10 Procedural Sedation
• Procedural sedation refers to the technique of administering sedatives or dissociative agents with or without analgesics to induce a state that allows the patient to tolerate unpleasant procedures while maintaining cardiorespiratory function.1,2
• Procedural sedation with analgesia in the emergency department is generally intended to create a depressed level of consciousness that allows the patient to maintain control of the airway and oxygenation without continuous assistance.
• Patients must be assessed before sedation to proactively identify potential difficulties associated with disease states and airway maintenance.
• When drugs are used in combination, their effects are more than additive, and this can be beneficial or can potentiate respiratory depression and cardiovascular instability.
• In patients with liver disease, the metabolism of drugs is altered in many ways and it is difficult to predict effects.
• In patients with a recent history of opiate and benzodiazepine overuse, propofol may offer advantages over other agents.
Definitions
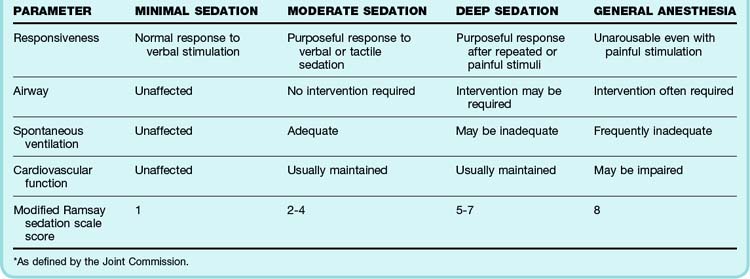
Procedural sedation, not including dissociative agents, represents a continuum of sedation ranging across defined levels of consciousness. These varying degrees of awareness have been termed minimal sedation (anxiolysis), moderate sedation, deep sedation, and general anesthesia. See Table 10.1 for general definitions as defined by the Joint Commission. Because patients can move from one state or level of awareness to another without warning, serial assessment and close hemodynamic monitoring are advised.
Indications for Procedural Sedation and Analgesia in the Emergency Department
Patients often arrive at the emergency department (ED) with acute injuries or disorders that require timely intervention to reduce both the physical and the psychologic effects of pain, anxiety, disability, and life-threatening complications. Common indications that may require procedural sedation are listed in Box 10.1.
Patient Monitoring
Because individual patient responses to sedatives and analgesics often vary, constant monitoring is essential to identify subtle changes in respiratory effort and hemodynamics. American College of Emergency Physician guidelines re-commend that patients selected for procedural sedation and analgesia (PSA) undergo continuous cardiac monitoring, continuous pulse oximetry, and documented blood pressure checks every 5 minutes during the procedure and in the postprocedural period.2 Box 10.2 provides a list of objective physiologic parameters recommended for safe bedside monitoring. In addition, see Table 10.2 for the six-point Ramsay sedation scale, which was initially validated in intensive care units for the assessment of sedation depth and later modified to correlate with the Joint Commission definitions of sedation.
| CLINICAL SCORE | LEVEL OF SEDATION ACHIEVED |
|---|---|
| 1 | Patient agitated, anxious |
| 2 | Patient cooperative, oriented, and tranquil |
| 3 | Patient responds to commands only |
| 4 | Brief response to light glabellar stimuli or loud auditory stimuli |
| 5 | Sluggish response to light glabellar tap or loud auditory stimuli |
| 6 | No response to light glabellar tap or loud auditory stimuli |
Capnometry (End-Tidal Carbon Dioxide Monitoring)
Many PSA agents decrease tidal volume and the respiratory rate, thereby creating the potential for hypoventilation and apnea. In the majority of patients, pulse oximetry readings correlate well with arterial O2 saturation values. Unfortunately, oximetry is ineffective in the early detection of hyperventilation-induced hypercapnia, particularly if patients are receiving supplemental oxygen. Growing evidence for the routine use of continuous capnography during procedural sedation has led to its increased clinical use in an attempt to identify hypoventilation and avoid unrecognized periods of apnea.2 This monitoring technology may have its greatest benefit in patients whose ventilation status cannot be visualized (e.g., covered with a sterile sheet). Although clear evidence demonstrating differences in clinical outcomes with its use is not yet available, end-tidal CO2 monitoring is probably useful in providing an added level of safety when perform-ing PSA.
Pulse Oximetry
Pulse oximetry readings may be misleading for a variety of reasons. The emergency physician must be aware of the pitfalls of this modality to correctly address changes in oxygenation (Table 10.3).3,4
| Low perfusion states | Low cardiac output, vasoconstriction, or hypothermia |
| Motion artifact | The most common source of error |
| Nail polish | Black, green, and blue nail polish have the same light absorbency: 660 and 940 nm |
| Type of probe and location | Ear probes have rapid response time. Accuracy of reading dependent on patient’s perfusion state and heart rate |
| Ambient light | Falsely low O2 saturation with fluorescent and xenon surgical lamps |
| Dyshemoglobinemias: carboxyhemoglobin, methemoglobin | Overestimation of true O2 saturation |
| Transient hypoxia consistent with patient’s normal sleep patterns | Inherent disadvantage of oximetry with insignificant hypoxic episodes |
Monitoring Depth of Sedation
Bispectral Index Monitoring
Electroencephalographic (EEG) bispectral index monitoring has been studied for use in the ED as a means of avoiding hypercapnia and hypoxic events and to objectively determine the depth of sedation during PSA. The bispectral index is a statistical numeric value based on bispectral processing of the last 15 to 30 seconds of the harmonic and phase relationship of the frontal lobe EEG data. A score of 90 to 100 represents an awake state; 70 to 80, a moderate sedation state; 60 to 70, a deep sedation state; 40, general anesthesia; and 0, consistent with brain death. These scores can vary with the PSA used and in individual patients.5 The use of combination PSA agents makes titrating to a predefined bispectral index value difficult because of the synergistic effect of the agents.6,7 Evidence is insufficient to recommend the routine use of such monitoring in the ED.2
Preprocedural Considerations and Risk Assessment
General Considerations
• History: past medical history, anesthesia history, medications, allergies, review of systems, time of last meal
• Physical examination: vital signs (blood pressure, pulse rate, respiratory rate), pulse oximetry, airway assessment, cardiopulmonary and neurologic examinations
Risk Assessment
Figure 10.1 presents an algorithm for evaluation before sedation.
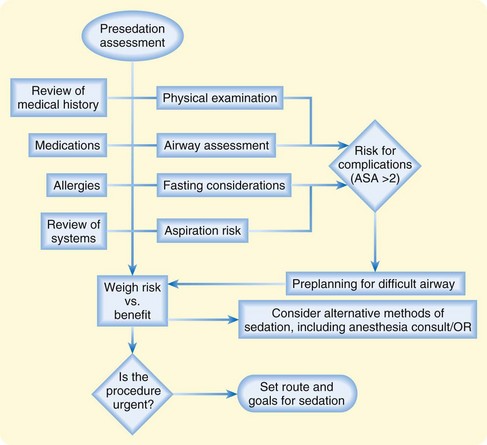
Fig. 10.1 Algorithm for evaluation before sedation.
ASA, American Society of Anesthesiologists [score]; OR, operating room.
Airway Evaluation
Assessment of the patient for potentially difficult bag-mask ventilation because of facial, oral, or neck anomalies is important before administration of PSA. Use of the mnemonics MOANS and LEMONS has been described as an aid in identifying anatomic and clinical features that may pose potential difficulties in airway management should bag-mask ventilation or intubation become necessary (Box 10.3).8
Box 10.3 Use of the Mnemonics MOANS and LEMON for Preprocedural Airway Assessment for a Difficult Airway
MOANS: Difficult Bag-Mask Ventilation
M: Mask seal—bushy beards, distorted lower facial contour
O: Obesity/obstruction—morbidly obese patients (because of increased redundant upper airway tissue) and patients with disorders that obstruct the upper airway
A: Age older than 55 years because of decreased muscular tone of the upper airway
N: No teeth, which creates difficulty in achieving an adequate mask seal
S: Stiff—patients with stiff noncompliant lungs, such as those with COPD, asthma, CHF, and pulmonary fibrosis
LEMON: Difficult Intubations
L: Look externally for physical features that may make intubation difficult—small mandible, large teeth, large tongue, short neck
E: Evaluate with the 3-3-2 rule:
M: Mallampati score—ability to visualize the posterior oropharynx with opening of the mouth
O: Obstruction—upper airway obstruction, stridor, odynophagia, and dysphagia
N: Neck mobility—immobilization because of cervical trauma, arthropathies
CHF, Congestive heart failure; COPD, chronic obstructive pulmonary disease.
Fasting Considerations
No compelling evidence is available to support fasting in the emergency setting for either children or adults. The emergency physician may consider a patient’s history of recent oral intake when determining the appropriateness of the depth of sedation and the complexity of a procedure, especially in patients at higher risk for airway compromise and complications. Prudence and good clinical judgment are paramount.2
Pharmacodynamics and Pharmacokinetics of Common Agents
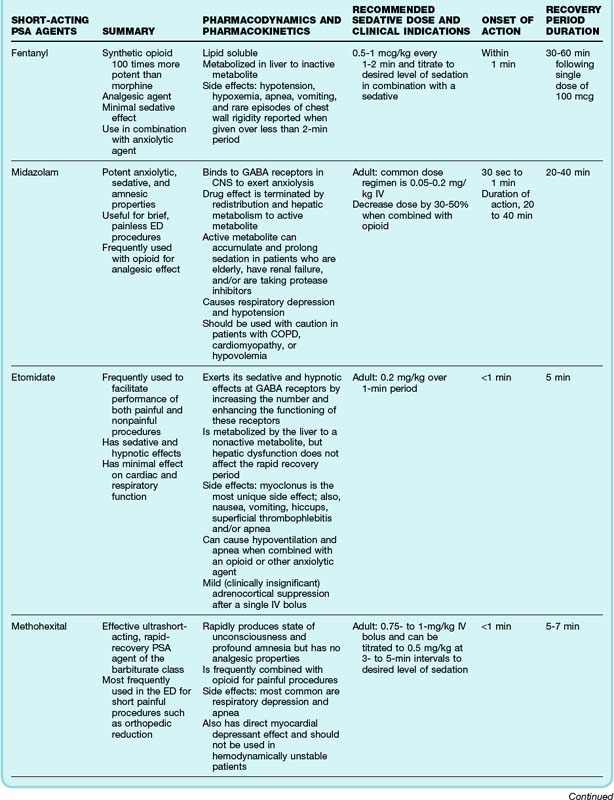
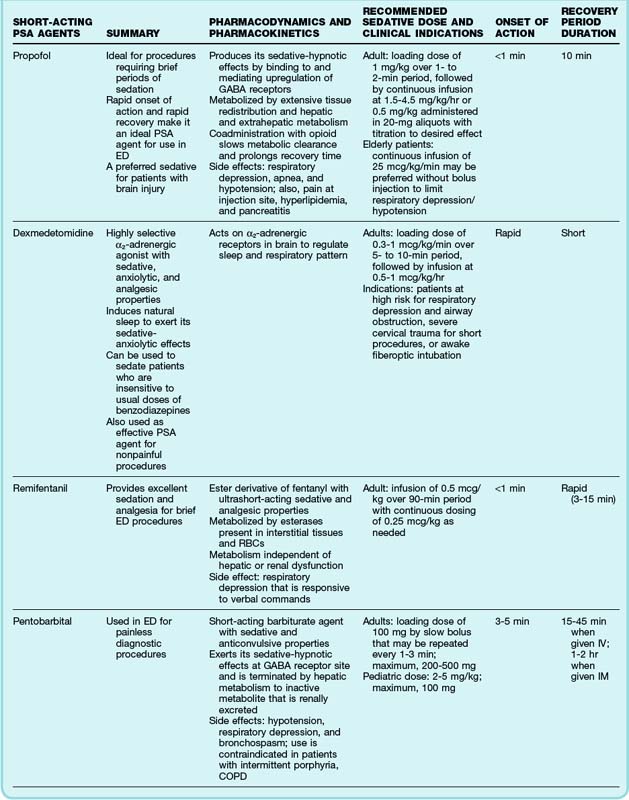
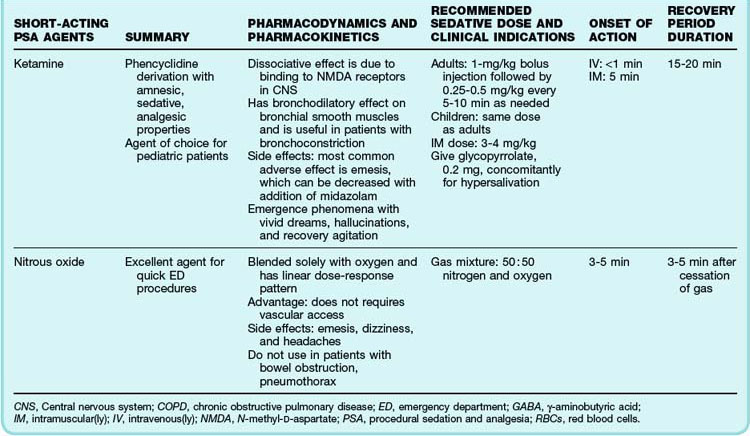
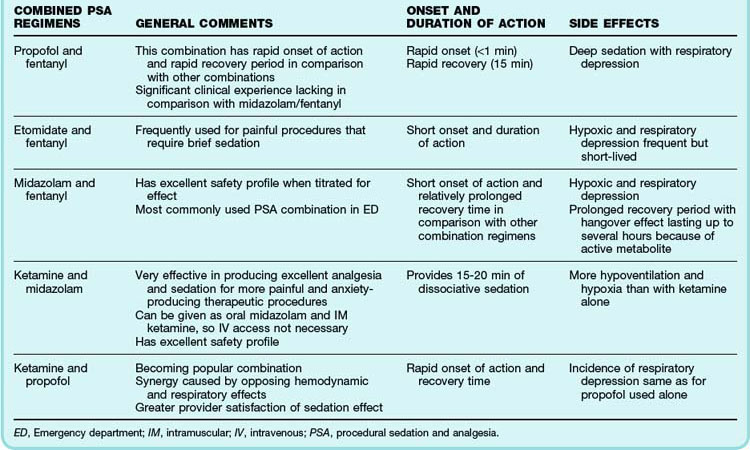
In view of the array of procedures requiring PSA in the ED and the varied underlying clinical disorders, an understanding of the pharmacology of individual agents is important. Such knowledge allows the provider to tailor sedation and analgesia to meet individual patients’ needs. A number of agents are well suited to the ED environment because of their rapid onset of action, brief recovery period, and minimal untoward effects. It is difficult for a single agent to meet all the sedative and analgesic goals of an individual patient, and a combination of drugs is sometimes used. Table 10.4 details the pharmacology of individual PSA agents,9–15 and Table 10.5 details the drug effects of commonly used combination pediatric regimens.16,17 A list of reversal agents for PSA can be found in Box 10.4.
1 American College of Emergency Physicians. Clinical policy for procedural sedation and analgesia in the emergency department. Ann Emerg Med. 1998;31:663–677.
2 American College of Emergency Physicians. Clinical policy for procedural sedation and analgesia in the emergency department. Ann Emerg. 2005;45:177–196.
3 Cote CJ, Goldstein EA, Fuchsman WH, et al. The effect of nail polish on pulse oximetry. Anesth Analg. 1989;67:683–686.
4 Tobin MJ. Respiratory monitoring. JAMA. 1990;264:244–251.
5 Miner J, Biros M, Seigel T, et al. The utility of the bispectral index in procedural sedation with propofol in the emergency department. Acad Emerg Med. 2005;12:190–196.
6 Barr G, Anderson RE, Samuelsson S, et al. Fentanyl and midazolam anesthesia for coronary bypass surgery: a clinical study of bispectral electroencephalogram analysis, drug concentrations and recall. Br J Anaesth. 2000;84:749–752.
7 Kissin I. Depth of anesthesia and bispectral index monitoring. Anesth Analg. 2000;90:1114–1117.
8 Murphy MF, Walls RM. Identification of the difficult and failed airway. Walls RM, Murphy MF. Manual of emergency airway management, 2nd ed, Philadelphia: Lippincott Williams & Wilkins, 2004.
9 Kennedy RM, Luhmann JD, Luhmann SJ. Emergency department management of pain and anxiety in orthopedic fracture care. Pediatr Drugs. 2004;6:11–31.
10 Bahn E, Holt K. Procedural sedation and analgesia: a review and new concepts. Emerg Med Clin North Am. 2005;23:503–517.
11 Beers R, Camponesi E. Remifentanil update: clinical science and utility. CNS Drugs. 2004;18:1085–1104.
12 Buttershill AJ, Keating GM. Remifentanil: a review of its analgesic and sedative use in the intensive care unit. Drugs. 2006;66:365–385.
13 Schenart CL. Adrenocortical dysfunction following etomidate induction in emergency department patients. Acad Emerg Med. 2001;8:1–7.
14 Green SM, Krauss B. Clinical practice guideline for emergency department ketamine dissociative sedation in children. Ann Emerg Med. 2004;44:460–471.
15 Minor JR, Burton JH. Clinical practice advisory: emergency department procedural sedation with propofol. Ann Emerg Med. 2007;50:182–187.
16 Godambe SA, Elliot V, Matheny D, et al. Comparison of propofol/fentanyl vs ketamine/midazolam for brief orthopedic procedural sedation in pediatric emergency department. Pediatrics. 2003;112:116–123.
17 Muellejans B, Matthey T, Scholpp J, et al. Sedation in the intensive care unit with remifentanil/propofol versus midazolam/fentanyl: a randomized, open-label, pharmacoeconomic trial. Crit Care. 2006;10:R91.