nitrogen, creatinine, glucose, urinalysis, prothrombin time, partial thromboplastin time (D-dimer or fibrin split products if disseminated intravascular coagulation is suspected), type and crossmatch (number of units depends on the area to be débrided or grafted), chest radiography, and arterial blood gases (with carboxyhemoglobin if indicated) are obtained. Other tests are done as suggested by the history and physical examination.
d) Begin volume replacement with crystalloid or blood, or both, preoperatively. If the patient’s condition permits, an anxiolytic (e.g., benzodiazepine) and a narcotic may be useful preoperatively.
5. Equipment and room preperation
a) Burn patients require all the standard monitors intraoperatively. It can be challenging at times to adapt the standard monitors to the burn patient.
b) Electrocardiogram (ECG) leads are often difficult to place secondary to a lack of intact skin. It may be necessary to staple the leads or use needle electrodes on the patient to obtain an acceptable ECG tracing.
c) Ideally, blood pressure cuffs should be placed on an unaffected limb or, at times, at a nonsurgical site.
d) The placement of an arterial line for blood pressure monitoring may be warranted even in a healthy patient if the planned amount of surgical débridement is extensive or if manipulation of the patient’s limbs intraoperatively limits the accuracy of noninvasive cuff readings. In large burns that are greater than 20% to 30%, TBSA invasive blood pressure monitoring should be instituted after induction, if not already in place preoperatively. Rapid blood losses, the potential for hemodynamic swings, and the need to check intraoperative laboratory values all validate this requirement.
e) The standard sites for pulse oximetry placement may not be available. Alternative sites include the nose, ear, and cheek.
f) Any preexisting invasive monitors such as arterial line catheters or central venous or pulmonary artery catheters should be continued in the operating room.
g) Accurate temperature monitoring is essential because burn patients can become very hypothermic intraoperatively. Temperature measurements should be obtained through an esophageal stethoscope. Skin temperature devices are highly inaccurate, and there may not be a suitable place to place one.
h) Patients with burns who are critically ill are usually transported directly to the operating room from the burn intensive care unit and vice versa postoperatively by the anesthesia provider. These patients are usually intubated, are receiving continuous infusions of pharmacologic agents, and have invasive lines in place. Astute monitoring of the patient’s vital signs during transport is mandatory. Care must be taken while transporting the patient to not disrupt or dislodge any invasive or IV lines. A portable oxygen delivery system is another component of required transport equipment. Careful handling and vigilant guarding of the airway are vital. The anesthesia provider must also consider the patient’s comfort and privacy during transport. Amnestic and analgesic drugs should be administered as needed.
i) Monitors: Standard. Needle electrodes may be needed for ECG. Blood pressure can be measured on the lower extremities; an arterial line or a cuff can be placed over the burned area with a sterile lubricated dressing after consultation with the burn specialist. Most patients with burns of more than 40% to 50% require an arterial line, a central line, and a pulmonary arterial catheter if they are hemodynamically unstable. Use caution in placement and avoid burned areas.
j) Additional equipment: Blood and fluid warmers. A heated circuit and warming blanket are used. Room temperature is increased. Burn patients are poikilothermic.
k) Positioning: Various positions may be required intraoperatively, depending on the area being treated. Assess limb contractures and stabilize fractures.
a) Acute airway problems are frequently addressed upon admission to the burn unit. In a patient with a major burn or one who has an inhalation injury, preoperative intubation is likely.
b) Succinylcholine administration is contraindicated because of the potential for life-threatening hyperkalemia. Some practitioners believe that succinylcholine can be used safely up to 24 hours after an acute burn.
c) In a nonintubated patient without an inhalation injury and whose airway is normal, induction and intubation of the airway can proceed as during any other anesthetic regimen.
d) Preoperative airway evaluation is necessary as with any other patient. The anesthesia provider should exert good judgment in determining the degree of intubation difficulty. If the airway appears difficult, fiberoptic intubation should be considered or at least readily available.
e) In a severely burned patient who is intubated preoperatively, vigilance is required to protect the airway from accidental extubation. Loss of the airway in the patient may be impossible to regain because of edema of the airway structures. In this instance, cricothyrotomy or tracheotomy may be necessary.
f) Securing of such an airway can be problematic. Tape does not readily stick to burned skin. The use of soft beard straps to secure an endotracheal tube is a good option, especially if the plan is to extubate the patient at the end of the case. Cloth ties encircled around the head are frequently used in the burn unit to secure endotracheal tubes and should not be disrupted.
a) Depending on the percentage of TBSA affected by the burn, temperature regulation can be problematic in burn patients. These patients are at high risk of hypothermia development resulting from the loss of the skin’s insulating mechanisms, radiation and evaporative heat losses, and the large amount of body surface area exposure intraoperatively.
b) The temperature in the operating room should be greater than 28° C. IV solutions and skin preparations should be warmed. All methods of heat conservation should be used while the patient is in the operating room.
c) The use of in-line Humidivents or low gas flows reduces evaporative respiratory tract heat loss.
d) Forced-air warming blankets are very effective, but their use can be limited. Over-body heating lamps can be used but need to be at a safe distance above the patient to prevent further skin burns. Plastic bags can also be used to insulate any exposed body parts not being treated surgically.
e) It is suggested that keeping a patient warm is more beneficial than rewarming. With hypothermia, vasoconstriction occurs that may curtail any later warming efforts. It has been shown that slow rewarming postoperatively in critically ill patients with burn injuries leads to an increase in mortality. If the patient becomes hypothermic even despite the best effort put forth, the surgeon needs to be advised to stop the procedure.
8. Fluid and blood replacement
a) Surgical burn débridements may result in excessive blood loss. Wound management involves removal of the burn eschar layer until brisk bleeding of the dermis is reached.
b) The surgical team may remove the eschar so rapidly that it becomes difficult to keep up with the massive blood loss, resulting in a suddenly hypovolemic patient. Some institutions stop the surgical procedure after 2 hours if more than two blood volumes have been lost or if the body temperature falls to 35° C or by greater than 1.5° C from baseline.
c) There are many formulas to approximate the amount of potential blood loss for a burn débridement. These vary from 200 to 400 mL of blood loss for each 1% of TBSA excised and grafted to as high as 4% to 15% of the patient’s blood volume for every percent of skin débrided.
d) During and especially after the excision and débridement, gauze pads soaked in a vasoconstrictor (e.g., epinephrine, phenylephrine) are placed on the newly excised wound to control the bleeding. However, this may result in systemic absorption of vasoconstrictors, causing elevation of the patient’s blood pressure even in the presence of hypovolemia. Thrombin-soaked sponges may be preferred for patients whose systemic absorption of epinephrine may cause myocardial ischemia or arrhythmias.
e) Adequate venous access is a must before the initiation of surgical débridement. The size and extent of the burn will mandate how much access is needed. It is optimal to have two large-bore peripheral IV lines in place to ensure the administration of fluids and blood products quickly.
f) Critically ill patients often have a central venous catheter in place, especially if the burn is extensive and access is difficult. Although a triple-lumen catheter is adequate in the intensive care unit setting, it may not be ideal in the operating room when fluid and blood replacement is needed quickly.
g) The readiness of blood and blood products should be ascertained before the patient is brought to the operating room. Ideally, the blood should be in the operating room, checked, and ready to use at the beginning of the surgical procedure. This is particularly necessary in pediatric patients. Some hospitals initiate blood transfusions before the beginning of the surgical débridement and apply compression dressings after excision and grafting.
h) Careful planning is necessary to manage the hemorrhage and potential complications associated with massive transfusion (citrate toxicity, loss of clotting factors) during the débridement. Visual estimation of the blood loss is subjective at best and is prone to be miscalculated. Suction is not used during débridements. Sponges may be accidentally thrown away or covered up during the procedure. Blood drips onto the floor, is covered up in the surgical drapes, or leaks under the patient, and it is possible to be lulled into a false sense of security immediately after the eschar incision. Proper monitoring of the patient’s urinary output, hematocrit, and hemodynamic status is necessary for keeping the patient’s volume within normal limits.
i) One IV catheter is adequate for the induction of anesthesia in most burn patients, but at least two large-bore IV catheters are necessary before beginning a major excision and grafting procedure. The use of central venous or pulmonary artery catheters is patient dependent. The risk of sepsis in immunosuppressed patients must be weighed against the benefit of information gained.
j) The guidelines for fluid resuscitation and urine output are listed in the box and table on pg. 474.
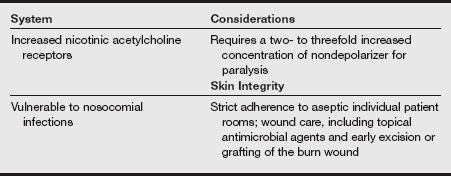
(1) There is no single best anesthetic agent to administer to burn patients. The anesthetic is individualized and should be based on the patient’s preoperative status and medical history.
(2) The patient with an acute burn seldom comes to the operating room immediately after the injury. Patients are usually admitted and stabilized in the burn unit. If the patient requires surgery, the anesthesia provider must realize that the burn patient is quite “fragile” within the first 24 hours of the injury. Anesthetic agents can exert extreme depressant effects, especially if fluid resuscitation is not adequate or has not been fully completed. The loss of intravascular volume coupled with the potential for a depressed myocardium can result in a hemodynamically unstable patient under general anesthesia.
(3) Careful and slow titration of all anesthetic agents is vital. Premedicating stable patients with a benzodiazepine or a narcotic decreases anxiety and makes transfer to the operating room tolerable. Anxiety, depression, and pain are common in patients with burns.
(4) To minimize patient discomfort, induction can be performed on the patient’s intensive care unit bed before moving the patient onto the operating room table.
(5) Regional anesthesia is sometimes considered for burn trauma limited to a small area or an extremity or for surgery during the reconstructive phase.
(a) One advantage of this technique is prolonged postoperative analgesia. Regional anesthesia is generally limited for a variety of reasons.
(b) The anesthesia provider must avoid performing any regional technique through burned tissue because of the potential for the spread of infection.
(c) There is an almost universal presence of hypotension (hypovolemia) and vasodilation with or without sepsis, which is a relative contraindication to the use of spinal or epidural routes for pain control until the burn wound is closed.
(d) Coagulopathy and cardiorespiratory instability are also reasons to avoid a regional anesthetic technique. The greatest limitation to the use of regional anesthesia is the extent of the surgical field. The anesthetized region must include both the area to be excised and the area to be harvested for donor skin.
(e) In children, regional anesthesia blocks are sometimes a viable option for postoperative analgesia. A tried and true regional block to institute in children undergoing débridements in the lower extremities or skin harvesting from the buttocks or thighs is a single-shot caudal technique. This can be placed either after the induction of general anesthesia or at end of the case before emergence. Injection of bupivacaine 0.25% and levobupivacaine 0.25% with epinephrine 1:200,000 added are two options. The volume of local anesthetic injected into the caudal space is determined by the child’s weight in kilograms and the analgesia level needed to be covered by the block. If the child is to be admitted postoperatively, the addition of morphine, at 30 to 50 mcg/kg, or clonidine, at 1 to 2 mcg/kg, can be added.
(6) Etomidate maintains hemodynamic stability during induction with less respiratory depression than barbiturates. However, repeated doses may inhibit adrenocortical function.
(7) Propofol has greater negative inotropic effects than does etomidate, which may lead to hypotension after induction. The high lipid content of propofol may limit its use during initial resuscitation and in septic patients.
(8) Another IV anesthetic is ketamine, a phencyclidine derivative that produces a dissociative anesthetic state of relatively short duration. Ketamine offers the advantage of stable hemodynamics and analgesia. Low doses produce adequate amnesia and analgesia for the débridement of superficial burns; higher doses may be administered for more extensive procedures, such as eschar excisions. Hallucinogenic episodes can be minimized with the administration of benzodiazepines in small doses, and an anticholinergic prevents excessive pharyngeal and tracheobronchial secretions.
(9) In the pediatric burn patient, inhalation induction with sevoflurane is certainly acceptable if the child does not have IV access before induction and if the airway appears normal.
(10) Anesthesia should be maintained with opioid or inhalational agents as the hemodynamic status of the patient permits. Inhalation agents have proved to be safe and effective, allowing rapid adjustment of anesthetic depth and the administration of high oxygen concentrations. The burn patient may be sensitive to the cardiovascular depressant effects of inhaled anesthetics, especially if acute fluid resuscitation is incomplete. Inhaled agents do not provide analgesia during the postsurgical period.
(11) Intubated burn patients frequently continued ventilation with specialized critical care ventilators (e.g., percussive ventilators) intraoperatively to maintain adequate oxygenation and ventilation. In this instance, a total IV anesthetic is indicated.
(l2) The main group of anesthetic agents that can exert altered effects in the burn patient are the muscle relaxants. Within the first 24-hour window after the burn injury, the burn is considered stable. Succinylcholine is probably safe to use within this time frame. As stated previously, the postjunctional acetylcholine receptors begin to proliferate soon after a burn injury occurs. This phenomenon is thought to be fully complete by 7 days after the acute injury. Succinylcholine given after the initial first 24-hour window has produced significant hyperkalemia as a result of this upregulation of receptors.
(13) Nondepolarizing muscle relaxants are safe to use in burn patients. Anesthesia providers should realize that patients may demonstrate a resistance to their effects. Higher dosing or more frequent redosing may be necessary. The origin of the phenomenon again is thought to result from the increase in postjunctional acetylcholine receptors. Because responses to nondepolarizing muscle relaxants can vary significantly, neuromuscular blockade monitoring should always be used.
(1) The postoperative anesthetic course should be planned in advance and is frequently intuitive. Critically ill and intubated burn patients are kept intubated postoperatively and are directly transported to the burn unit.
(2) The anesthesia provider should safeguard the airway and be respectful of the patient’s need for sedation and analgesia during this terminal phase of the anesthetic.
(3) If the patient is to be extubated, emergence from anesthesia should be planned in advance as well, similar to any other patient undergoing an anesthetic.
(4) Neuromuscular blockade should be adequately reversed and, if possible, the patient should be allowed to begin spontaneously breathing at an appropriate time.
(5) Narcotics for postoperative analgesia should be titrated according to the patient’s respiratory status. Keep in mind that these are painful procedures, and patients’ narcotic requirements can be tremendous.
B Trauma
Trauma is the fifth leading cause of death in the United States. Mortality is related to the age and prior condition of the patient, the type and severity of the trauma, and the response time for emergency treatment received.
The time allowed for preoperative assessment is limited and is based on the severity of the trauma. A rapid assessment and review of pertinent patient data available are essential. Blood therapy and the establishment of multiple large bore IV lines are priorities. The preoperative considerations are listed in the following box.
a) Cardiac: Assess for symptoms of shock listed in the following table. Assess the chest wall for obvious contusion, or instability, and assess stability of vital signs.
Classification of Hemorrhagic Shock
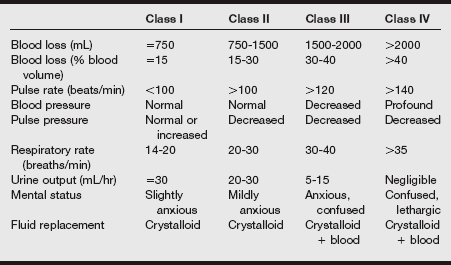
Adapted from American College of Surgeons, Committee on Trauma. Shock. In American College of Surgeons, ed. Advanced trauma life support course for physicians. 7th ed. Chicago: American College of Surgeons; 2004:74:108.
b) Respiratory: Assess breath sounds and patterns of respiration.
c) Neurologic: Assess patient using the Glasgow Coma Scale (GCS). Assume a cervical spine injury until it is definitively ruled out by x-ray examination or computed tomography (CT). There are three categories of the GCS to which a value is assigned: eye opening, motor response, and verbal response. For eye opening: 4 = spontaneous, 3 = to speech, 2 = to pain, and 1 = none. For motor response: 6 = to verbal, 5 = localizes to pain, 4 = withdraws to pain, 3 = decorticate flexion to pain, 2 = extends to pain, and 1 = none. For verbal response: 5 = oriented, 4 = confused, 3 = inappropriate words, 2 = incomprehensible sounds, and 1 = none. A normal GCS score is 15. A score of 8 or less indicates a severe brain injury.
d) Renal: Assess the color and amount of urine.
e) Gastrointestinal: All trauma patients are considered to have a full stomach. Gastric emptying slows or stops at the time of the trauma. The presence of a nasogastric tube also provides a “wick” that may allow gastric fluid: to be aspirated.
f) Endocrine: The release of stress hormones transiently elevates blood glucose levels.
g) Hematologic: Severe physical stress can lead to coagulopathies, as can dilution of clotting factors during massive volume resuscitation.
(1) Baseline laboratory tests are obtained as available: hemoglobin, hematocrit, and others as indicated by history and physical examination.
(2) Type and cross-match for at least 4 units.
(3) Other diagnostic tests are as indicated by history and physical examination.
(4) Premedication is usually avoided but can be individualized in trauma patients.
a) Standard monitoring equipment
b) Difficult airway equipment such as multiple laryngoscope blades, video laryngoscope, laryngeal mask airway (LMA) of various sizes, intubating LMA, bougie stylet, and emergency airway access kits.
c) Arterial line, arterial blood gas measurement, pulmonary artery catheters, blood warmers, rapid infuser, and patient warming equipment
d) Full range of standard and emergency resuscitative drugs immediately available
e) Transesophageal echocardiogram capabilities can aid in the assessment of heart function.
Immediate establishment of the airway is the priority. Anesthetics are introduced depending on the stability of the patient as assessed by vital signs and physical assessment. Muscle paralysis is provided to facilitate surgical procedures, which can lead to intraoperative awareness in the trauma patient.
(1) This is individualized based on the patient’s condition and the severity of trauma.
(2) Rapid-sequence induction and immediate establishment of the airway are necessary.
(3) Ketamine, propofol, and thiopental (Pentothal) may be administered depending on hemodynamic status. The specific anesthetic considerations for various trauma conditions are listed in the boxes on pg. 480.
(1) Oxygen and muscle relaxants are required in critically injured patients.
(2) After assessment and stabilization, anesthetics are administered as appropriate and as tolerated by the patient.
(3) Blood loss should be closely monitored and transfusions initiated with the type-specific blood products unless an emergency transfusion is required using O negative blood.
(4) A 1:1:1 (packed red blood cells:fresh-frozen plasma:platelet) ratio should be considered during massive blood transfusions to limit the dilution of blood clotting factors.
(5) Blood gas analysis and coagulation status should be frequently considered during resuscitative efforts.
c) Emergence: Continued ventilation and management of all major systems are required in the immediate postanesthesia period.
Continued ventilation and observation of cardiac, respiratory, renal, and coagulation status are required for at least the first 24 hours in severely injured patients. These patients are transferred to the critical care unit for long-term management of multiple sequelae. Pain control may include narcotics, patient-controlled analgesia, or regional block. Common problems in trauma are listed in the following boxes.