Principles of treatment
Introduction
Cyriax had a straightforward opinion about treating orthopaedic problems:
It is obvious that the method of treatment will depend largely on the existing type of disorder.
In orthopaedic medicine, disorders may be grossly categorized as follows:
• Traumatic – an injury resulting either from one single trauma or from multiple small traumas, the so-called overuse injuries
• Inflammatory – rheumatoid: poly- or monoarticular, infectious, traumatic
• Internal derangement – loose bodies and displaced menisci in peripheral joints and intervertebral disc displacements in the spine
• Functional disorders – instability, weakness, proprioceptive disturbances
• Psychogenic pain – there is no existing functional or anatomical explanation for the pain.
Techniques
• Manipulation techniques (rapid, small-amplitude, thrusting passive movement – also called ‘grade C mobilization’) are used to reduce small cartilaginous displaced fragments both in the spine and in peripheral joints (loose bodies). Manipulation is also called for to restore normal mobility in a joint restricted by ligamentous adhesion and in subluxation of bones.
• Gentle passive mobilizations (grade A and B mobilizations) are used to stretch capsular adhesions and to improve the function of ligaments and tendons. In the treatment of traumatic injuries they are often used in combination with deep transverse massage.
• Active movements and proprioceptive training are needed in the treatment of functional disorders and instability. In the treatment of minor muscular tears they are very useful in avoiding the formation of abnormal intralesional adhesion formation.
• Injection and infiltration techniques are used to reduce traumatic or rheumatoid inflammation. They are most valuable in arthritis, bursitis, ligamentous and tendinous lesions and in neurocompression syndromes.
• Deep friction is a very useful technique in treating traumatic and overuse soft tissue lesions. The rationale for using deep friction (which is in fact a form of soft tissue mobilization) is supported by experimental studies of the past several decades that confirm and explain the beneficial effects of activity on the healing musculoskeletal tissues (see Connective tissue).
Repair and remodelling of healing tissues respond to cyclic loading and motion.1 Early motion and loading of injured tissues is not without risk, however, and excessive loading can inhibit or stop healing. Deep transverse friction imposes cyclic loading without bringing too much tension on the healing longitudinal structures of tendon or ligament and can therefore be considered as beneficial.
Deep transverse friction
Deep transverse friction (although the word friction is technically incorrect and would be better replaced by ‘massage’) is a specific type of connective tissue massage2 developed in an empirical way by Cyriax.3
Transverse massage is applied by the finger(s) directly to the lesion and transverse to the direction of the fibres. It can be used after an injury and for mechanical overuse in muscular, tendinous and ligamentous structures.4–6 In many instances the friction massage is an alternative to infiltrations with steroids. Friction is usually slower in effect than injections but leads to a physically more fundamental resolution, resulting in more permanent cure and less recurrence. Whereas steroid injection is usually successful in 1–2 weeks, deep friction may require up to 6 weeks to have its full effect.
Mode of action
Only a few studies exist,7,8,9 and more research is urgently needed. However, experienced therapists know in what kind of soft tissues they can expect good results with transverse massage and where the technique does not work. Transverse massage either is effective quickly (after 6–10 sessions) or not at all. Advice on indications, contraindications and modalities of the technique that are given in this book rely solely on the experiences of the authors and not on scientific research.
Relief of pain
It is a common clinical observation that application of local transverse friction leads to immediate pain relief – the patient experiences a numbing effect during the friction and reassessment immediately after the session shows reduction in pain and increase in strength and mobility. The time to produce analgesia during the application of transverse friction is a few minutes and the post-massage analgesic effect may last more than 24 hours.10 The temporary relief at the end of a session may prepare the patient for treatment with mobilization not otherwise possible, such as selective rupture of unwanted adhesions.
• Pain relief during and after friction massage may be the result of modulation of the nociceptive impulses at spinal cord level: the gate control theory (see Ch. 1). The centripetal projection into the dorsal horn of the spinal cord from the nociceptive receptor system is inhibited by the concurrent activity of the mechanoreceptors located in the same tissues. Selective stimulation of the mechanoreceptors by rhythmical movements over the affected area thus ‘closes the gate for pain afference’.
• According to Cyriax, friction also leads to increased destruction of pain-provoking metabolites, such as Lewis’s substances. This metabolite, if present in too high a concentration, provokes ischaemia and pain.3
• It has also been suggested that prolonged deep friction of a localized area may give rise to a lasting peripheral disturbance of nerve tissue, with local anaesthetic effect.
• Another mechanism through which reduction in pain may be achieved is through diffuse noxious inhibitory controls, a pain-suppression mechanism that releases endogenous opiates. The latter are inhibitory neurotransmitters that diminish the intensity of the pain transmitted to higher centres.11–13
Effect on connective tissue repair
Connective tissue regenerates largely as a consequence of the action of inflammatory cells, vascular and lymphatic endothelial cells and fibroblasts. Regeneration comprises three main phases: inflammation, proliferation (granulation) and remodelling. These events do not occur separately but form a continuous sequence of changes (cell, matrix and vascular changes) that begins with the release of inflammatory mediators and ends with the remodelling of the repaired tissue (see Ch. 3). Friction massage may have a beneficial effect on all three phases of repair.
Friction stimulates phagocytosis
It has been suggested that gentle transverse friction, applied in the early inflammatory phase enhances the mobilization of tissue fluid and therefore increases the rate of phagocytosis.14
Friction stimulates fibre orientation in regenerating connective tissue
During maturation, the scar tissue is reshaped and strengthened by removing, reorganizing and replacing cells and matrix.15
It is now generally recognized that internal and external mechanical stress applied to the repair tissue is the main stimulus for remodelling immature and weak scar tissue – with fibres that are oriented in all directions and through several planes – into linearly rearranged bundles of connective tissues.16 Therefore, during the healing period, the affected structures should be kept mobile by normal use. However, because of pain, the tissues cannot be moved to their full extent. This problem can be solved by friction. Transverse friction massage imposes rhythmical stress transversely to the remodelling collagenous structures of the connective tissue and thus reorients the collagen in a longitudinal fashion. Friction is thus a useful treatment to apply early in the repair cycle (granulation and beginning of remodelling stage): the cyclic loading on and motion of the healing connective tissues stimulates formation and remodelling of the collagen.17
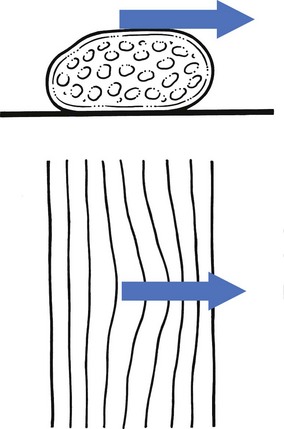
Friction prevents adhesion formation and ruptures unwanted adhesions (Fig. 5.1)
At a later stage when strong crosslinks or adhesions have formed, more intense friction is needed to break these down.18–21 The technique is then used to soften the scar tissue and to mobilize the crosslinks between the collagen fibres and the adhesions between healing connective tissue and surrounding tissues. This, together with the local anaesthesia produced, prepares the structures for mobilizations that apply longitudinal stress to the structures and rupture the larger adhesions.
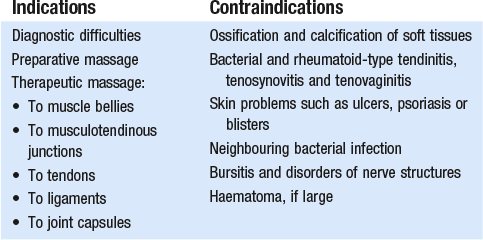
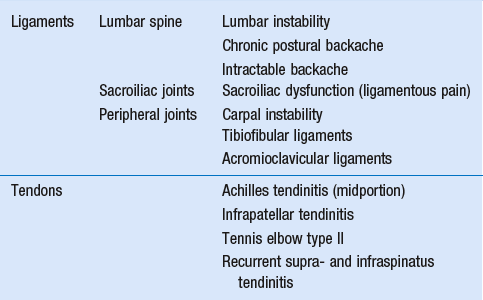
Indications
Therapy
Muscle bellies
Theoretically, friction can be used for all muscle belly lesions. However, some lesions respond so well to local anaesthetic infiltration that friction is not used. This is the case in type IV tennis elbow (lesion at the muscle belly of the extensor carpi radialis). On the other hand, sometimes no alternatives exist to treatment with deep transverse friction (Box 5.1). A lesion of the subclavius or intercostal muscles for instance can be treated only by deep transverse friction.
Tendons
Lesions at the tenoperiosteal insertion can be treated either with corticosteroid infiltrations or with deep transverse massage. Corticosteroid suspension quickly converts an inflamed and painful scar into one free of inflammation. However, the recurrence rate is rather high, between 20% and 25%.3 The aim of the massage is to get rid of the self-perpetuating inflammation by breaking up the disorderly scar tissue and adhesion formation by converting it into properly arranged longitudinal connective fibres. This takes longer but once cure is achieved there will be less of a tendency towards recurrence. It may therefore be a policy to start treatment with infiltrations but if the trouble recurs after a few months to substitute with massage.
Lesions in the tendinous body, either traumatic or resulting from overuse, are contraindications for infiltration with corticosteroids. Ruptures have been reported after intralesional steroid infiltrations of long tendons and therefore deep frictions are the treatment of choice here.22,23
Ligaments
It has been explained (see Ch. 3) that early mobilization is extremely important for swift and full recovery of ligamentous sprains. However, in advocating this, one main difficulty is encountered: the intensity of the initial inflammatory reaction. The slightest movement causes pain which forces the patient to immobilize the joint and the ligaments. However, during immobilization, regenerating fibrils quickly start to form randomly organized scar tissue, leading to crosslinks and adhesion formation. This problem can be solved by gentle transverse frictions. Rhythmic movement across the inflamed ligament eases the pain and the tissue can be moved to and fro in an imitation of its normal behaviour.
Joint capsules
Deep transverse friction can be applied to the capsules of the trapezium–first metacarpal joint, the temporomandibular joint and the cervical facet joints. The indication is traumatic arthritis or osteoarthrosis. Results are fair, provided the arthrosis is not too advanced. Indications and contraindications to friction are outlined in Table 5.1.
Contraindications
Technique
Position of the therapist and the hands
Three main techniques can be distinguished.
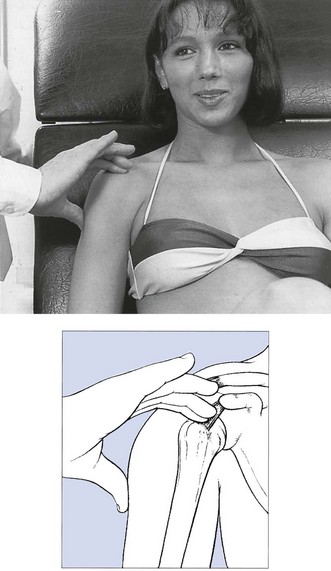
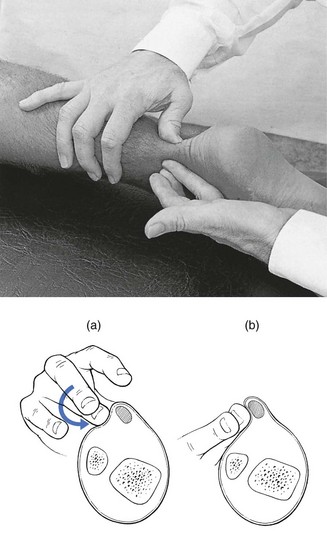
To-and-fro movements
These are used in the treatment of dense, round or flat collagenous bundles (tendons or ligaments) and in the treatment of tenosynovitis. The active phase is a sweep with the tip(s) of one or two digits across the tendinous structure. During the passive relaxation phase the finger is returned to the starting position, without losing contact between finger and skin. Movement is with the arm; friction is given by use of the pulpy part of the finger (Fig. 5.2). In large lesions, as in peroneal tendinitis, two or three adjacent fingers are used together. In deep-seated lesions as in tendinitis of the long head of biceps in the bicipital groove or at its insertion on the radius or in infraspinatus tendinitis, the thumb performs friction.
Counterpressure is usually provided to enable a good sweep. The finger(s) applying counterpressure and stabilization are most important in bringing those applying friction into the right position and also determining the direction of the friction. The thumb is used (to give counterpressure) when the sweep is performed by a movement of the index reinforced by the middle finger or the middle finger aided by the index finger. When the thumb does the massage, counterpressure is from the fingers (Fig. 5.3). The most common way of applying friction around a round edge on a flat surface is to use the index reinforced by the middle finger. Sometimes the opposite is done: the middle finger is reinforced by the index. Sometimes counterpressure is not given, for example in friction to the quadriceps expansion or intercostal muscles.
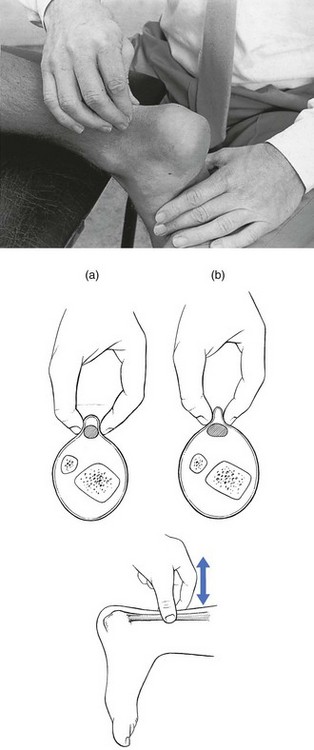
Pronation–supination
This technique is often used where the lesion is difficult to reach: the anterior aspect of the Achilles tendon, popliteus tendon and the dorsal interossei of the metacarpals. Massage is performed with the pulpy part of the third finger (long finger), reinforced by the index finger. The long finger is used because its long axis is the prolongation of the axis of pronation–supination rotation of the forearm (Fig. 5.4).
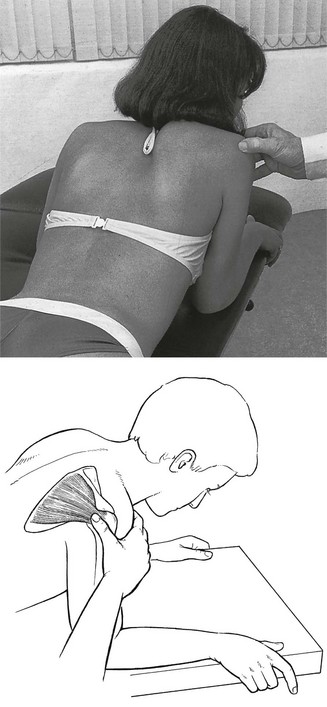
Pinch grip
This is the normal technique for a muscle belly. The pinch is between the thumb and the other fingers. The muscle is fully relaxed. The fingers are placed at one side of the affected area and the thumb at the opposite side (Fig. 5.5). By drawing the fingers upwards over the affected area, the therapist feels the muscle fibres escape from the grip until only skin and subcutaneous tissue remain.
Amount of pressure
The amount of pressure applied depends on three elements:
• The depth of the lesion: that friction must always reach sufficient depth to move the affected fibres in relation to their neighbours and sometimes the underlying bone or capsule, increased pressure must be applied to deeper structures.
• The ‘age’ of the lesion: recent sprains and injuries require only preventive friction because crosslinks or adhesions have not had time to form. In long-standing cases more pressure is needed to get rid of these. However, pressure should always be associated with movement and should not replace it because pressure alone is both painful and ineffective.
• The tenderness of the lesion: in severely inflamed lesions that are very tender to touch, friction with the usual amount of force may be very painful. Pain can be avoided by starting with a minimal amount of pressure – just enough to reach the lesion – and progressively increasing the force as treatment proceeds.
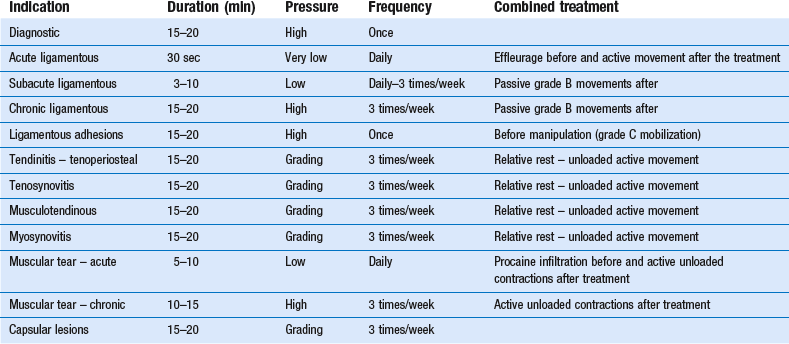
Duration and frequency
Treatment is stopped once the patient is pain-free during daily activities and functional tests are totally negative. Local tenderness may persist longer but disappears spontaneously because it is the outcome of repetitive hard pressure. However, in a minor lesion of a muscle belly, massage is continued for 1 week after full clinical recovery to prevent recurrence (see Table 5.2; see also Box 5.2).
Passive movements
• Grade A mobilization is a passive movement performed within the pain-free range.
• Grade B mobilizations are passive movements performed to the end of the possible range. The latter is indicated by an end-feel. All stretching and traction techniques are grade B mobilizations.
• Grade C mobilization is a minimal thrust with a high velocity and over a small amplitude. It is performed at the end of the possible range, i.e. the moment the therapist has reached the end-feel. Another word for grade C mobilization is manipulation.
Indications
Grade A mobilizations
To promote healing of injured connective tissue
Passive movements within the pain-free range are usually called for in the treatment of injured connective tissue. A comprehensive literature evaluation and meta-analysis of experimental studies of the past several decades have demonstrated that regeneration of injured connective tissue is significantly better with the application of continuous passive motion. If the healing tissues are not loaded, regeneration results in unstructured scar tissue. Under functional load, the collagen fibres are oriented in a longitudinal direction and the mechanical properties are optimized.24
Distractions at the shoulder
Grade A mobilizations are also used on the capsule of the shoulder in stage III arthritis when stretching and intra-articular steroids are contraindicated (see Ch. 14). In this condition, long-standing stimulation of the nociceptors has increased neuro-sympathetic activity, giving rise to vasoconstriction, muscle spasm and pain.
Deformity correction
Some cases of lumbago show persistent spinal deviation even after the pain has ceased. A quick thrust manipulation so effective in relief of pain is not effective in correcting the remaining deformity, but sustained translatory gliding in the opposite direction is most helpful. The movement is performed slowly and care is taken to keep the gliding within the pain-free range (see Ch. 40).
Grade B mobilizations
To stretch the capsule of a joint
• a limitation in the capsular pattern (see Ch. 4)
• demonstration of a hard-elastic end-feel to restricted movements (see Ch. 4).
In the very beginning of arthritis, muscle spasm forces the joint to be held in a position of ease, so restricting movement in some directions more than in others (see Capsular pattern, Ch. 4). Immobilization and inflammation cause disordered deposition of collagen fibres in the joint capsule and lead to the formation of capsular adhesions, which in turn are responsible for more restriction of movement and pain. Stretching aims at restoring mobility and function by breaking micro-adhesions and producing elongation of the shortened capsule. To be applicable, however, the ligamentous end-feel must be reached before the protective muscle spasm begins. To be successful, the therapist should therefore be able to differentiate between an elastic and a spastic end-feel.
Capsular stretching can be preceded by application of heat, either through short-wave diathermy or ultrasound. This can relieve some pain and seems to lower the viscosity of the collagenous tissue, allowing more movement for less force. In vivo studies on the effects of heat on ligament extensibility have shown that sustained force applied after elevating tissue temperature produced significantly greater residual elongation.25,26
Traction
Traction is used to separate articular surfaces from each other and can be employed in two ways: as an accessory to manipulation or as the sole treatment. Reducing a displaced fragment is obviously easier when the bone ends between which it lies are pulled apart. If the fragment projects beyond the articular edge, tautening of the ligaments and capsule also provides a centripetal force. In that traction diminishes the pressure on the fragment, pain decreases, which allows the patient to relax the muscles more.18 In the cervical and thoracic spines, traction is a built-in safety measure for protecting the spinal cord during manipulation (see below) although the use of traction for this purpose and at these sites does not imply that manipulation can be performed on a basis of ‘try and see what happens’ without a proper diagnosis.27
In the spine, traction is used as the sole treatment only in nuclear disc protrusions, which are rare at the cervical and thoracic levels but are more common in the lumbar area. Spinal traction is always mechanical and is performed with the help of a harness (lumbar or low thoracic) or a sling (cervical or upper thoracic). Spinal traction distracts the intervertebral disc spaces. It also pulls the apophysial joints apart and slightly widens the intervertebral foramina.27–31 At the same time, negative intradiscal pressure is produced with centripetal ‘suction’ on any protrusion. The posterior longitudinal ligament is tightened, which may help reduce a displaced fragment. All these elements are helpful in the progressive reduction of a nuclear disc protrusion. Reduction of herniated bulges has been demonstrated on epidurography31–33 and on CT scan34 during and after traction. The effect of traction depends on the amount of force applied, the length of time per session, the interval between each session and the total number of sessions.35
Grade C mobilizations
Manipulation of the spine
Introduction
A manipulation or grade C mobilization usually implies a single thrust of high velocity performed at the end of a passive movement after the ‘slack’ has been taken up, and over a small amplitude. It goes beyond the physiological limit but remains within the anatomical range. Precision of the movement and control of the applied force are required.36 Spinal manipulative therapy is a valuable method in the treatment of mechanical spinal disorders. Although it has not been scientifically validated, some studies have shown beneficial effect.37–40 However, its potential benefit should not be overestimated and the indications must be well defined and based on a sound clinical diagnosis. It must never be done as a test to see if it is effective. Therefore it should not be used on all those with back and neck pain although it may well cure a proportion who actually require it. To use McKenzie’s words:
Even if you have a hammer in your hand not everything you see is a nail. Therefore indiscriminate use of spinal manipulative therapy must not be made if the criticisms that have been justifiably levelled at chiropractice and osteopathy are to be avoided. The development of postgraduate courses in manipulation is welcome, although some have overvalued the benefits of manipulative therapy. All who undertake manipulation have experienced the feeling of pride and joy in producing cure. It is the duty of those who have more experience of the benefits and limitations of manipulative therapy to moderate the understandable enthusiasm of those entering the field – a few successes may quickly lead to the temptation to manipulate every patient for any disorder.41
Historical note
Osteopathy
Diagnosis is mainly based on palpation for restricted spinal mobility and treatment consists of a manipulative system in which joints are forced by a distant leverage. Cure is sought for all kinds of visceral and musculoskeletal disorders.27
Orthopaedic medicine
This term describes the system of diagnosis and treatment of musculoskeletal lesions introduced by J.H. Cyriax. It is the system on which this book is based. Diagnosis rests on careful history and functional examination. Treatment depends mainly on the type of lesion, and manipulation is applied only when indicated. In spinal manipulation, Cyriax proposed a fixed set of high-velocity, small-amplitude thrusts performed at a certain distance from the lesion and, characteristically for this method, usually under strong traction. The objective of Cyriax’s spinal manipulative techniques is to alter the discodural or discoradicular interaction by moving a displaced cartilaginous fragment away from the sensitive dura mater and dural nerve sleeve. Spinal rotation manipulations apply a torsion stress throughout a whole part of the spine, not at just one level. With an intact posterior longitudinal ligament and annulus fibrosus, some of this torsion force exerts a centripetal force by suction on the protruding disc material.42 This effect is not confined to one level and full reduction is not absolutely necessary for pain relief, in that when contact between dura and disc has ceased the problem is frequently solved.
Manual therapy
Treatment is characterized by rhythmic repeated movements within the physiological range. Oscillatory techniques had already been used by E. Cyriax (father of J.H. Cyriax) but were more widely employed by Maitland and later slightly changed by the different schools of manual therapy (Cyriax:3 p. 40). Pressure is applied to what is believed to be the appropriate level.
Orthopaedic medicine technique
Attention must be given to the following general matters, which are important for all manipulations.
Final thrust
Immediately after the slack has been taken up in the surrounding tissues, a minimal amplitude, high-velocity thrust is given to affect the target tissue. The velocity is of great importance because tissues loaded quickly are stiffer so that the manœuvre will affect only the displaced fragment of disc and will not damage the surrounding structures.43
The amount of force used for the final thrust depends mainly on the patient and manipulator in that a tall manipulator will have to use less force in a small patient and vice versa.44 The length of the lever (see later) is also important. The force should always be kept reasonable and may be progressively increased, according to the immediate result.
The manipulation thrust is often accompanied by an audible ‘pop’.29,45 Although it is a common belief that pops or clicks are provoked by the formation of a temporary vacuum, as occurs in small peripheral joints put under traction,46–48 this is not definitely established for the spine. An alternative and more likely explanation is movement of cartilaginous fragments, as may be heard during manipulation for a loose body in the knee or hip. If the clicks were simply the result of the collapse of a vacuum they should also be – but are not – heard during mechanical traction, in which the traction force is much higher.
Reassessment
After each manœuvre the patient is assessed, the criteria of success being the absence of symptoms and the restoration of pain-free movement. The patient and not the manipulator is the arbiter.49 Depending on the immediate outcome, the therapist decides whether to repeat the same manipulation, probably with increased strength, to try another manœuvre or to refrain from further manipulation.
Figure 5.6 outlines the assessment of spinal lesions and their manipulation.
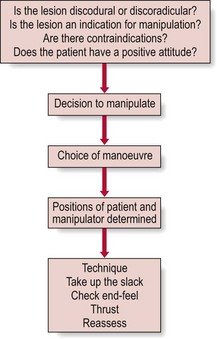
Fig 5.6 Spinal manipulation.
Selectivity of a manipulative treatment
Selectivity must be considered both in diagnosis and therapy.
Selectivity of diagnosis
The great variability in the extent of spinal stiffness between subjects, or at different levels within the one subject, makes the determination of areas of abnormally increased stiffness difficult. Increased stiffness may in fact be a normal variant and bear no relationship to the patient’s presenting symptoms. Few of those advocating segmental mobility tests have seriously examined the value of their tests. They have generally presumed that the tests were useful because their patients got better.50 However, several studies have failed to demonstrate the reliability of these tests.51–62 Therefore it must be made clear that judgement of small changes in the range of movement of a segment, in the absence of full restriction of movement, remains a very subjective finding, which depends mainly on the personal conviction of the examiner rather than on objective measurements. Moreover, in soundly based tests, findings must be reproducible and must show correspondence when performed by other investigators. In the establishment of ‘joint play’ the inter-observer discrepancy is too large to be acceptable.63 In 1973, Cyriax attended a demonstration in which five therapists, all of whom specialized in mobility testing, examined over a period of a few minutes a patient with a neck problem. There was no agreement between these specialists about the level of the lesion (C2, C3, C4, C5, C6 or T2), or about the direction of restriction (see Cyriax:64 p. 108). Similarly, a patient who had congenital fusion of the sacroiliac joints was examined by 10 manipulators. Each had his own diagnosis, such as left anterior sacrum, right anterior sacrum and bilateral posterior sacrum, although ‘the tests were very positive’ for all of them (see Maigne65 and Cyriax:64 p. 363).
Even if it were possible to identify with certainty localization of the hypomobile segment, the question remains as to whether this is also the site of the lesion. Studies have shown that frequently the lesion does not lie at the joint where motion is restricted but at one which appears to be normal.55 Moreover, other disorders such as osteophytosis, congenital fusion and ankylosing spondylitis all give rise to restricted movement which is usually painless.
Selectivity of manipulation
In orthopaedic medicine most manœuvres used are non-specific long-lever manipulations. These include all procedures in which a force is exerted on a part of the body some distance away from the area where it is expected to have its beneficial effect. Levers may include the shoulder, transverse processes and parts of the skull, pelvis or thigh (Frymoyer et al:45 p. 1594). Although some criticize the crudity of long-lever high-velocity manipulation it should be realized that it is not elegance, impressiveness, specificity or technical difficulty which count but effectiveness and safety. Furthermore, the use of a lever enables the manipulator to reach the lesion more effectively. During the preparative phase – on taking up the slack – all the normal joints are brought to their anatomical end position except for the joint that is blocked. When the additional thrust is given, the final extra pressure falls inevitably first and to the greatest degree on the deranged joint. The manœuvre thus becomes specific even though in general the techniques are regarded as non-specific.
Long-lever manipulations are in full contrast to what are called ‘specific’ short-lever high-velocity manipulations. Here the goal is to act specifically at what is believed to be the level of the lesion. The spinal segment and the facet joints adjacent to the lesion are locked by moving the spine to the physiological limit of passive movement and a high-velocity small-amplitude thrust is given to the short vertebral lever (transverse process or spinous process) in the specific direction that will liberate the restricted movement. However, it is technically not possible to lock all other joints and then to manipulate at just one level (Cyriax:64 p. 108). It was even demonstrated that by mobilizing the sacroiliac joints after locking of the lumbar spine, the largest movement took place between L4 and L5.66 Furthermore, if diagnosis fails to be absolutely right, how can there be certainty as to the exact level of the lesion to work on? Fortunately for those who employ ‘specific’ short-lever manipulations, these are much less specific than they think, because the manipulations actually cover a much larger part of the spine and so unintentionally also include the lesion.
Specificity is a false attribute. The methods that claim to lead to specific localization in both diagnosis and treatment are scientifically unacceptable. Claims of specificity are made in order to give prestige to manipulators who claim to feel something that cannot be felt. Manual therapists, chiropractors and osteopaths over-complicate their teaching and often create excessive patient dependency, instead of providing the patient with independence. Indeed, patients are encouraged to return at regular intervals for pointless prophylactic adjustment.41 We support R. McKenzie’s conclusion that demystification of spinal manipulative therapy is an urgent priority.41 Chiropraxy, manual therapy and osteopathy, however, thrive by creating the impression that there is something complex and exclusive about the practice of passive end-range motion that only experts in these practices can understand or have the skills to feel. The belief is strong that expertise in the understanding and delivery of spinal manipulative therapy requires 3 or 4 years’ training. The main advantages of the methods discussed in this book are that the manipulations are much simpler and at least as effective as those advocated by chiropractors, osteopaths and manual therapists. Non-specific long-lever manipulations are quickly effective, do not take long to perform and are simple to learn. Moreover, they can take only about 180 hours of tuition, provided that the student has already gained qualifications in medicine or physiotherapy.
Mode of action of spinal manipulation
To date, the mode of action of manipulation has not been totally clarified, although many different models have been put forward. All pose unsolved questions, lack objective confirmation and are subject to dispute. Different attitudes towards spinal disorders determine theories and explanations.67
Those who believe in ‘posterior facet joint’ syndrome as a frequent source of back pain, believe that manipulation corrects a posterior joint dysfunction, in which either a minor subluxation of a facet together with an entrapment of the synovial fold, or of part of a small intra-articular meniscus, is held responsible, both of which may give rise to a blocked vertebral joint (Kirkaldy-Willis:29 p. 296; Mathews and Yates68).
Others suggest that manipulation ruptures periarticular connective tissue adhesions or that it abolishes a muscle spasm.69 In our opinion, a manipulation does not directly affect muscle spasm; instead, the latter disappears secondarily when the underlying problem is solved.
It has also been suggested that manipulations influence the mechanism of cutaneous pain tolerance as the result of release of endorphins, or that stimulation of mechanoreceptors of the facet joint capsules, ligaments and annulus fibrosus influences the neurophysiological gate that controls the perception of pain.70 This could conceivably abolish pain immediately after manipulation but does not explain longer term improvement.
Some believe that manipulation may move an inflamed nerve away from the herniation71 or that relief is achieved via a return to normal of neurogenic reflex activity.42,72
We strongly believe that spinal pain is the result of disc protrusion that gives rise to a conflict between the posterocentral or posterolateral rim of the disc and the pain-sensitive dura mater or dural nerve sleeve, and that a displaced fragment of an intervertebral disc can be moved by manipulation.42,73–76
This was the hypothesis of Cyriax3 (see his pp. 38–50) and Maigne77 and has been supported by the observations of Mathews and Yates,68 who have shown by epidurography that in acute lumbago small lumbar disc protrusions diminished in size after manipulation. Manipulative interruption of contact, moving the displaced cartilaginous rim away from sensitive structures, is the objective for relief of pain and is best obtained by a non-specific long-lever, high-velocity manipulation.
Contraindications to spinal manipulation
Bleeding disorders and anticoagulant use
When normal clotting of blood is not guaranteed, as in congenital or acquired (liver disease) bleeding disorders or because of the administration of anticoagulants (Box 5.3), spinal manipulations are potentially dangerous. Disastrous results can follow, such as intraspinal haemorrhage with the formation of a haematoma that may lead to sensory and motor deficit, to paraplegia, quadriplegia or death.78 For this reason, a coagulopathy is an absolute contraindication to spinal manipulations. Manipulation can be safely performed only after blood clotting tests have returned to normal.
Spinal tumours, unstable fractures, vertebral infections and severe osteoporosis (see Grieve:27 p. 829)
Rheumatoid arthritis, psoriatic arthritis, Reiter’s syndrome and ankylosing spondylitis
The first three of these may be associated with ligamentous laxity and gross destruction of the joint with subsequent instability. Manipulation must not be undertaken. The same applies for the inflammatory stage of ankylosing spondylitis. In the unlikely event of a patient with this disorder developing a disc lesion, manipulation is not at all safe, especially in the cervical spine, where luxations, fractures and cord compression have been described.79
Neurological deficit and spinal cord compression
Segmental neurological deficit is characterized by disturbance of either motor function, with impaired reflexes and/or muscular weakness, or sensory function, with diminished sensibility. The two may be combined. Segmentally referred pins and needles due to compression of the sensory fibres of a nerve are not regarded as neurological deficit and are therefore not a contraindication. In neurological deficit, manipulation is usually without value because deficit suggests a large protrusion that cannot be reduced. This opinion is not universally supported,80,81 and some still manipulate when minor neurological signs are present. However, in all instances where progressive neurological deficit is present, manipulation must not be done.
Hypermobility
In several schools of thought on manipulation, too much emphasis is placed on hypermobility. Although it is true that special attention must be given to hypermobility in the cervical spine, it is not important elsewhere. A hypermobile joint may move further than an ordinary joint, but once extreme range is reached it stops in exactly the same way as does an ordinary joint. More often the disc fragment itself is hypermobile, which may lead to frequent recurrences. This circumstance does not contraindicate manipulation but calls for extra measures to achieve stabilization, for example by infiltration with ligament sclerosant (see Cyriax:3 p. 38).
For the cervical spine a history of frequent disc problems, alternating from one side to another, may be suggestive of hypermobility. When doubt exists the following tests may be useful: spinal flexion with putting the palms flat on the floor with knees straight, passive apposition of the thumb to the flexion aspect of the forearm, passive hyperextension of the fingers parallel to the external surface of the forearm and hyperextension of the elbow and/or of the knee of 10° or more. If one or several of these are positive hypermobility is likely.82 Also, when the end-feel on passive rotation, extension or on preparation for a straight-pull manipulation is too elastic, further manipulation must cease.
Spinal manipulation under anaesthesia
Spinal manipulation should never be done in an unconscious patient. First, anaesthesia is unnecessary. Second, the final warning of potential danger offered by increased pain or abnormal end-feel on taking up the slack is completely lost, as is clinical assessment after each manœuvre. Consequently, complications are more frequent after manipulation under anaesthesia.83
Evaluation of the effectiveness of spinal manipulation
Although several studies, mainly done on the lumbar spine, support the view that many patients benefit from spinal manipulation,39–41,84–87 agreement on the effectiveness and the role of manipulation in spinal disorders is still lacking. Reports from clinical trials are not always clear and the effects of manipulation are often difficult to interpret88 because of a small number of patients and their selection by symptoms rather than diagnosis. To make trials scientifically valuable a precise definition of manipulation is necessary – a record of which types of technique have been used and for what type of disorder and its duration. It should also be said that a double-blind randomized trial on spinal manipulation is not possible because of the absence of a placebo and the obvious knowledge by the patient and operator of what is being done.
Sims-Williams published a clinical trial on 94 patients with non-specific lumbar pain, who took part in a trial in which placebo physiotherapy was compared to Maitland mobilization and manipulation. Studies mainly showed that manipulation hastened improvement chiefly in those patients whose severity and duration of symptoms did not require specialist referral.80,89
Bergquist-Ullman and Larsson,90 Coxhead et al81 and Farrell and Twoney39 found a significantly shorter duration of complaints in patients receiving manipulation.
Chrisman et al91 stated that half of those suffering from sciatica showed clinical improvement after manipulation, but the improvement could not be objectively confirmed by myelography.
Hadler et al86 compared the results of spinal mobilization to high-velocity thrust manipulation in patients with acute, uncomplicated low back pain and tried to exclude all elements of chronicity or compensation insurance. Patients treated by manipulation improved to a significantly greater degree and more rapidly than those treated by mobilization.
In one study, in which rotational manipulation was compared with simulated short-wave diathermy, those who received the former fared better immediately after the session.92 However, when pain relief was compared 7 days after treatment there was no significant difference between the two groups.
In another study, 24 patients with complaints of less than 3 weeks’ duration were followed. It showed that 92% of those treated by rotational manipulation were cured in less than 2 weeks.93 Of those who received diathermy, only 25% got better in the same period of time.
A further trial in acute disc herniation compared conventional physiotherapy with manipulation and showed that the manipulated group scored significantly better.94 All manipulated patients were able to return to work, whereas only 26% of the physiotherapy group could do so.
In a randomized clinical trial Koes et al compared the effectiveness of manipulative therapy, physiotherapy, treatment by the general practitioner and placebo therapy in 256 patients with non-specific back and neck complaints of at least 6 weeks’ duration. They concluded that manipulative therapy showed a faster and greater improvement in physical functioning compared to the other three therapies.95,96
Controlled studies performed by Mathews et al clearly demonstrated that manipulation treatment for low back pain scored significantly higher in the subgroup with limited straight leg raising.97,98
Complications of spinal manipulation
General considerations
Manipulation is, as with anything in medicine, not without danger and it must be admitted that even in experienced hands accidents may happen. Therefore manipulative treatment must never be undertaken recklessly, or on a ‘hit or miss’ basis.3 Although it is probable that more accidents have occurred than have been reported, the risks must not be overstressed.40,99 In 30 years of clinical practice Kirkaldy-Willis29 (his p. 293) did not have one patient who was made worse by a manipulation. Dvorak and Orelli estimated that in 1 out of 400 000 manipulations severe neurological damage results, and in 1 out of 40 000 slight neurological signs appear.100 It should not be forgotten that traditional treatment with non-steroidal anti-inflammatory drugs is also not without complications, in that they may give rise to severe gastrointestinal problems (mucosal bleeding, or reactivation of previous ulcers or initiation of new ones), haemolytic anaemia, leukopenia, thrombocytopenia and even fatal agranulocytosis, salt and water retention, albuminuria, nephritis, acute renal insufficiency, or to allergic reactions in all degrees of severity. No matter what treatment is given there will always be an inherent risk, but this should be reduced to a minimum by taking all necessary precautions.
Risks in relation to level
The risks involved in manipulation differ at the cervical, thoracic and lumbar levels.
Cervical level
Serious neurological complications have been reported after manipulation of the cervical spine. The techniques that are blamed to cause most of the injuries are hyperextension manœuvres accompanied by excessive rotation.45,102,103
During a recent inquiry over a period of 2 years among 468 Californian neurologists, 55 strokes following osteopathic cervical manipulation were surveyed. Most of the patients continued to have persistent neurological deficits 3 months after the onset and about one-half were marked or severe. Nearly all of the strokes involved the posterior circulation and almost one-half were angiographically proven.109 A Danish survey reported the incidence of cerebrovascular incidents (CVI) after chiropractic manipulation to be about 1 for every 120 000 cervical treatment sessions, manipulation to the upper neck being about four times more commonly associated with CVI than treatment of the lower neck.110
Neurological complications are mainly the result of a dissection of the vertebral artery104–108. Vertebral artery dissection (VAD) is an uncommon vascular wall condition that typically involves a tear at some point in the artery’s lining and the formation of an intimal flap (see Chapter 9). The latter triggers off an arterial narrowing or even a complete obstruction of the lumen.111,101 Although the pathophysiology of a dissecting vertebral artery is well understood, the underlying cause of intimal tears remains uncertain. Most experts link VAD to traumas of varying degrees of severity and maintain that because tearing occurs, previous trauma was necessarily involved. An article reviewing 606 cases of VAD reported that 371 (61%) were spontaneous. The remaining 39% were associated with trivial or other trauma, which included manipulation in 9% of the total cases.112 However, VADs more commonly occur after very minor trauma, and even everyday activities such as reversing a vehicle, coughing, vomiting, unusual sleeping positions or having one’s hair washed at a beauty salon113. For that reason, evidence is mounting that the association between spinal manipulation and stroke is coincidental rather than causal and reflects the natural history of the disorder114.
Lumbar level
The main complication is compression of the cauda equina because of a massive posterior sequestration of a lumbar disc.115 Compression of the cauda equina complicating lumbar manipulations without anaesthesia is extremely rare, when it is considered that in the US in 1975 about 124 million office visits to chiropractors took place. Between 1911 and 1992 only 13 cases were recorded.116 This potential complication should never be taken as contraindication to manipulation. However, anyone who manipulates must be able to recognize the syndrome immediately, so that no time is lost before surgical decompression is performed.
Measures to prevent complications
Although complications may occur and cannot be totally excluded by any means, each manipulator should try to reduce the eventuality to the lowest possible degree. It would be wrong to condemn the manipulator simply because a mishap or a complication occurred. If this was done it would mean that, instead of getting on with his work, the practitioner would forever be ‘looking over his shoulder’. It is not possible to arm oneself against unpredictable events. Even if they do occur occasionally, this argument should not be used to condemn manipulation.116
Clinical examination
Manipulation should never be used simply because ‘no contra-indication has been discovered, no one can think what else to try, and a friend was recently relieved by this means’ (Cyriax:117 p. 31). If the diagnosis is unclear or if too many inconsistencies are found, manipulation should be avoided. Once again it should be stressed that manipulation follows only if the diagnosis of a discodural or discoradicular interaction has been established. For safety, the following must be added: ‘If the diagnosis is established but it is uncertain if manipulation will work, then try. If the diagnosis is uncertain and it is unclear whether or not manipulation is safe, do not try.’ (Cyriax3).
Radiographic appearances
Although the diagnosis of tumours of the lumbar spine is largely dependent on radiography examinations, it must be remembered that 30% of the osseous mass of a bone must be destroyed before this type of lesion becomes radiologically evident.118 Therefore radiographs do not reveal early disease, and too much reliance on negative radiographic appearances can give rise to a false feeling of security. Radiographs that show no evidence of bone disease should not be taken to indicate that manipulation is safe (Cyriax:64 p. 292). A decision to manipulate because the radiograph is normal carries a high risk of worsening the patient’s condition and may even lead to disaster. The diagnosis of lesions in bone in the early stage is mainly dependent on history and clinical examination. Special attention must be paid to ‘warning signs’. In several disorders, such as early invasion of bone by a secondary neoplasm, the clinical signs may precede the radiographic findings. In doubtful cases, when routine radiography fails to support the clinical impression, a radioisotope scan must be obtained.
Appropriate technique
Manipulative techniques contain important safeguards against possible accidents. This is chiefly so for the cervical spine, in which dangerous techniques such as extension in combination with rotation should never be used.36,119,120 Those with special interest in musculoskeletal disorders should not only read textbooks but must be prepared to take courses in order to learn the necessary theoretical and practical skills before undertaking manipulation.
Once a manipulation has started, the operator must always concentrate on the type of tissue resistance (end-feel) while taking up the slack just before the final thrust is given. If the end-feel is abnormal, he must stop immediately and must not manipulate. To push through muscle spasm protecting a joint should never be attempted.117
To prevent compression of the spinal cord all manipulations must he performed under traction.
Active movements
The effects of immobilization on skeletal muscle, tendon, ligament, joint capsule and articular cartilage are dramatic and have been described thoroughly in Chapter 3. Physical activity is also the primary stimulus for the repair of musculoskeletal tissues. Therefore, most therapeutic modalities that are advocated in this book are in conjunction with movement. Active movements are defined as those undertaken by the patient via muscular contraction. In orthopaedic medicine they are not so often used as a sole therapy; their main role is in combination with other therapeutic techniques. However, there are a few situations (both therapeutic and prophylactic) where active movements play a particular role.
Simple active movements to gain or preserve normal range in a joint
Treatment of sprains is essentially treatment with movement (see p. 48). Although the first measure is friction, passive and active movements within the limits of pain to maintain normal gliding of the ligament over adjacent bones should be encouraged. When the lower limb is involved, the patient should be instructed to walk as normally as possible but without provoking pain.
Ligamentous adhesions that have developed as the consequence of a chronic sprain at ankle or knee need to be ruptured manually: the joint is forced through its normal range of movement by a high-velocity, short-amplitude thrust manipulation (see p. 12). After the manipulation and in order to retain the mobility achieved, the patient should repeat the same movement actively and on a daily basis. After rupturing of adhesions under anaesthesia, active movements in addition to passive ones are also necessary to maintain the range that has been regained. They should be performed several times a day.
Isotonic contractions
In orthopaedic medicine, isotonic contractions are performed in the following situations:
• In minor muscular tears after the lesion has been prepared by gentle transverse friction (see p. 4). The contractions are carried out with the muscle in a position of maximal relaxation and with minimal resistance so that no tension falls on the healing breach. They begin as soon as possible after the injury and are preceded by an infiltration with local anaesthesia and by transverse friction. The idea is to promote movement between adjacent muscular fibres to prevent abnormal formation of adhesions because these can disturb the normal increase in breadth on contraction.
• To strengthen weakened muscles as in arthritis or after local or generalized immobilization. If passive movements are limited, say by the arthritis, the isotonic exercises should be performed within the painless range to avoid increase of synovial inflammation.
• To strengthen muscles so they can protect joints or inert structures from being painfully overstretched. One example is the strengthening exercises of the short plantiflexor muscles and the lumbricals of the foot in the treatment of splay foot and chronic metatarsalgia. Strong muscles that contract properly at each step will take most of the body weight and relieve the metatarsal heads.
Eccentric contractions
Eccentric (lengthening) actions are characterized by elongation of the muscle during active contraction.122 Over the last fifteen years, eccentric exercises have been promoted as treatment strategies for tendinopathies and muscle strains, especially for the lower limb (quadriceps and Achilles tendinopathy). Greater forces can be produced during eccentric contraction than during concentric (shortening) actions,123 which leads to positive changes in tissue structure and mechanical properties. One study found that Type I collagen synthesis increased after eccentric training in a group of twelve soccer players with unilateral Achilles tendinosis, offering a possible explanation for the mechanism of tendon healing.124 Another study described a decrease in tendon thickness and normalized tendon structure measured by ultrasound in a group of subjects with chronic Achilles tendinosis who were trained using an eccentric training protocol.125 Systematic review of the literature revealed that eccentric exercise may reduce pain and improve strength in subjects with lower extremity tendinosis,126,127 but whether it is better than other forms of rehabilitation has yet to be determined.
Coordination exercises
Proprioception is a specialized sensory modality that gives information about extremity position and direction of movement: stretch-sensitive mechanoreceptors within skin, capsular ligaments and tendons (see Ch. 3) are activated by tension, thus producing a muscular contraction to protect these structures at the extreme of motion.128 This type of afferent sensory feedback is extremely important in mediating muscular control over joints and thus preventing them from overstretch and (sub)luxation.129
Numerous authors have recommended the training of proprioceptive skills and proper muscular coordination to re-establish the reactive neuromuscular control abilities in the joints at risk and to create a functional joint stability.130–134 Several techniques exist, from the see-saw block or tilting board in the treatment of functional instability of the ankle to the use of dual channel electromyography biofeedback systems in the treatment of patellofemoral dysfunction135 and glenohumeral instability.136 However, most functional training techniques used to re-establish the proprioceptive skills make use of eccentric training.137 Eccentric activation refers to the situation in which the muscle–tendon unit is lengthened while active. Small weights and multiple repetitions of the movements are used.
Proprioceptive neuromuscular facilitation (PNF) techniques can also be used to gain or improve neuromuscular stability at a joint. PNF techniques may be of value in the prophylaxis of recurrent periarticular shoulder lesions. PNF may be defined as a method promoting or hastening the neuromuscular mechanism through stimulation of the proprioceptors. Hence, PNF refers to the improvement of flexibility through stimulation of the nerves and muscles internally. The technique involves the use of the principles of reciprocal innervation and the stretch reflex: as a muscle is passively or actively stretched, it is brought to a point of limitation before pain develops. This is the point at which the proprioceptive organs send a message to the central nervous system to terminate the movement before further elongation occurs. At this point the muscles being stretched (antagonist) are contracted for a few seconds at an intensity of 50% of maximum. This contraction allows for the inhibition of the muscle spindles and Golgi tendon organs and a subsequent initiation of the stretch reflex of the stretch receptors. After releasing the contraction, the muscle is stretched to a new point of limitation and held for another few seconds. The interested reader is referred to Alter’s Science of Stretching,138 that offers over eight PNF techniques and exercises.
Injection and infiltration
General principles
To obtain maximal benefit with minimal side effects the following general rules must be observed.
Exact diagnosis
Any treatment must reach the lesion. Infiltrations, like deep friction, need a diagnosis accurate within a millimetre or two and must be directed to the precise site of the lesion. The steroids used in orthopaedic medicine are all suspensions of insoluble particles, so their action is mainly confined to the place where they are administered. An exact preliminary diagnosis must be made, together with proper localization of the lesion.139
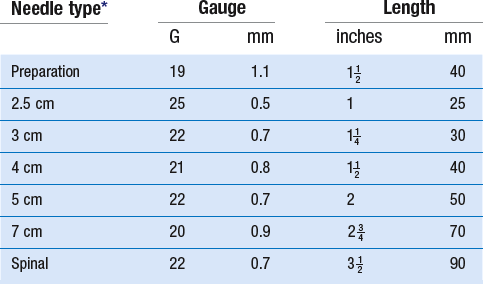
Equipment
The main characteristics of the needle types referred to in this book are given in Table 5.3.
Aseptic care
• Skin antisepsis at the site of insertion
• Disinfecting the rubber septum with alcohol prior to piercing it
• Using a new sterile syringe and sterile needle to draw up the fluid while preventing contact between the needle and the hands
• Removing the needle and using a fresh one for the injection
• Using a no-touch-technique: neither the tip of the needle, nor the skin at the site of insertion should be touched after skin antisepsis
• Using gloves? Gloves can only be used if an assistant handles the non-sterile packages and vials and prepares the syringes. In our opinion, the use of gloves does not add to aseptic safety, if the rules mentioned above are strictly followed.
Technique of infiltration
Dynamic infiltration
Conewise infiltration
This is the usual technique for a lesion of a muscle belly. The limb is brought into such a position that the muscle is well relaxed. The tender part is pinched between the thumb and fingers and the needle is inserted obliquely in between them until its tip passes beyond the farthest edge of the lesion. Some of the product is now administered while the needle is withdrawn until the tip is at a point just beyond the nearer border of the lesion. It is then reinserted at a slightly different angle and more product is infiltrated while the tip is again withdrawn (Fig. 5.7). This is repeated several times until the entire lesion has received some of the product. During the whole procedure, the fingers that hold the lesion verify and control the infiltration.
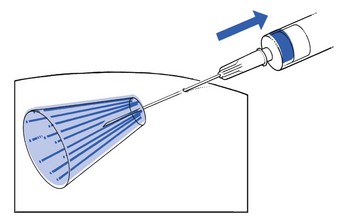
Fig 5.7 Conewise infiltration.
Fanwise infiltration
This technique is similar to conewise infiltration but is two-dimensional. It is used in subacromial bursitis. The needle is directed towards the centre of the deep part of the subdeltoid bursa and to its full length. By a series of partial withdrawals and reinsertions in a horizontal plane, to the left and to the right from the centre (Fig. 5.8), the full amount of product is applied during withdrawal.
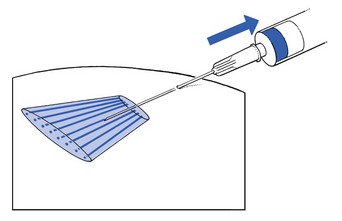
Fig 5.8 Fanwise infiltration.
Cylindrical infiltration
A cylindrical infiltration is used to place the agent along the surface of a tendinous body. The tendon is first stretched to provide a stiff flat surface. The needle is tangentially inserted along the tendon between the tendon and its sheath, until the tip reaches the far edge of the lesion. During partial withdrawal as the needle traverses the surface of the tendon, constant pressure on the plunger maintains flow of the suspension. The needle is then reinserted parallel to its first position but 2 mm to one or the other side and the manœuvre repeated (Fig. 5.9). This is repeated four or five times until the full amount has been given.
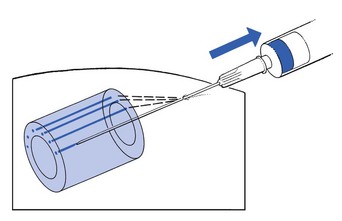
Fig 5.9 Cylindrical infiltration.
Static infiltration
This technique is mainly used to put a small amount of fluid into a well-delineated area. It is indicated for tendinous insertions and ligamentous attachments to bone. These offer considerable resistance to depression of the plunger. Hence the smallest syringe must be used to provide enough purchase to force the product into the structure. When the tip of the needle lies at the exact site, a typical counterpressure is felt during insertion, just before its point hits the bone. Now a few droplets are injected with the tip of the needle in bony contact. The needle is then five to ten times partly withdrawn and inserted at slightly different angles and depths (Fig. 5.10) until the full amount has been administered and the whole lesion has been treated. The technique is sometimes referred to as peppering. During the entire infiltration a typical resistance is felt, much more marked than during infiltration of a muscle belly or a bursa, where resistance is minimal.
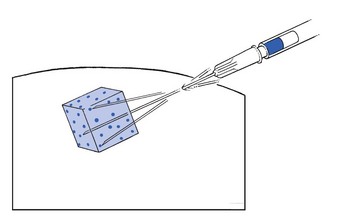
Fig 5.10 Static infiltration.
Local anaesthetics
Types of local anaesthetic
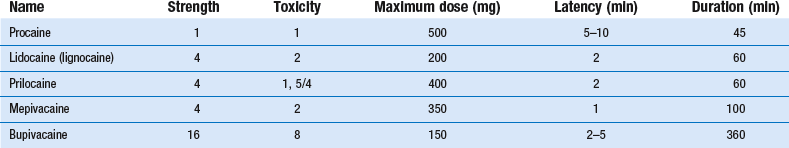
Two major types of local anaesthetic are available: procaine and those belonging to the amide group (e.g. bupivacaine, lidocaine (lignocaine)) (Table 5.4).
Procaine
Procaine is an ester of para-aminobenzoic acid and was first synthesized in 1904 by Einhorn. Until 1943 it was the only anaesthetic available.140 It is quickly and locally metabolized by an esterase, giving rise to the acid itself, which may act as an allergen. Its effect begins after 5–10 minutes and lasts approximately 45 minutes. The maximum dose used is 250 mg, which corresponds to 50 ml of a 0.5% concentration.
Psychogenic side effects
These minor side effects are mainly caused by somatosympathetic reactions on pain and fear and are not related to the drug as such. Nevertheless the symptoms may be quite similar to those of real toxic reactions: pallor, cold sweating, dizziness, nausea, yawnings, palpitations and vasovagal collapse with syncope all may be present.142 They should be taken seriously because if the patient is not placed supine quickly, cerebral hypoxia may follow, with unconsciousness, tremor and convulsions.
Toxic reactions
These are dose-dependent side effects related to the amount of product that reaches the blood circulation.143 They may be the result of unintentional intravascular injection, absolute overdose, swift absorption or delayed elimination of the drug.144
Types of reaction
Effects on the central nervous system
Although local anaesthetics may provoke stimulation or depression of both cortex and medulla, stimulation is the more frequent but is less severe than depression. Normally the depression period is preceded by a stimulation stage, but it may come on at once without a prior stage of excitement.145
Some stimulation of the cerebral cortex and the upper centres may sometimes occur even with a low dose. It is characterized by anxiety, excitement, logorrhoea, hypertension, headache, dizziness, tinnitus, diminished hearing, disturbed vision, metallic taste, muscular fasciculations around the mouth and tremor. None of these symptoms is severe as such, but they are all signs of the presence of a toxic reaction that could lead to cardiovascular collapse. Further stimulation may be followed by convulsions, which indicate that severe cortical stimulation is present and may progress to postconvulsive depression.145 Stimulation of the emetic centre causes nausea and vomiting. Stimulation of the cardiovascular centre in the medulla may cause tachycardia and hypertension; respiratory stimulation is characterized by an increased depth and frequency of breathing.
Effects on the cardiovascular system
Local anaesthetics can alter the blood pressure in different ways. Stimulation of the CNS leads to hypertension, depression to hypotension. Hypotension may be intensified via a direct vasodilatory effect on the blood vessels and by direct myocardial depression. Furthermore, in lumbar epidural injection, hypotension may be due to blockade of the sympathetic nerves.146
Clinical appearance
Toxic side effects may clinically appear in two ways:147
• A delayed reaction may occur within 5–30 minutes after the infiltration. This is the most frequent reaction and is due to slow absorption until a toxic level is reached. It usually first gives rise to stimulation of the cortex before respiratory symptoms and cardiovascular collapse occur. For this reason the patient should always remain under supervision during the first half hour following an injection.
• An immediate reaction may occur within seconds to minutes of the administration, with all toxic reactions coming on at once. It is usually the result of intravascular injection or of swift absorption. Collapse may occur very quickly and death may follow rapidly if resuscitation is not begun at once.
Treatment
• Fear or anxiety attacks are best treated by intravenous diazepam (5–10 mg).
• Cerebral signs – tremor and convulsions – require immediate administration of 100% oxygen via a mask. Small intravenous doses (5–10 mg) of diazepam may be given. Barbiturates and short-acting muscular relaxants should only be used by the experienced and should always be preceded by the administration of oxygen.144
• Hypotension: the patient is put into the Trendelenburg position. If this is not sufficient, administration of vasoactive drugs such as dopamine or noradrenaline (norepinephrine) may be required.143 In circulatory depression, intravenous fluid must also be given. Bradycardia can be treated by atropine.
• Cardiac arrest: oxygen and external cardiac massage are given.
• Respiratory depression is treated by oxygen and artificial respiration (intubation) (see Box 5.5).
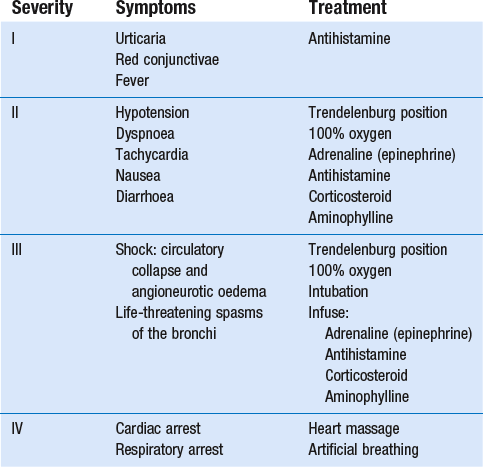
Allergic (anaphylactic) reactions
Although allergic reactions are frequently mentioned in relation to local anaesthetics they are in fact rare.147 According to Cyriax, anaphylactic reactions occur in 1/50 000 procaine infiltrations, though they are more frequently encountered with procaine than with the amides.144,146,148 Since an anaphylactic reaction may be very dramatic, with a mortality rate of about 3.4%, one must always be aware that it is possible.149 Before local anaesthetics are administered the patient must always be asked for evidence of an allergic constitution. If a patient claims to be allergic to local anaesthetics, a careful and detailed history must be taken because 99 out of 100 reactions are due to toxic or psychogenic side effects and not to an allergy as such.147 An intradermal test with a small amount of agent can be useful but is not 100% reliable.147
Treatment
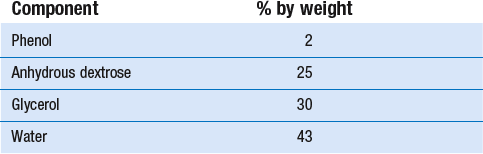
Treatment is different for immediate and delayed allergic reactions. The treatment is outlined in Tables 5.5 and 5.6.
Table 5.6
Medication used in anaphylactic reactions
| Drug | Dose | Notes |
| Adrenaline (epinephrine) | ||
| Adults | ||
| Normal blood pressure | 1/1000, 0.3–0.5 ml s.c. | To be repeated every 20 min |
| Severe hypotension | 1/10 000, 3–5 ml i.v. | 1 ml per shot |
| Children | 1/1000, 0.01–0.03 ml/kg s.c. | |
| Antihistamine (clemastine) | 2 mg i.m./i.v. | Every 6 h for up to 24 h |
| Corticosteroids (dexamethasone) | 4–8 mg i.v. | Every 6 h for up to 24 h |
| Aminophylline | ||
| Adults, initial dose | 240 mg i.v. | |
| Children | ||
| Initial dose | 5 mg/kg i.v./i.m. | |
| Follow-up dose | 0.4 mg/kg/h i.v. |
Immediate reaction
Even when only minor signs of anaphylactic reaction are present 0.3–0.5 ml of adrenaline (epinephrine) 1/1000 (0.3–0.5 mg) is immediately administered by the subcutaneous route to provoke vasoconstriction, bronchiolar dilatation and resorption of oedema. Since adrenaline (epinephrine) is broken down quickly, it should be repeated every 20 minutes. Subcutaneous administration of adrenaline can only be done if the general circulation is intact. When blood pressure is too low it must be carefully administered intravenously. In this event 3–5 ml of adrenaline (epinephrine) 1/10 000 must be administered in repeated shots of 1 ml (0.1 mg) until effect has been attained.150 Small repeated shots are necessary to avoid ventricular fibrillation. Some also advise inhalation of a 1/10 000 adrenaline (epinephrine) solution via aerosol in case of laryngeal oedema. Steroids inhibit allergic reactions but act too slowly in this situation. Oxygen should also be given but may be of little value if the airway is severely obstructed. In the latter case, aminophylline should also be injected.
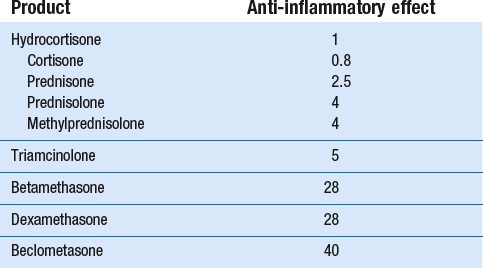
Corticosteroids
The adrenal corticosteroids are classified into two groups: mineralocorticoids such as aldosterone, with sodium-retaining activity, and glucocorticoids, which influence the intermediary metabolism (nitrogen catabolism, increased glucogenesis) and have a strong anti-inflammatory and anti-allergic effect. The ability to suppress inflammation has made the glucocorticoids very useful but also potentially harmful. Administered in high doses, they may cause Cushing’s syndrome.151
All corticosteroids used in orthopaedic medicine are glucocorticoids. The first was hydrocortisone, extracted from the adrenal cortex by Kendall in 1936, and first intra-articularly injected by Thorn in 1950.152 Since then many other steroids have been synthesized. Efforts to increase the anti-inflammatory effect and to diminish the influence on metabolism have remained largely unsuccessful so far. Thus, unnecessary use should be avoided.
The ideal steroid should meet the following criteria: little discomfort to the patient during and after injection, a low level of absorption into the systemic circulation (if absorption does occur, it should be slow), together with a prolonged local effect without general and local side effects.153 Some preparations are formulated specifically for local use and are available as a crystalline suspension. The less water soluble they are, the less they are absorbed into the general circulation. As a consequence they have a more prolonged local effect and fewer general side effects. Intrasynovial administration has the advantage of a maximal local benefit with minimum systemic side effect.154
The agent we use most often is triamcinolone acetonide, in a concentration of 10 mg/ml. Throughout this book, this is the product and concentration intended, unless indicated otherwise in the text. It has a mean duration of activity of about 14 days, whereas triamcinolone hexacetonide has more prolonged activity.155 Normal doses used are 5 mg for small joints, 20 mg for medium-sized joints and 50 mg for the hip and knee.
Therapists who prefer another type of corticosteroid should always administer the dose equivalent to the one indicated in the text (see Table 5.7).
Effects of local corticosteroids
Corticosteroid injected locally has a local anti-inflammatory effect due to stabilization of the lysosomal membrane with decreased liberation of cytotoxic enzymes. Steroids also impair the proliferation of fibroblasts and decrease the rate of production of mature collagen. They decrease plasma fibrinogen as well and have an increased fibrinolytic activity.156 Furthermore, corticosteroids reduce oedema formation and the escape of plasma protein across the capillary membrane, and diminish the number of leukocytes in exudate at an inflammatory site. All these effects lead to reduction of pain and fibrosis.157–161
Indications for local corticosteroids
Joints
Beneficial effects occur in traumatic arthritis, monoarticular steroid-sensitive arthritis, rheumatoid arthritis, crystal-induced arthritis (gout and pseudogout), ankylosing spondylitis, lupus erythematosus and psoriasis.153 Steroids are ineffective in Reiter’s disease (Cyriax:3 p. 52).
Improvement is subjectively felt by the patient in that pain and stiffness diminishes, and objectively shown by a decrease of local heat and effusion together with improved function. Patients should be warned against overactivity at weight-bearing joints for the first days after injection to avoid further destruction of cartilage.162 Moreover, the efficacy of an injection is greater with relative rest.
In arthrosis, lasting improvement is not to be expected.163 Some authors even suggest, although this has never been scientifically proven, that it may accelerate the degenerative process.162 If synovitis complicates arthrosis, intra-articular injection may well be beneficial.
Tendons
To avoid rupture, infiltration should be at the tenoperiosteal insertion or between tendon and tendon sheath, never into the body of the tendon.162,164–167 Ruptures have been reported mainly after intratendinous infiltration with agents of high anti-inflammatory effect or at too high a concentration or when too frequently administered. When the rules are respected as set out in this chapter, there should be no danger of rupture.
Ligaments
In sprain of the cruciate ligaments of the knee, steroid infiltration is the only possible treatment, no matter what the stage of inflammation. Steroid infiltration is also an important part of the treatment in sprains of the radial and ulnar collateral ligaments of the wrist and in plantar fasciitis.168
Local side effects
Unwanted side effects of local corticosteroids are minimal compared with those of even low doses of oral steroids.153 They are traditionally divided into local and general side effects.
Musculoskeletal side effects
There are a number of musculoskeletal side effects of local corticosteroid injection.
Iatrogenic infectious arthritis
This complication is the most feared although it is seldom encountered. The incidence varies from author to author: it follows between 1/1000 and 1/40 000 injections.153,171 The usual organism is Staphylococcus aureus; less often, Gram-negative organisms are involved.172 The condition should not be regarded as a real side effect caused by the steroid but is due rather to inadequacy of aseptic care or contamination, chiefly occurring during preparation of the syringe. Patients who suffer from diabetes, or who are receiving oral steroids or are immunosuppressed (leukaemia, AIDS, drug abuse) are more vulnerable.173 Suppurative arthritis may often lead to therapeutic difficulties, and death may follow.174
Destruction of joint cartilage and evolution of steroid arthropathy
It has been suggested that intra-articular steroids may hasten the process of arthrosis by a deleterious effect on cartilage, leading to changes that closely resemble a Charcot-like neuroarthropathy. Steroid depresses the synthesis of collagen and proteoglycans, which may result in a loss of stiffness of the cartilage. In non-weight-bearing joints this has little or no effect. In weight-bearing joints it may result in fissure formation at the surface of the cartilage and cystic degeneration in the middle zone.175–178 However, rapid progression to degeneration has not been proved with certainty.171,179 Cases have been reported of multiple intra-articular injections in some joints not leading to any abnormalities on later radiography.180,181 Often effects of local steroid cannot be differentiated from those caused by general administration of the product,182 prompting the question whether it is a local or general effect. Because it is difficult to differentiate the possible destructive effects of the steroids from the natural progression of the osteoarthrosis, even though the risk may appear small, it is a good habit to avoid frequent injections. Moreover, injection into cartilage should never be done. When too much counterpressure on the plunger is present, the tip of the needle must be replaced. It is also wise to rest weight-bearing joints for 24–48 hours after an injection.139
Rupture of ligament or tendon
Tendon ruptures have been described after one or multiple infiltrations.166,183,184 Infiltration of steroids into acutely injured ligaments in the rat significantly impaired the healing process relative to a non-injected ligament at 10 days and at 3 weeks after injury.185 However, after 6 weeks the tensile strength (the ultimate stress) of the ligaments that had been injected with the steroids returned to a value that was equal to that of the controls that had not received an injection.186 Although other studies have not confirmed these findings,187,188,189 infiltration into the tendon body should never be done. In tenosynovitis, steroid can safely be infiltrated between tendon and tendon sheath and at the tenoperiosteal insertion, although multiple repetitive infiltrations must be avoided.
Neurovascular complications
Direct intrafascicular injection of steroid in peripheral nerves may provoke permanent damage, whereas extrafascicular injection does not appear to be harmful.190 The mechanism of injury is multifactorial and can be related to direct trauma with the needle, to ischaemia and to a neurotoxic effect of the steroid or of the buffer agents and additives such as polyethylene glycol and benzyl alcohol. The first features are severe radiating pain and numbness or paraesthesia in the sensory territory of the nerve, together with motor deficit. The pain usually responds poorly to narcotics and may persist for many years.191 As to the steroid itself, triamcinolone hexacetonide and hydrocortisone are most hazardous and dexamethasone causes minimal damage, whereas triamcinolone acetonide is intermediate.190,192
General side effects
Although injected intra-articularly or into the soft tissues, corticosteroids do enter the circulation. The causes are leakage and absorption. Therefore general side effects depend on the administered dose, the frequency of injections, the number of joints injected and the aqueous solubility of the agent. The greater the aqueous solubility, the higher the absorption rate. Less soluble microcrystalline suspensions remain within the joint for longer. Administration of a given dose equally divided between two joints produces more general side effects than if the same amount was injected into a single joint – the result of a larger absorptive surface.172
The majority of the more severe systemic effects can be avoided if no more than two joints are treated at the same time, using a maximum of 40 mg triamcinolone and allowing an interval of 1 month between two injections.193 If treatments are performed as recommended in this book general side effects are extremely rare.
Endocrinological side effects
There are five categories of potential endocrinological side effects.
Disturbance of hormonal equilibrium
• Hyperglycaemia: glucocorticoids have an important influence on the intermediary metabolism. They increase circulatory glucose via stimulation of gluconeogenesis and decrease the intracellular use of glucose. Therefore it is wise to advise diabetic patients to check their blood sugar more closely for the first few days after the use of steroid.
• Suppression of the adrenal cortex via depression of plasma cortisol levels: small doses of steroid may provoke some suppression of the adrenal cortex.194 This seems to occur not only when steroids are administered orally but also after intra-articular injections.195 Prolonged administration renders the adrenals atrophic and provokes suprarenal insufficiency with symptoms such as hypotension, anorexia, fever and generalized joint or muscular pain.
Iatrogenic Cushing’s syndrome
The full syndrome with weight gain, depression, insomnia, amenorrhoea, diminished libido, thinned skin, muscular weakness, polyuria and polydypsia is seldom encountered after local use of steroids.180 Occasionally facial hirsutism and acne may be seen.
Musculoskeletal side effects
Immunological side effects
An allergic reaction to steroids is not expected because they all have immunosuppressive and anti-inflammatory activity. However, a number of well-documented allergic anaphylactic (type I) reactions to corticosteroid medications have been reported.199 Recent reports have warned of potential (though rare) anaphylactic reactions after intra-articular or intralesional injection of triamcinolone acetonide.200–202
One recent study indicates that the triamcinolone acetonide component responsible for the patient’s reaction is the suspending agent carboxymethylcellulose.203 It is therefore suggested that care be taken and component testing eventually considered when patients experience allergic-type reactions to drugs.
Miscellaneous side effects
Central nervous system, gastrointestinal and ophthalmological side effects have been reported:
• Prolonged use of steroids may provoke changes in personality and mood.
• In patients who have previously suffered from peptic ulcer and pancreatitis, steroids should he cautiously used.
• After long-term use of steroids some patients may complain of worsening of vision. This may be due to glaucoma or cataracts.204
Indications for and contraindications to local corticosteroids
The indications for corticosteroid injection are given in Box 5.6. Contraindications may be divided into absolute and relative (Box 5.7).
Viscosupplementation
Over the past 2 decades, the use of intra-articular viscosupplementation in the non-operative management of patients with osteoarthritis has become quite popular. Viscosupplementation refers to the concept of synovial fluid replacement with intra-articular injections of hyaluronic acid (HA) for the relief of pain associated with osteoarthritis.205 HA is a high molecular weight polysaccharide and is an important component of synovial fluid and extracellular matrix of articular cartilage. It contributes to the elasticity and viscosity of synovial fluid. HA acts as a fluid shock absorber and it helps to maintain the structural and functional characteristics of the cartilage matrix.206,207 It also inhibits the formation and release of prostaglandins, induces proteoglycan aggregation and synthesis, and modulates the inflammatory response.208 Any degradation of HA is therefore associated with increased vulnerability to articular cartilage damage. Treatment with HA is indicated for patients who are functionally limited due to osteoarthritic pain and who have failed to respond adequately to standard treatment options and wish to postpone or avoid surgery. Viscosupplementation is currently accepted as a useful therapeutic modality in treating patients with osteoarthritis of the knee or hip,209,210 with beneficial effects on pain, function and patient global assessment.211 Recently, promising results for viscosupplementation in grade I and II ankle osteoarthritis have also been published.212,213
Sclerosing agents
Product
The original solution, used by Hackett and consisting of zinc sulfate and carbolic acid, provoked painful reactions and was not totally risk free.214 The mixture used nowadays is the one chosen by Ongley which has a safe reputation as it was regularly used to sclerose varicose veins. It is formulated as described in Table 5.8 and is mentioned under the name P2G.215
Mode of action
Liu et al216 and Maynard et al217 studied the histologic effect of injections with a sclerosant. Biopsies of infiltrated medial collateral ligaments of the knee of the rabbit showed not only increase in ligamentous mass and strength but also a normal alignment of the fibres. In other words, the newly produced connective tissue did not have the chaotic appearance of scar but appeared much the same as normal tissues, except that they were thicker, stronger, and contained fibres of varying thickness.
Klein et al218 performed biopsies of posterior sacroiliac ligaments in three patients with chronic low back pain both before and after prolotherapy injections. After six injections at intervals of a week they found an increase in the average ligament diameter measured by electron microscopy from 0.055 micrometres to 0.087 micrometres. Light microscopy showed an increase in collagen-producing fibroblasts. The ligament orientation was organized and linear, as in normal ligaments.
In addition to the effects on fibrous tissue, phenol also has a neurolytic effect. When injected in or around the medial branches of the posterior ramus, it provokes a chemical denervation. This may explain the quick relief (sometimes from the day after the injection) obtained by a number of low back pain patients, treated with sclerosant injection.219
Another possible mode of action is through the sclerosing of pathologic neovessels that are frequently associated with painful tendinopathy.220,221 Finally, the potential of prolotherapy to stimulate release of growth factors favouring soft tissue healing has also been suggested as a possible mechanism.222
Indications (Table 5.9)
Ligaments
1. The main indication for sclerosant therapy is at the lumbar spine. In recurrent disc protrusions or in chronic backache from postural ligamentous pain (see p. 459), a series of infiltrations is made in all the dorsal ligaments of L4–L5–S1 motion segments.
Prolotherapy is also used for pain relief in ‘intractable backache’ of the lumbar spine (see p. 582). The positive effect after the injections is thought to be caused by the neurolytic effect of the phenol. The agent is infiltrated around the lateral or medial branch of the posterior ramus and may cause pain relief of months’ or years’ duration.
2. Sclerosing injections are also used in treating sacroiliac strains. Infiltration is always at the ligamentoperiosteal junction (see p. 608).
3. Recurring carpal subluxations or in the inferior tibiofibular ligament. Infiltration is into the remains of the ligament at the ligamentoperiosteal attachment. The injections can also be used in the treatment of recurrent subluxations and strain of the acromioclavicular joint.
Tendons
During the last decade some reports of good results with prolotherapy in the treatment of painful chronic mid-portion Achilles tendinosis were published.223,224 It is suggested that neovessels play a key part in causing chronic tendon pain, hence the curative effect of their sclerosis.225,226 Prolotherapy has also been used in the treatment of chronic infrapatellar tendinitis,220 hip adductor tendinopathy227 and chronic plantar fasciitis refractory to conservative care228. Also type II tennis elbow (tendinopathy of the origin of the extensor carpi radialis brevis) in which previous infiltrations with steroid have given poor or only temporary relief is a good indication for sclerosing injections.229,230
Side effects and complications
In 1993 Dorman published a survey of prolotherapy injections performed on a total of 494 845 patients.231 Of these, 343 897 were treated for low back pain. Only 66 minor complications were reported. These included 24 reports of allergic reactions and 29 instances of pneumothorax. All of these resolved without serious problems. There were also 14 reports of major complications, defined as the patient needing hospitalization or having transient or permanent nerve damage.
Results
A double-blind controlled study of prolotherapy was published in The Lancet in 1987.215 The investigators used a strict set of criteria (such as no litigation, long-standing pain, no severe medical illnesses and a diagnosis of ligamentous back pain). One half of a group of 81 patients received prolotherapy injections with a solution of dextrose, phenol, lidocaine (lignocaine) and glycerin, while the others were injected with saline. The average length of time of symptoms was 8.98 years in the treatment group and 10.72 years in the placebo group. The results showed a statistically significant difference in the two groups, with the prolotherapy group showing a marked decrease in subjective pain as compared to the saline groups (p < 0.00l at 6 months). A later double-blind study in 1993 showed similar results.232