Primary Care Assessment
Although it would be ideal for a family physician who is familiar with the patient’s and the family’s history to perform a primary care assessment because he or she would more likely be aware of any congenital or developmental problems, the patient’s immunization status, and any recent injuries or illnesses and therefore could provide continuity of care,1–3 many people today do not have a family physician. As health care changes occur, more and more health care professionals are becoming involved in assessment of patients who come to them as first-level providers of medical care. This may involve nurse practitioners, physician assistants, and other health care providers, as well as physicians in primary care facilities, physical therapists with direct access in private practice, clinicians in sole-charge facilities, and sports therapists working and traveling with teams.4–8 Thus it becomes important for clinicians to be able to evaluate and recognize the potential for health care problems, including systemic disease as a disease entity itself or a disease masquerading as neuromuscular dysfunction, that must be referred to the appropriate health professional.9,10 Primary care assessment is a form of triage in which the clinician decides whether the patient’s problem or problems fall within his or her scope of practice or should be referred to other health care professionals.11–15
In many ways, a primary care assessment is similar to a preparticipation examination used in sports because both assessments are used to clear patients of having certain problems that could affect activity and also to provide a mechanism in which problems can be referred to the appropriate health care professional.16–22 This process involves an understanding of disease as well as an ability to distinguish what system may be affected through a detailed history, observation and examination, and an understanding of different levels of reporting ability of the patient.9,23 It also requires the clinician to understand his or her limitations, the scope of practice of his or her chosen profession, and why the patient has come to see the clinician. For example, what is the patient’s complaint? Is it related to how the patient feels? Is it related to his or her occupation? Is it related to a certain population, age, or gender?18,24,25
If the patient has symptoms, several questions should be asked that relate to the symptoms26:
1. Where is the symptom, and does it radiate?
2. What does the symptom feel like?
4. Where does (did) the symptom start?
5. How long does the symptom last?
6. How often does the symptom occur?
7. What brings the symptom on?
Once these questions, and the ones discussed under the different systems as outlined later in the chapter, are answered, the examiner can decide to treat the patient or refer on to another health care professional, usually a physician. Goodman and Snyder27 clearly outline cases in which referral to a physician is necessary (Table 17-1). This chapter is not meant to be all inclusive of conditions and systems that may need referral. Complete systems assessment is left to other sources.26,27
TABLE 17-1
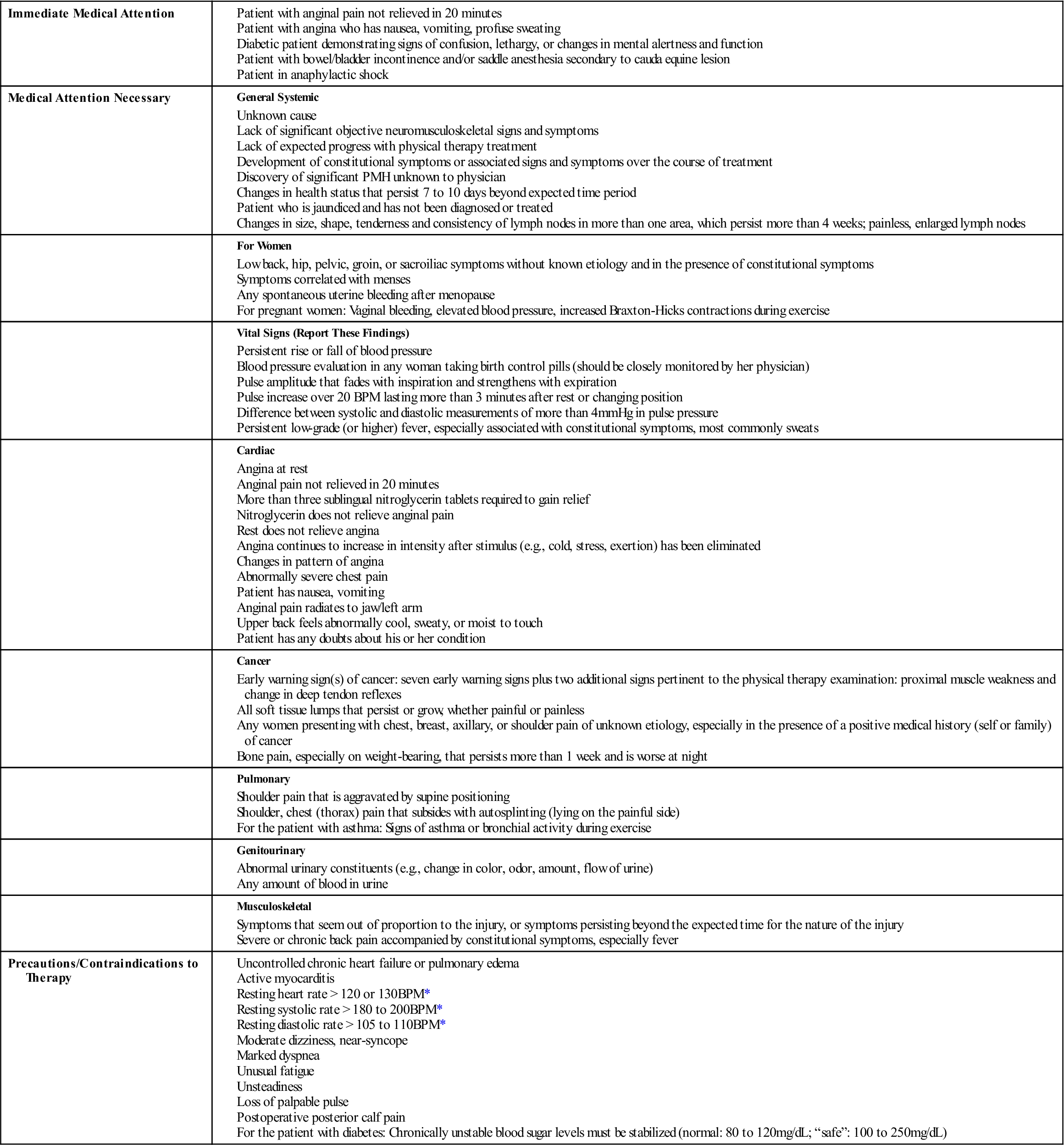
BPM, Beats per minute; PMH, past medical history.
*Unexplained or poorly tolerated by patient
From Goodman CC, Snyder TE: Differential diagnosis in physical therapy, Philadelphia, 1995, WB Saunders, pp. 18–20.
McKeag28 has outlined five specific populations in which special areas of possible concern should be included in an examination. In the prepubescent patient (6 to 10 years of age), assessments should include examination for congenital abnormalities that may not have been diagnosed previously. In the pubescent patient (11 to 15 years of age), the examination should include an evaluation of physical maturity and good health practices. The postpubescent or young adult group (16 to 30 years of age) has the widest variety of skills, levels, and motivation. For this group, the history of previous injuries and any sport-specific or activity-specific problems is particularly important. For the adult population (30 to 65 years of age), injury prevention (e.g., overuse), previous injury patterns, health concerns, and conditioning should be included in the examination. The final group consists of elderly patients (65 years of age or older), who require an examination based on individual requirements, because many of these people take up exercising or increased physical activity after a medical illness.20 Age-related changes and their possible consequences are outlined in Table 17-2.
TABLE 17-2
Selected Age-Related Changes and Their Consequences
| Organ/System | Age-Related Physiologic Change* | Consequence of Age-Related Physiologic Change | Disease, Not Age |
| General | ↑ Body fat | ↑ Volume of distribution for fat-soluble drugs | Obesity |
| ↓ Total body water | ↓ Volume of distribution for water-soluble drugs | Anorexia | |
| Eyes/Ears | Presbyopia | ↓ Accommodation | Blindness |
| Lens opacification | ↑ Susceptibility to glare | Deafness | |
| ↓ High-frequency acuity | Difficulty discriminating words if background noise is present | ||
| Endocrine | Impaired glucose tolerance | ↑ Glucose level in response to acute illness | Diabetes mellitus |
| ↓ Thyroxine clearance (and production) | ↓ T4 dose required in hypothyroidism | Thyroid dysfunction | |
| ↑ ADH, ↓ renin, and ↓ aldosterone | — | ↓ NA+, ↑ K+ | |
| ↓ Testosterone | — | Impotence | |
| ↓ Vitamin D absorption and activation | Osteopenia | Osteoporosis Osteomalacia |
|
| Respiratory | ↓ Lung elasticity and ↑ chest wall stiffness | Ventilation/perfusion mismatch and ↓ pO2 | Dyspnea Hypoxia |
| Cardiovascular | ↓ Arterial compliance and ↑ systolic BP → LVH | Hypotensive response to ↑ HR, volume depletion, or loss of atrial contraction | Syncope |
| ↓ β-adrenergic responsiveness | ↓ Cardiac output and HR response to stress | Heart failure | |
| ↓ Baroreceptor sensitivity and ↓ SA node automaticity | Impaired blood pressure response to standing, volume depletion | Heart block | |
| Gastrointestinal | ↓ Hepatic function | Delayed metabolism of some drugs | Cirrhosis |
| ↓ Gastric acidity | ↓ Ca+ absorption on empty stomach | Osteoporosis Vitamin B12 deficiency |
|
| ↓ Colonic motility | Constipation | Fecal impaction | |
| ↓ Anorectal function | — | Fecal incontinence | |
| Hematologic/ Immune system | ↓ Bone marrow reserve (?) | — | Anemia |
| ↓ T-cell function | False-negative PPD response | — | |
| ↑ Autoantibodies | False-positive rheumatoid factor, antinuclear antibody | Autoimmune disease | |
| Renal | ↓ Glomerular filtration rate | Impaired excretion of some drugs | ↑ Serum creatinine |
| ↓ Urine concentration/ dilution (see also Endocrine) | Delayed response to salt or fluid restriction or overload; nocturia | ↑↓ Na+ | |
| Genitourinary | Vaginal/urethral mucosal atrophy
Prostate enlargement |
Dyspareunia Bacteriuria ↑ Residual urine volume |
Symptomatic urinary tract infection Urinary incontinence Urinary retention |
| Musculoskeletal | ↓ Lean body mass, muscle | — | Functional impairment |
| ↓ Bone density | Osteopenia | Hip fracture | |
| Nervous system | Brain atrophy | Benign senescent forgetfulness | Dementia Delirium |
| ↓ Brain catechol synthesis | — | Depression | |
| ↓ Brain dopaminergic synthesis | Stiffer gait | Parkinson disease | |
| ↓ Righting reflexes | ↑ Body sway | Falls | |
| ↓ Stage 4 sleep | Early wakening, insomnia | Sleep apnea |
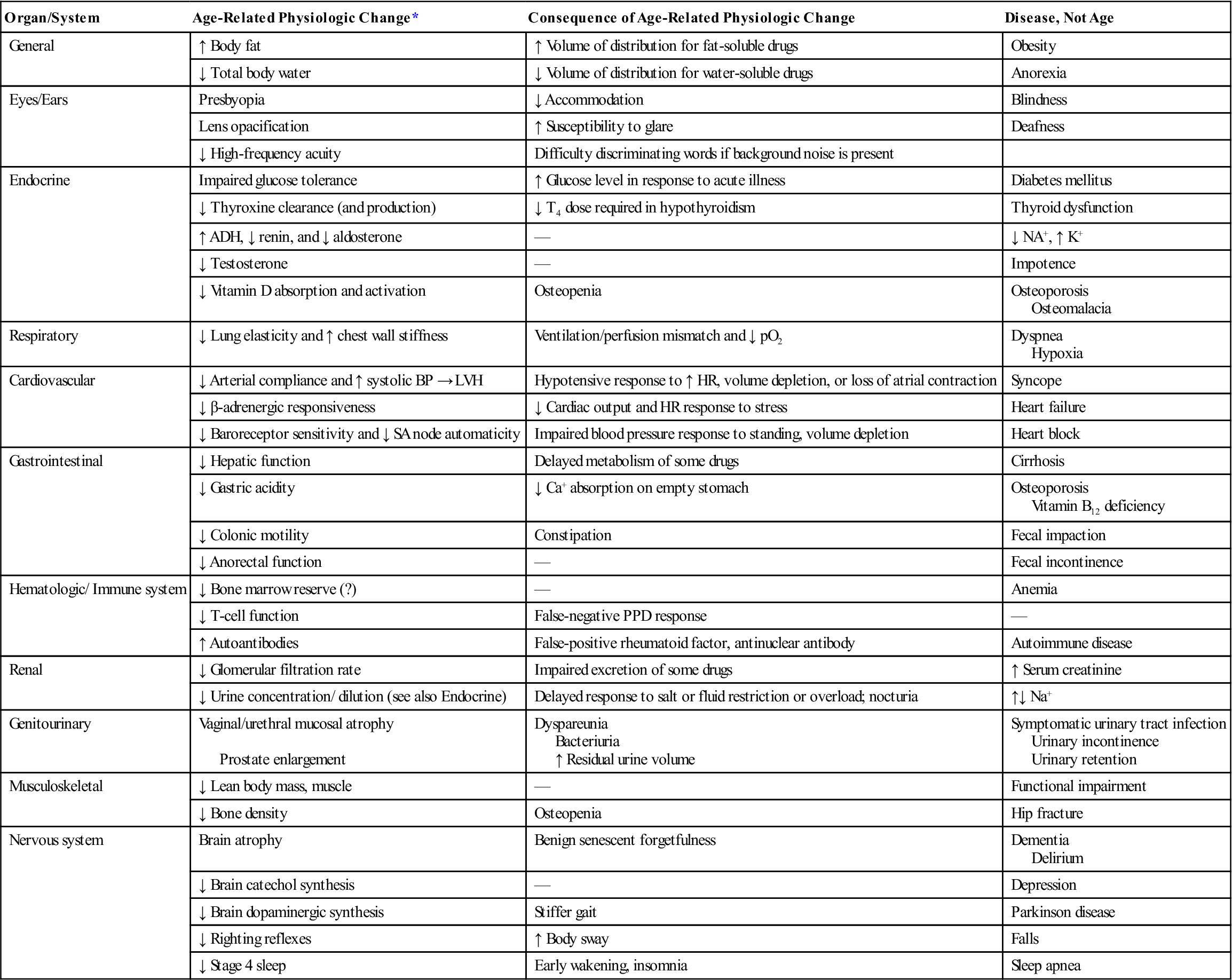
ADH, Antidiuretic hormone; BP, blood pressure; HR, heart rate; LVH, left ventricular hypertrophy; PPD, purified protein derivative, SA, sinoatrial; T4, thyroxine.
The table displays selected changes that occur normally with age and their physiologic consequences. Changes due to disease rather than to age are listed in the last column.
*Changes generally observed in healthy elderly subjects free of symptoms and detectable disease in the organ system studied. The changes are usually important only when the system is stressed or other factors are added (e.g., drugs, disease, or environmental challenge); they rarely result in symptoms otherwise.
From Resnick NM: Geriatric medicine. In Isselbacher KJ, et al, editors: Harrison’s principles of internal medicine, ed 13, New York, 1994, McGraw-Hill.
A primary care assessment may vary from a minimal medical examination or physical to rule out possible systemic problems to a very extensive examination involving laboratory tests, stress testing, profiling, x-rays, and other special protocols.29 History, as well as a physical examination, plays a major role.30–32 If the patient is going to be asked to do strenuous activity as part of his or her treatment program, various systems (e.g., heart, lungs) must be cleared to ensure the patient is capable of doing the activity.33
Objectives of the Evaluation
Primary care evaluations have many useful purposes.1,9,29,34,35 However, the examiner must remember that the primary purpose of the examination is to determine the patient’s health problem and to either treat the patient or refer him or her to the appropriate health care professional.1,9 As part of the examination, the examiner can establish baseline values for the patient. These may be compared with normal “textbook” values or used to determine change in the future. In other words, the assessment should not consist of simple “yes/no” questions. Instead, it must be very thorough to establish proper baseline levels.
The primary care assessment is used to determine the health status of the patient. It also helps to prevent injuries through identification of any abnormalities, physical inadequacies, or poor conditioning that may put the patient at risk.36 The examination may identify previously unsuspected conditions that are amenable to correction or that preclude participation in the desired activity. Similarly, the evaluation helps to avoid misinterpretation of findings that appear to be new but existed previously. For this reason, a review of previous health records, if possible, is also part of the primary care assessment.
The primary care assessment is also worthwhile to ensure that treatments have been carried out previously and that conditions previously diagnosed have been properly cared for. In this way, it acts as a screening process to ensure that treatment of potentially serious medical and surgical conditions has taken place. It also helps to rule out potentially serious or threatening conditions that may temporarily preclude the patient from participation in work or recreational activities. For example, with infectious mononucleosis, contact sports may be precluded for a time, because the patient’s spleen is enlarged and is more easily injured or ruptured.
The assessment also gives the clinician an opportunity to foster good health practices and to promote optimum health and fitness. The assessment enables the health care provider to give proper health guidance and to determine the general state of health of the patient.
The assessment also gives the examiner a chance to develop a rapport with the patient. The examiner can learn what motivates the patient and, at the same time, help establish the patient’s confidence in the health care staff. The examination may also be used to establish guidelines for the patient and health care team on questions of health, safety, and care. In addition, it provides an opportunity to counsel the patient.
Primary Care History
For a primary care assessment, the history plays a predominant role to ensure that questions related to the various systems are asked. A complete history can usually identify 60% to 75% of the problems affecting a patient.22,29,37 For the young person or the patient with communication problems, both the patient and his or her parent or guardian should provide the history to ensure completeness. The rest of the assessment proceeds from the information determined in the history. The history provides details regarding health problems and injuries and enables the examiner to focus on any abnormalities that it brings out.29 Generally, the history is completed by the patient’s answering questions in a yes/no format (see Appendix 17-1 on the Evolve website for a generic primary care assessment questionnaire). Using such a format decreases the chance of the patient forgetting something.23 The “yes” answers then are investigated further in other parts of the assessment (see Appendix 17-2 on the Evolve website). It is important, however, that the “no” answers also be checked for accuracy. Ideally, oral histories, in which the health care professional asks the questions, are more accurate; but usually, because of time constraints, this is not possible. The history should include the patient’s medical history as well as the family’s medical history to rule out any congenital, hereditary, or injury problems. It is important that a complete health history be obtained, because the patient may leave out or hide information that may preclude the patient from taking part in a desired activity or because of possible secondary gain.37
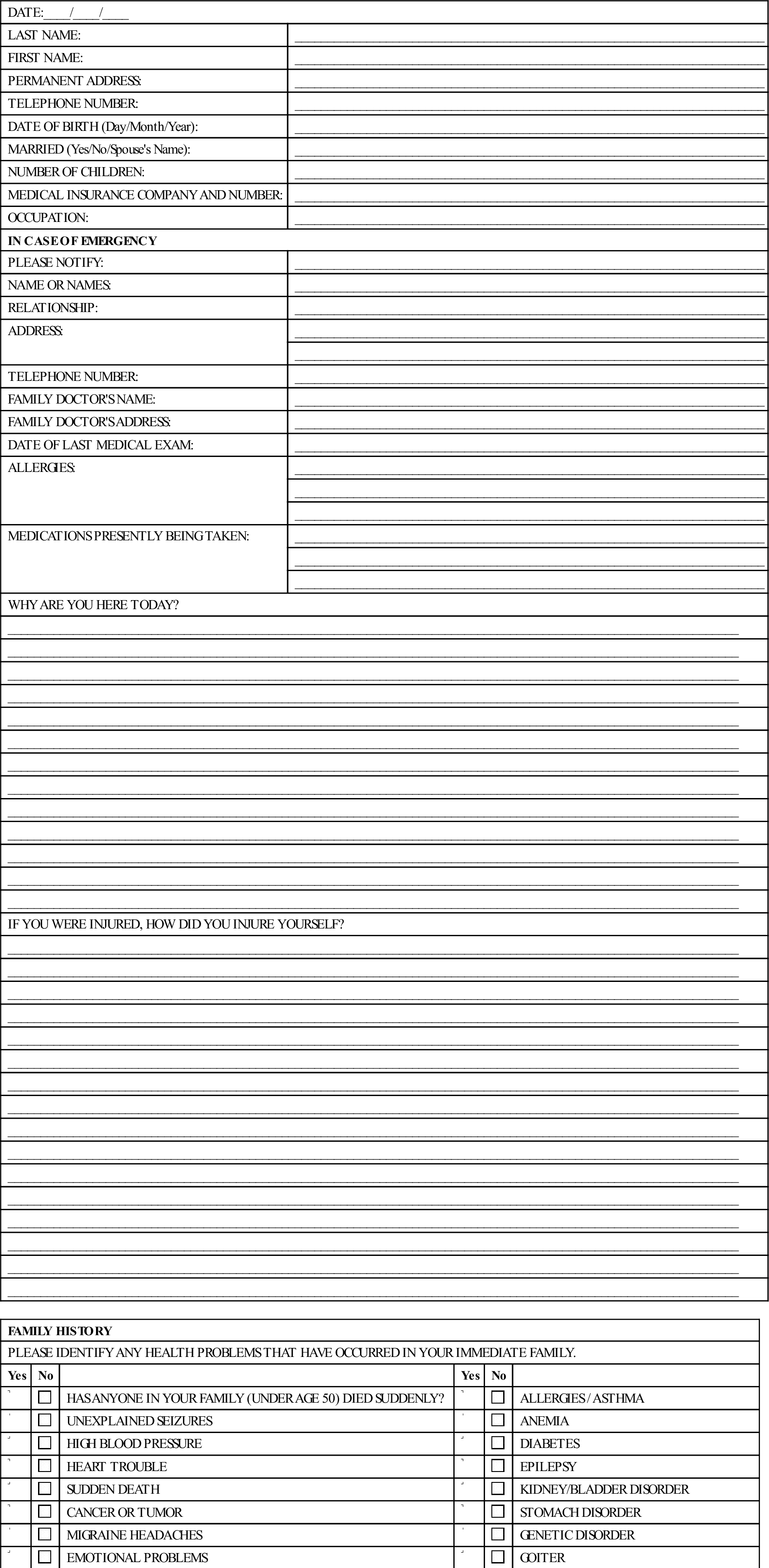
APPENDIX 17-1
Primary Care Assessment Patient Questionnaire
| DATE:____/____/____ | |
| LAST NAME: | ________________________________________________________________________ |
| FIRST NAME: | ________________________________________________________________________ |
| PERMANENT ADDRESS: | ________________________________________________________________________ |
| TELEPHONE NUMBER: | ________________________________________________________________________ |
| DATE OF BIRTH (Day/Month/Year): | ________________________________________________________________________ |
| MARRIED (Yes/No/Spouse’s Name): | ________________________________________________________________________ |
| NUMBER OF CHILDREN: | ________________________________________________________________________ |
| MEDICAL INSURANCE COMPANY AND NUMBER: | ________________________________________________________________________ |
| OCCUPATION: | ________________________________________________________________________ |
| IN CASE OF EMERGENCY | |
| PLEASE NOTIFY: | ________________________________________________________________________ |
| NAME OR NAMES: | ________________________________________________________________________ |
| RELATIONSHIP: | ________________________________________________________________________ |
| ADDRESS: | ________________________________________________________________________ |
| ________________________________________________________________________ | |
| TELEPHONE NUMBER: | ________________________________________________________________________ |
| FAMILY DOCTOR’S NAME: | ________________________________________________________________________ |
| FAMILY DOCTOR’S ADDRESS: | ________________________________________________________________________ |
| DATE OF LAST MEDICAL EXAM: | ________________________________________________________________________ |
| ALLERGIES: | ________________________________________________________________________ |
| ________________________________________________________________________ | |
| ________________________________________________________________________ | |
| MEDICATIONS PRESENTLY BEING TAKEN: | ________________________________________________________________________ |
| ________________________________________________________________________ | |
| ________________________________________________________________________ | |
| WHY ARE YOU HERE TODAY? | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| IF YOU WERE INJURED, HOW DID YOU INJURE YOURSELF? | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| ________________________________________________________________________________________________________________ | |
| FAMILY HISTORY | |||||
| PLEASE IDENTIFY ANY HEALTH PROBLEMS THAT HAVE OCCURRED IN YOUR IMMEDIATE FAMILY. | |||||
| Yes | No | Yes | No | ||
 |
 |
HAS ANYONE IN YOUR FAMILY (UNDER AGE 50) DIED SUDDENLY? |  |
 |
ALLERGIES / ASTHMA |
 |
 |
UNEXPLAINED SEIZURES |  |
 |
ANEMIA |
 |
 |
HIGH BLOOD PRESSURE |  |
 |
DIABETES |
 |
 |
HEART TROUBLE |  |
 |
EPILEPSY |
 |
 |
SUDDEN DEATH |  |
 |
KIDNEY/BLADDER DISORDER |
 |
 |
CANCER OR TUMOR |  |
 |
STOMACH DISORDER |
 |
 |
MIGRAINE HEADACHES |  |
 |
GENETIC DISORDER |
 |
 |
EMOTIONAL PROBLEMS |  |
 |
GOITER |
 |
 |
ARTHRITIS |  |
 |
NEUROLOGICAL DISORDERS |
 |
 |
OBESITY |  |
 |
TUBERCULOSIS |
 |
 |
BLOOD DISORDERS OR EARLY BLEEDING |  |
 |
ABNORMAL NUMBNESS OR ANESTHESIA |
| SPECIFY:________________________________________________________________________________________________________ ________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________ |
|||||
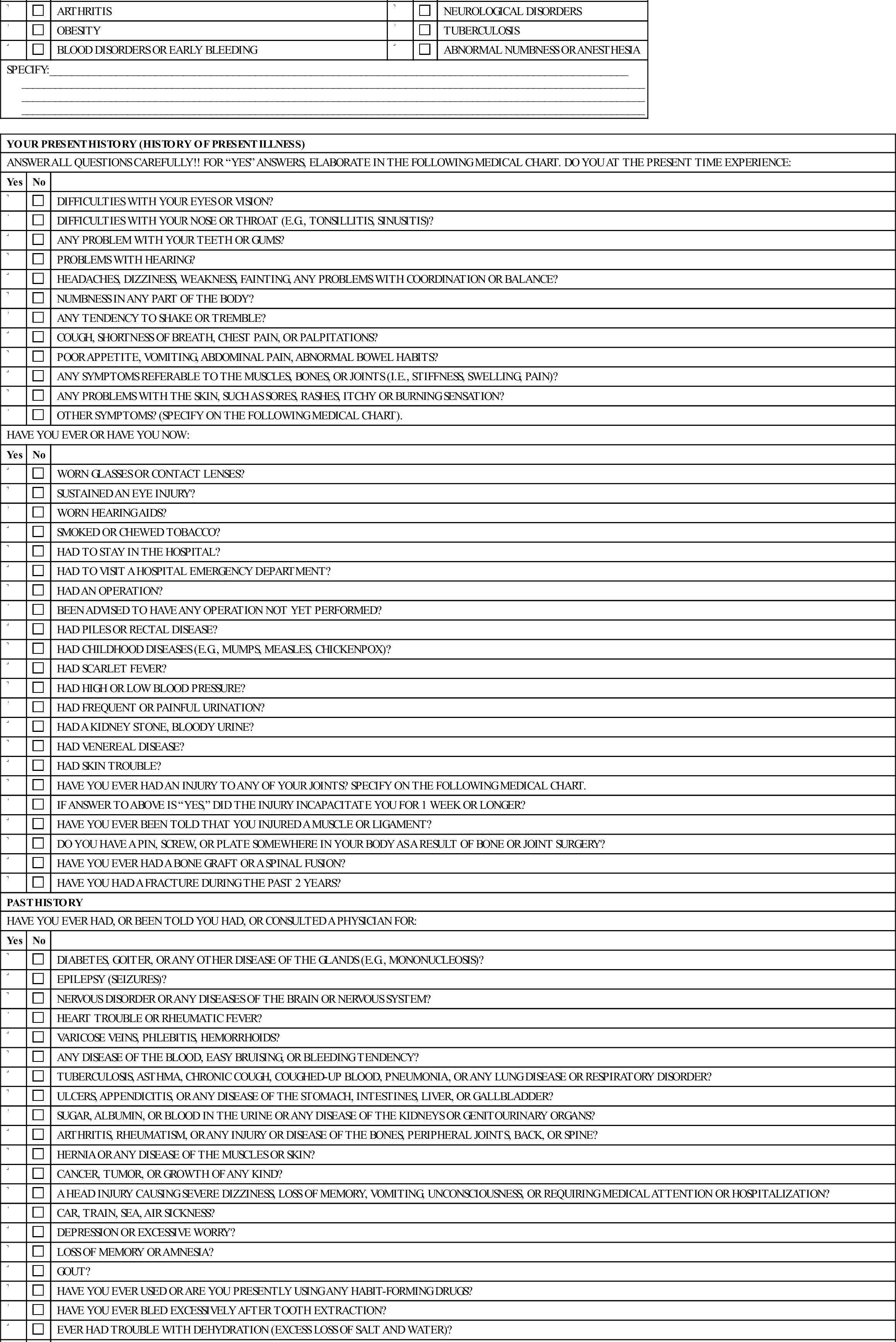
| YOUR PRESENT HISTORY (HISTORY OF PRESENT ILLNESS) | ||
| ANSWER ALL QUESTIONS CAREFULLY!! FOR “YES” ANSWERS, ELABORATE IN THE FOLLOWING MEDICAL CHART. DO YOU AT THE PRESENT TIME EXPERIENCE: | ||
| Yes | No | |
 |
 |
DIFFICULTIES WITH YOUR EYES OR VISION? |
 |
 |
DIFFICULTIES WITH YOUR NOSE OR THROAT (E.G., TONSILLITIS, SINUSITIS)? |
 |
 |
ANY PROBLEM WITH YOUR TEETH OR GUMS? |
 |
 |
PROBLEMS WITH HEARING? |
 |
 |
HEADACHES, DIZZINESS, WEAKNESS, FAINTING, ANY PROBLEMS WITH COORDINATION OR BALANCE? |
 |
 |
NUMBNESS IN ANY PART OF THE BODY? |
 |
 |
ANY TENDENCY TO SHAKE OR TREMBLE? |
 |
 |
COUGH, SHORTNESS OF BREATH, CHEST PAIN, OR PALPITATIONS? |
 |
 |
POOR APPETITE, VOMITING, ABDOMINAL PAIN, ABNORMAL BOWEL HABITS? |
 |
 |
ANY SYMPTOMS REFERABLE TO THE MUSCLES, BONES, OR JOINTS (I.E., STIFFNESS, SWELLING, PAIN)? |
 |
 |
ANY PROBLEMS WITH THE SKIN, SUCH AS SORES, RASHES, ITCHY OR BURNING SENSATION? |
 |
 |
OTHER SYMPTOMS? (SPECIFY ON THE FOLLOWING MEDICAL CHART). |
| HAVE YOU EVER OR HAVE YOU NOW: | ||
| Yes | No | |
 |
 |
WORN GLASSES OR CONTACT LENSES? |
 |
 |
SUSTAINED AN EYE INJURY? |
 |
 |
WORN HEARING AIDS? |
 |
 |
SMOKED OR CHEWED TOBACCO? |
 |
 |
HAD TO STAY IN THE HOSPITAL? |
 |
 |
HAD TO VISIT A HOSPITAL EMERGENCY DEPARTMENT? |
 |
 |
HAD AN OPERATION? |
 |
 |
BEEN ADVISED TO HAVE ANY OPERATION NOT YET PERFORMED? |
 |
 |
HAD PILES OR RECTAL DISEASE? |
 |
 |
HAD CHILDHOOD DISEASES (E.G., MUMPS, MEASLES, CHICKENPOX)? |
 |
 |
HAD SCARLET FEVER? |
 |
 |
HAD HIGH OR LOW BLOOD PRESSURE? |
 |
 |
HAD FREQUENT OR PAINFUL URINATION? |
 |
 |
HAD A KIDNEY STONE, BLOODY URINE? |
 |
 |
HAD VENEREAL DISEASE? |
 |
 |
HAD SKIN TROUBLE? |
 |
 |
HAVE YOU EVER HAD AN INJURY TO ANY OF YOUR JOINTS? SPECIFY ON THE FOLLOWING MEDICAL CHART. |
 |
 |
IF ANSWER TO ABOVE IS “YES,” DID THE INJURY INCAPACITATE YOU FOR 1 WEEK OR LONGER? |
 |
 |
HAVE YOU EVER BEEN TOLD THAT YOU INJURED A MUSCLE OR LIGAMENT? |
 |
 |
DO YOU HAVE A PIN, SCREW, OR PLATE SOMEWHERE IN YOUR BODY AS A RESULT OF BONE OR JOINT SURGERY? |
 |
 |
HAVE YOU EVER HAD A BONE GRAFT OR A SPINAL FUSION? |
 |
 |
HAVE YOU HAD A FRACTURE DURING THE PAST 2 YEARS? |
| PAST HISTORY | ||
| HAVE YOU EVER HAD, OR BEEN TOLD YOU HAD, OR CONSULTED A PHYSICIAN FOR: | ||
| Yes | No | |
 |
 |
DIABETES, GOITER, OR ANY OTHER DISEASE OF THE GLANDS (E.G., MONONUCLEOSIS)? |
 |
 |
EPILEPSY (SEIZURES)? |
 |
 |
NERVOUS DISORDER OR ANY DISEASES OF THE BRAIN OR NERVOUS SYSTEM? |
 |
 |
HEART TROUBLE OR RHEUMATIC FEVER? |
 |
 |
VARICOSE VEINS, PHLEBITIS, HEMORRHOIDS? |
 |
 |
ANY DISEASE OF THE BLOOD, EASY BRUISING, OR BLEEDING TENDENCY? |
 |
 |
TUBERCULOSIS, ASTHMA, CHRONIC COUGH, COUGHED-UP BLOOD, PNEUMONIA, OR ANY LUNG DISEASE OR RESPIRATORY DISORDER? |
 |
 |
ULCERS, APPENDICITIS, OR ANY DISEASE OF THE STOMACH, INTESTINES, LIVER, OR GALLBLADDER? |
 |
 |
SUGAR, ALBUMIN, OR BLOOD IN THE URINE OR ANY DISEASE OF THE KIDNEYS OR GENITOURINARY ORGANS? |
 |
 |
ARTHRITIS, RHEUMATISM, OR ANY INJURY OR DISEASE OF THE BONES, PERIPHERAL JOINTS, BACK, OR SPINE? |
 |
 |
HERNIA OR ANY DISEASE OF THE MUSCLES OR SKIN? |
 |
 |
CANCER, TUMOR, OR GROWTH OF ANY KIND? |
 |
 |
A HEAD INJURY CAUSING SEVERE DIZZINESS, LOSS OF MEMORY, VOMITING, UNCONSCIOUSNESS, OR REQUIRING MEDICAL ATTENTION OR HOSPITALIZATION? |
 |
 |
CAR, TRAIN, SEA, AIR SICKNESS? |
 |
 |
DEPRESSION OR EXCESSIVE WORRY? |
 |
 |
LOSS OF MEMORY OR AMNESIA? |
 |
 |
GOUT? |
 |
 |
HAVE YOU EVER USED OR ARE YOU PRESENTLY USING ANY HABIT-FORMING DRUGS? |
 |
 |
HAVE YOU EVER BLED EXCESSIVELY AFTER TOOTH EXTRACTION? |
 |
 |
EVER HAD TROUBLE WITH DEHYDRATION (EXCESS LOSS OF SALT AND WATER)? |
 |
 |
BEEN MORE THIRSTY THAN USUAL LATELY? |
 |
 |
EVER HAD HEAT STROKE OR ANOTHER HEAT DISORDER (FAILURE OF BODY’S HEAT-REGULATING SYSTEM RESULTING IN THE BODY TEMPERATURE ABOVE 40.5° C (105° F)? |
 |
 |
WEIGHT CHANGED IN THE LAST YEAR? GAIN_____KG; LOSS_____KG |
 |
 |
ANY EXPLANATION FOR THIS WEIGHT CHANGE? (SPECIFY ON THE FOLLOWING MEDICAL CHART. |
 |
 |
HAD ANY ADDITIONAL ILLNESS, INJURIES (OTHER THAN CHILDHOOD DISEASE)? |
 |
 |
ARE YOU PRESENTLY UNDER A PHYSICIAN’S CARE FOR ANY DIFFICULTY NOT ALREADY DISCUSSED? |
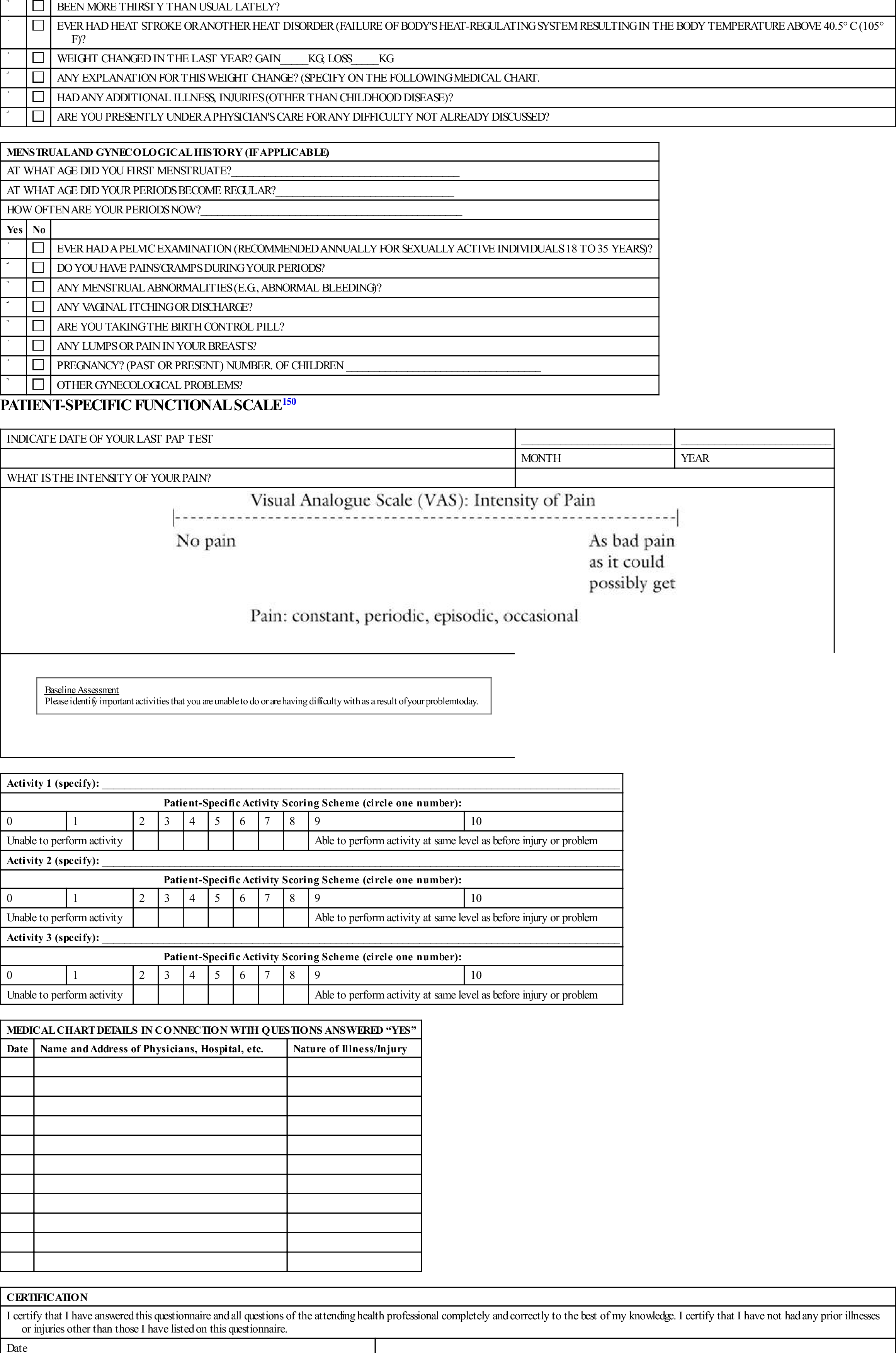
| MENSTRUAL AND GYNECOLOGICAL HISTORY (IF APPLICABLE) | ||
| AT WHAT AGE DID YOU FIRST MENSTRUATE?_________________________________________ | ||
| AT WHAT AGE DID YOUR PERIODS BECOME REGULAR?________________________________ | ||
| HOW OFTEN ARE YOUR PERIODS NOW?_______________________________________________ | ||
| Yes | No | |
 |
 |
EVER HAD A PELVIC EXAMINATION (RECOMMENDED ANNUALLY FOR SEXUALLY ACTIVE INDIVIDUALS 18 TO 35 YEARS)? |
 |
 |
DO YOU HAVE PAINS/CRAMPS DURING YOUR PERIODS? |
 |
 |
ANY MENSTRUAL ABNORMALITIES (E.G., ABNORMAL BLEEDING)? |
 |
 |
ANY VAGINAL ITCHING OR DISCHARGE? |
 |
 |
ARE YOU TAKING THE BIRTH CONTROL PILL? |
 |
 |
ANY LUMPS OR PAIN IN YOUR BREASTS? |
 |
 |
PREGNANCY? (PAST OR PRESENT) NUMBER. OF CHILDREN ___________________________________ |
 |
 |
OTHER GYNECOLOGICAL PROBLEMS? |
| INDICATE DATE OF YOUR LAST PAP TEST | ___________________________ | ___________________________ |
| MONTH | YEAR | |
| WHAT IS THE INTENSITY OF YOUR PAIN? | ||
 |
||
| PATIENT-SPECIFIC FUNCTIONAL SCALE150 | ||
|
Baseline Assessment Please identify important activities that you are unable to do or are having difficulty with as a result of your problem today. |
||
| Activity 1 (specify): _____________________________________________________________________________________________ | ||||||||||
| Patient-Specific Activity Scoring Scheme (circle one number): | ||||||||||
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Unable to perform activity | Able to perform activity at same level as before injury or problem | |||||||||
| Activity 2 (specify): _____________________________________________________________________________________________ | ||||||||||
| Patient-Specific Activity Scoring Scheme (circle one number): | ||||||||||
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Unable to perform activity | Able to perform activity at same level as before injury or problem | |||||||||
| Activity 3 (specify): _____________________________________________________________________________________________ | ||||||||||
| Patient-Specific Activity Scoring Scheme (circle one number): | ||||||||||
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Unable to perform activity | Able to perform activity at same level as before injury or problem | |||||||||
| MEDICAL CHART DETAILS IN CONNECTION WITH QUESTIONS ANSWERED “YES” | ||
| Date | Name and Address of Physicians, Hospital, etc. | Nature of Illness/Injury |
| CERTIFICATION | |
| I certify that I have answered this questionnaire and all questions of the attending health professional completely and correctly to the best of my knowledge. I certify that I have not had any prior illnesses or injuries other than those I have listed on this questionnaire. | |
| Date___________________ | ________________________________ |
| Patient’s signature | |
| ________________________________ | |
| Print name | |
| CONSENT FOR TRANSMITTAL OF INFORMATION | |
| I, ______________________, give my permission for the transmittal of the results of this medical examination to the appropriate health care professional. The confidentiality of these medical records is to be preserved. | |
| Date___________________ | Signed__________________________ |
| Place__________________ | Witness_________________________ |
| RECORD OF CONSENT FOR MINORS | |
| I, ______________________, give my permission for emergency medical/surgical care to be given by the appropriate health care professional to | |
| ________________________who is my son /daughter. | |
| It is understood that wherever possible I shall be contacted, informed of the problem, diagnosis, treatment required, and the hoped-for results. | |
| Date__________________ | Signed________________________ |
| Place_________________ | Witness________________________ |
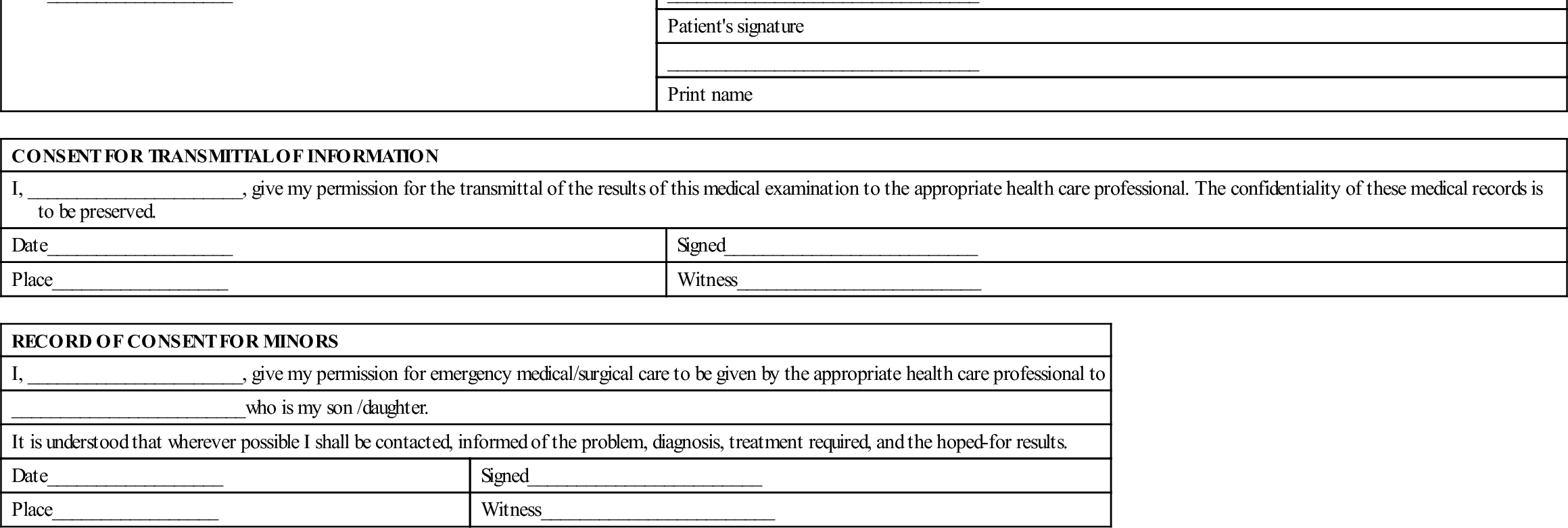
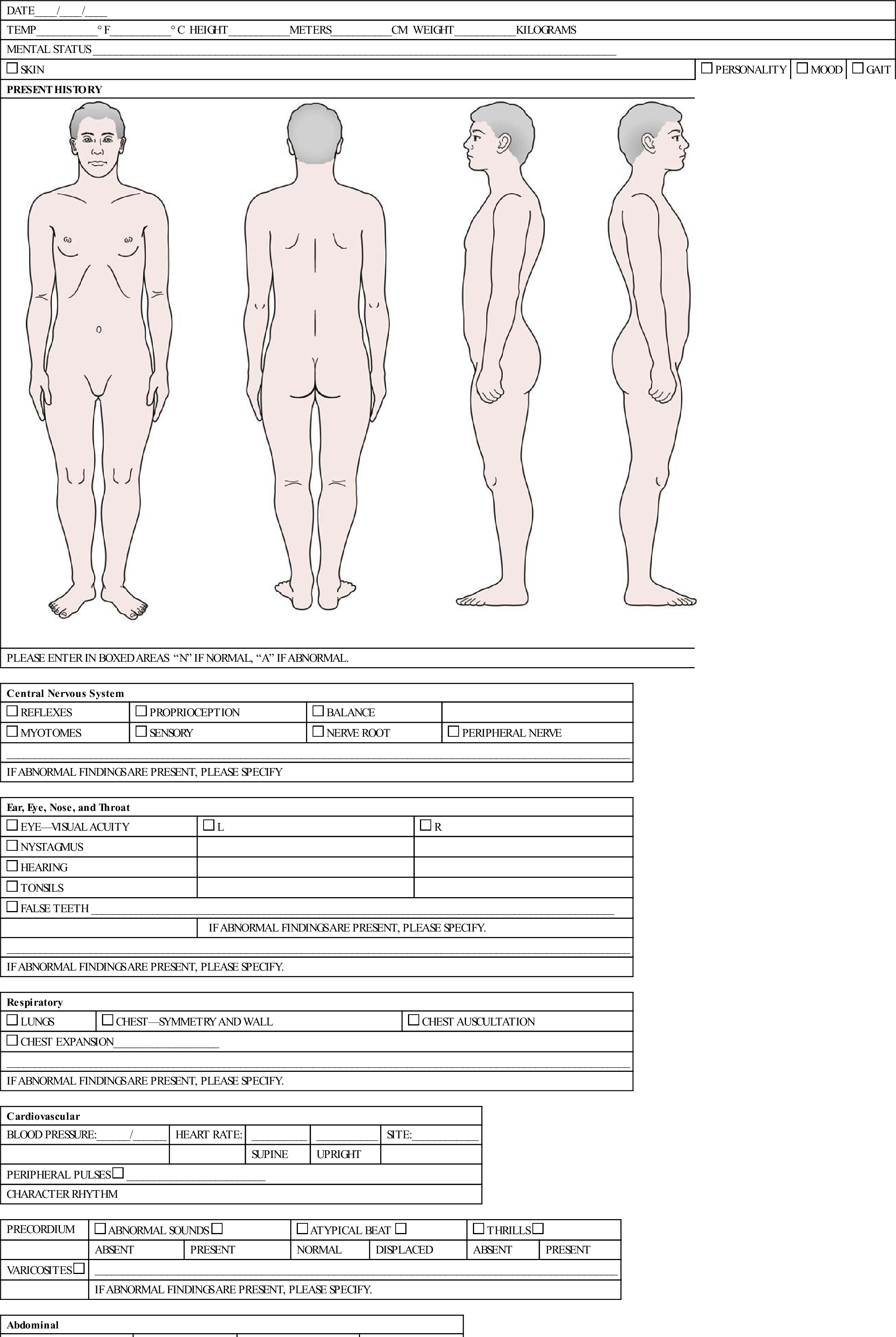
APPENDIX 17-2
Primary Health Care Examination
| DATE____/____/____ | |||
| TEMP___________° F___________° C HEIGHT___________METERS___________CM WEIGHT___________KILOGRAMS | |||
| MENTAL STATUS ______________________________________________________________________________________________ | |||
 SKIN SKIN |
 PERSONALITY PERSONALITY |
 MOOD MOOD |
 GAIT GAIT |
| PRESENT HISTORY |
 |
| PLEASE ENTER IN BOXED AREAS “N” IF NORMAL, “A” IF ABNORMAL. |
| Central Nervous System | |||
 REFLEXES REFLEXES |
 PROPRIOCEPTION PROPRIOCEPTION |
 BALANCE BALANCE |
|
 MYOTOMES MYOTOMES |
 SENSORY SENSORY |
 NERVE ROOT NERVE ROOT |
 PERIPHERAL NERVE PERIPHERAL NERVE |
| ________________________________________________________________________________________________________________ | |||
| IF ABNORMAL FINDINGS ARE PRESENT, PLEASE SPECIFY | |||
| Ear, Eye, Nose, and Throat | ||
 EYE—VISUAL ACUITY EYE—VISUAL ACUITY |
 L L |
 R R |
 NYSTAGMUS NYSTAGMUS |
||
 HEARING HEARING |
||
 TONSILS TONSILS |
||
 FALSE TEETH ______________________________________________________________________________________________ FALSE TEETH ______________________________________________________________________________________________ |
||
| IF ABNORMAL FINDINGS ARE PRESENT, PLEASE SPECIFY. | ||
| ________________________________________________________________________________________________________________ | ||
| IF ABNORMAL FINDINGS ARE PRESENT, PLEASE SPECIFY. | ||
| Respiratory | ||
 LUNGS LUNGS |
 CHEST—SYMMETRY AND WALL CHEST—SYMMETRY AND WALL |
 CHEST AUSCULTATION CHEST AUSCULTATION |
 CHEST EXPANSION___________________ CHEST EXPANSION___________________ |
||
| ________________________________________________________________________________________________________________ | ||
| IF ABNORMAL FINDINGS ARE PRESENT, PLEASE SPECIFY. | ||
| Cardiovascular | ||||
| BLOOD PRESSURE:______/______ | HEART RATE: | __________ | ___________ | SITE:____________ |
| SUPINE | UPRIGHT | |||
PERIPHERAL PULSES  _________________________ _________________________ |
||||
| CHARACTER RHYTHM | ||||
| PRECORDIUM |  ABNORMAL SOUNDS ABNORMAL SOUNDS  |
 ATYPICAL BEAT ATYPICAL BEAT  |
 THRILLS THRILLS  |
|||
| ABSENT | PRESENT | NORMAL | DISPLACED | ABSENT | PRESENT | |
VARICOSITES  |
______________________________________________________________________________________________ | |||||
| IF ABNORMAL FINDINGS ARE PRESENT, PLEASE SPECIFY. | ||||||
| Abdominal | |||||||
 ABDOMINAL WALL ABDOMINAL WALL  |
 TENDERNESS TENDERNESS  |
 ORGANOMEGALY ORGANOMEGALY  |
 MASSES MASSES  |
||||
| NORMAL | ABNORMAL | ABSENT | PRESENT | ABSENT | PRESENT | ABSENT | PRESENT |
| Genitourinary | ||
 HERNIA HERNIA  |
 GENITALIA GENITALIA |
|
| ABSENT | PRESENT | |
 BLOOD IN URINE BLOOD IN URINE |
||
 RECTAL RECTAL |
||
 SACRAL SACRAL |
 COCCYX COCCYX |
|
| Musculoskeletal System | ||
 CERVICAL CERVICAL |
 THORACIC THORACIC |
 LUMBAR LUMBAR |
 CHEST/RIBS CHEST/RIBS |
||
| ________________________________________________________________________________________________________________ | ||
| IF ABNORMAL FINDINGS ARE PRESENT, PLEASE SPECIFY. | ||
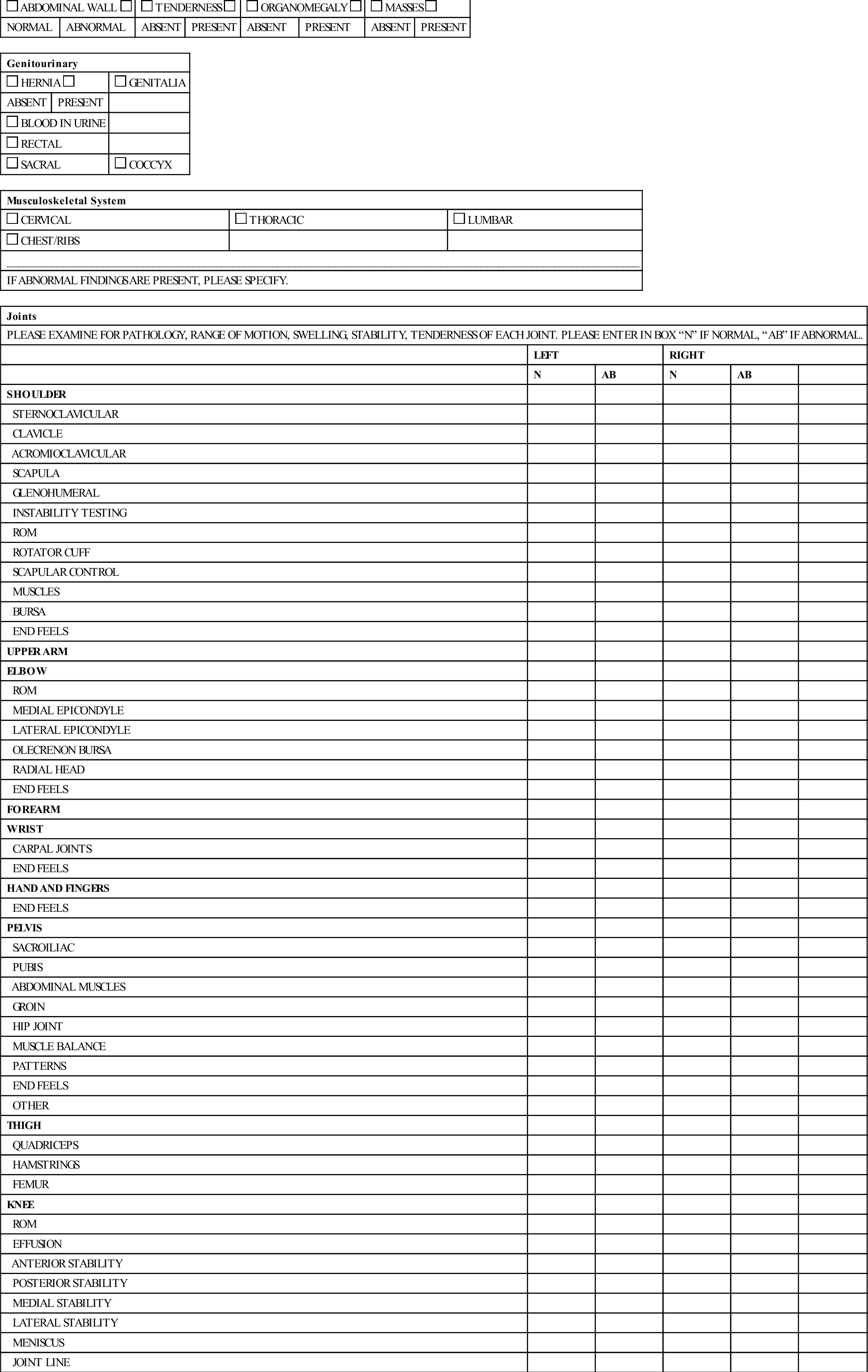
| Joints | |||||
| PLEASE EXAMINE FOR PATHOLOGY, RANGE OF MOTION, SWELLING, STABILITY, TENDERNESS OF EACH JOINT. PLEASE ENTER IN BOX “N” IF NORMAL, “AB” IF ABNORMAL. | |||||
| LEFT | RIGHT | ||||
| N | AB | N | AB | ||
| SHOULDER | |||||
| STERNOCLAVICULAR | |||||
| CLAVICLE | |||||
| ACROMIOCLAVICULAR | |||||
| SCAPULA | |||||
| GLENOHUMERAL | |||||
| INSTABILITY TESTING | |||||
| ROM | |||||
| ROTATOR CUFF | |||||
| SCAPULAR CONTROL | |||||
| MUSCLES | |||||
| BURSA | |||||
| END FEELS | |||||
| UPPER ARM | |||||
| ELBOW | |||||
| ROM | |||||
| MEDIAL EPICONDYLE | |||||
| LATERAL EPICONDYLE | |||||
| OLECRENON BURSA | |||||
| RADIAL HEAD | |||||
| END FEELS | |||||
| FOREARM | |||||
| WRIST | |||||
| CARPAL JOINTS | |||||
| END FEELS | |||||
| HAND AND FINGERS | |||||
| END FEELS | |||||
| PELVIS | |||||
| SACROILIAC | |||||
| PUBIS | |||||
| ABDOMINAL MUSCLES | |||||
| GROIN | |||||
| HIP JOINT | |||||
| MUSCLE BALANCE | |||||
| PATTERNS | |||||
| END FEELS | |||||
| OTHER | |||||
| THIGH | |||||
| QUADRICEPS | |||||
| HAMSTRINGS | |||||
| FEMUR | |||||
| KNEE | |||||
| ROM | |||||
| EFFUSION | |||||
| ANTERIOR STABILITY | |||||
| POSTERIOR STABILITY | |||||
| MEDIAL STABILITY | |||||
| LATERAL STABILITY | |||||
| MENISCUS | |||||
| JOINT LINE | |||||
| TENDERNESS | |||||
| CREPITUS | |||||
| END FEELS | |||||
| -PATELLA | |||||
| -LATERAL APPREHENSION |
|||||
| -TENDERNESS | |||||
| -Q-ANGLE | |||||
| -PATELLA CREPITUS | |||||
| -POPLITEAL FOSSA | |||||
| LOWER LEG | |||||
| TIBIA OR FIBULA | |||||
| ANT. COMPARTMENT | |||||
| POST. COMPARTMENT | |||||
| TENDO ACHILLES | |||||
| ANKLE | |||||
| ROM | |||||
| MEDIAL OR LATERAL MALLEOLUS | |||||
| ANT. DRAWER | |||||
| BURSA | |||||
| END FEELS | |||||
| FOOT | |||||
| INVERSION | |||||
| EVERSION | |||||
| MEDIAL LONGITUDINAL ARCH |
|||||
| LATERAL LONIGTUDINAL ARCH |
|||||
| PES PLANUS | |||||
| PES CAVUS | |||||
| METATARSAL ARCH | |||||
| END FEELS | |||||
| TOES | |||||
| LOWER LEG ALIGNMENT | |||||
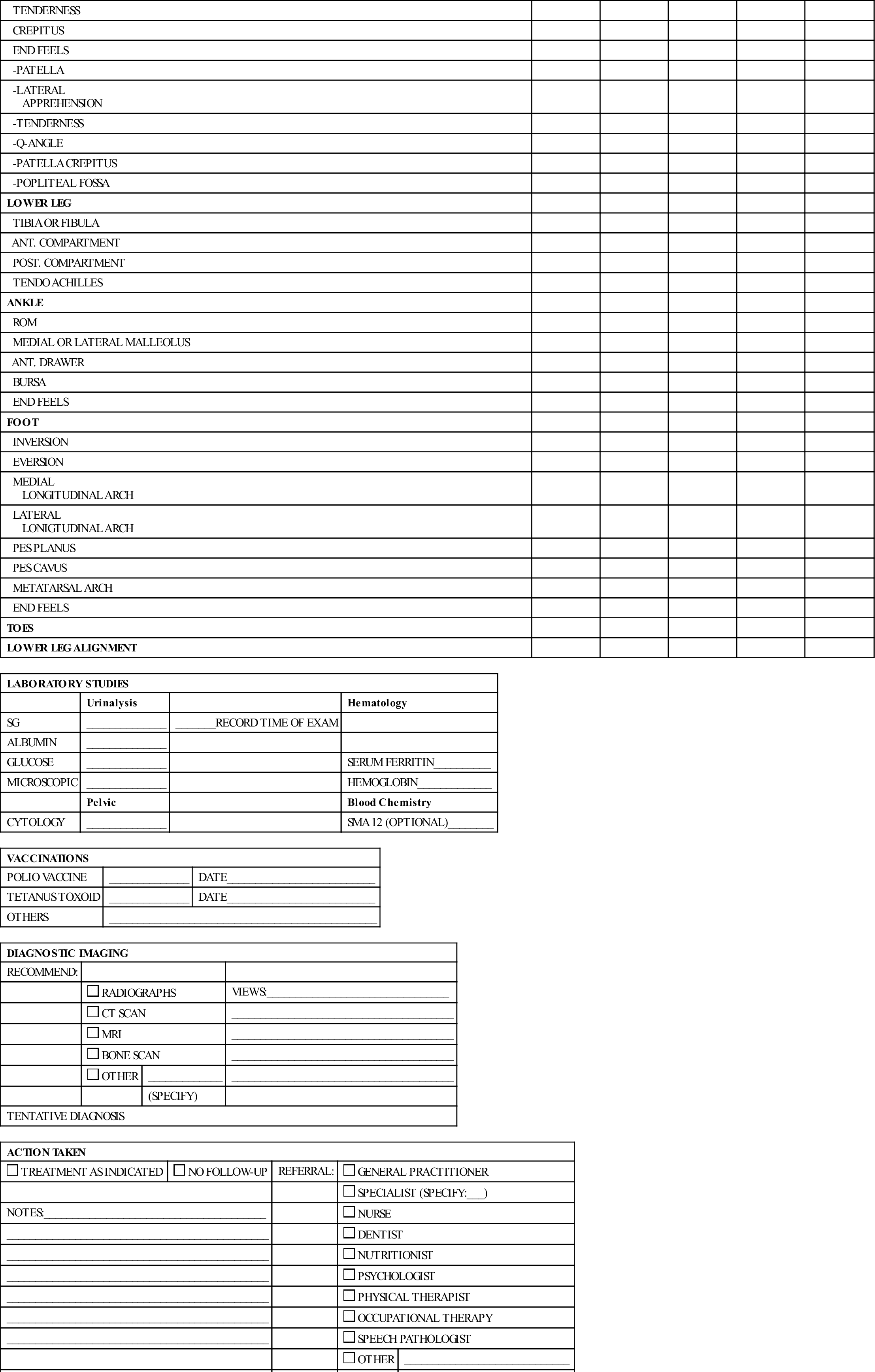
| LABORATORY STUDIES | |||
| Urinalysis | Hematology | ||
| SG | ______________ | _______RECORD TIME OF EXAM | |
| ALBUMIN | ______________ | ||
| GLUCOSE | ______________ | SERUM FERRITIN__________ | |
| MICROSCOPIC | ______________ | HEMOGLOBIN_____________ | |
| Pelvic | Blood Chemistry | ||
| CYTOLOGY | ______________ | SMA 12 (OPTIONAL)________ | |
| VACCINATIONS | ||
| POLIO VACCINE | ______________ | DATE__________________________ |
| TETANUS TOXOID | ______________ | DATE__________________________ |
| OTHERS | _______________________________________________ | |
| DIAGNOSTIC IMAGING | |||
| RECOMMEND: | |||
 RADIOGRAPHS RADIOGRAPHS |
VIEWS:________________________________ | ||
 CT SCAN CT SCAN |
_______________________________________ | ||
 MRI MRI |
_______________________________________ | ||
 BONE SCAN BONE SCAN |
_______________________________________ | ||
 OTHER OTHER |
_____________ | _______________________________________ | |
| (SPECIFY) | |||
| TENTATIVE DIAGNOSIS | |||
| ACTION TAKEN | ||||
 TREATMENT AS INDICATED TREATMENT AS INDICATED |
 NO FOLLOW-UP NO FOLLOW-UP |
REFERRAL: |  GENERAL PRACTITIONER GENERAL PRACTITIONER |
|
 SPECIALIST (SPECIFY:___) SPECIALIST (SPECIFY:___) |
||||
| NOTES:_______________________________________ |  NURSE NURSE |
|||
| ______________________________________________ |  DENTIST DENTIST |
|||
| ______________________________________________ |  NUTRITIONIST NUTRITIONIST |
|||
| ______________________________________________ |  PSYCHOLOGIST PSYCHOLOGIST |
|||
| ______________________________________________ |  PHYSICAL THERAPIST PHYSICAL THERAPIST |
|||
| ______________________________________________ |  OCCUPATIONAL THERAPY OCCUPATIONAL THERAPY |
|||
| ______________________________________________ |  SPEECH PATHOLOGIST SPEECH PATHOLOGIST |
|||
 OTHER OTHER |
_____________________________ | |||
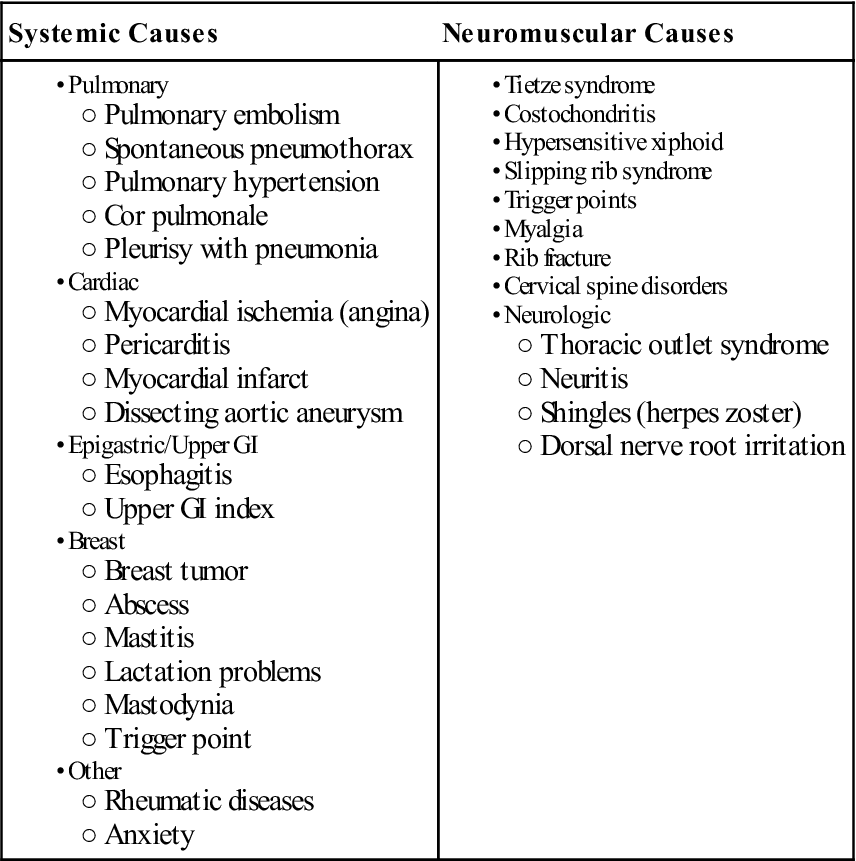
| SPECIFY: | ||||
| ________________________________________ | ||||
| SIGNATURE | ||||
| PRINT NAME:__________________________ | ||||
Some general questions can be asked initially, and these can be used to cross-reference questions asked in specific areas of assessment:29
1. Have you ever been a patient in a hospital, emergency room, or clinic?
2. Have you ever seen a physician for an injury or illness?
4. Have you ever had an operation?
5. Are you presently taking any medication or pills?
6. Do you have any allergies (to medications, insects, food, or other things)?
7. When was your last vaccination? What was the vaccination for?
8. Have you ever been unable to work or participate in exercise or sports?
9. Have you ever experienced chest pain, dyspnea, or syncope during work, exercise, or activity?
10. Have you ever had a seizure?
11. Have you ever been told you had high blood pressure?
12. Have you ever been told you had high cholesterol?
13. Do you have trouble breathing or do you cough during or after activity?
These general questions cover wide areas, and the specific parts of the assessment should corroborate the answers given to these general questions. In addition, the examiner must consider the effect of psychosocial issues on both the patient and his or her reported symptoms. Haggman et al.38 believed two questions were useful to screen for symptoms of depression:
1. During the past month, have you often been bothered by feeling down, depressed, or hopeless?
2. During the past month, have you been bothered by little interest or pleasure in doing things?
If the answer to both questions is yes, further psychological investigation may be warranted.39,40 Waddell and Main40 talked about illness behavior, a normal and reasonable behavior, which is what people do and say to communicate that they are ill. The examiner should always keep in mind the role psychosocial issues may have in anyone seeking primary care help.
The following assessment sections outline questions pertaining to specific body systems that may lead to further examination or testing and possible concerns or issues that must be dealt with if the patient is going to take part in a particular activity. The examiner may want to cover all of the systems or only those that appear pertinent to the problem.
Examination
The medical examination must be not only thorough but also applicable to the job, activity, exercise, or sport to which the person hopes to return or take part in. Health care professionals should always be alert for concealment, denial, or invention of problems on the part of the patient.
Vital Signs
The initial part of the examination is performed to establish the patient’s baseline physiological parameters and vital signs (see Chapter 1, Table 1-7), including pulse or heart rate, respiratory rate, blood pressure (systolic and diastolic), weight, and temperature (normal: 98.4° F [37° C], range: 96.5° F [35.8° C] to 99.4° F [37.4° C]). This part of the examination may be performed by any health care professional who has knowledge or an understanding of the techniques, and it is part of any primary care examination.41,42
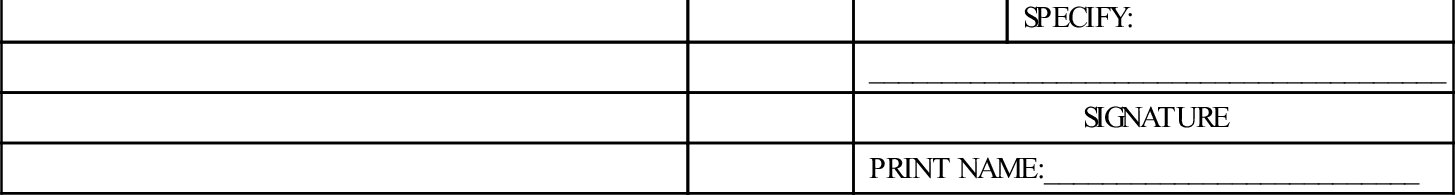
Table 1-8 (see Chapter 1) outlines guidelines for blood pressure measurement.43 High blood pressure values should be checked several times at 15- to 30-minute intervals with the patient resting in between to determine whether a high reading is accurate or is being caused by anxiety (“white coat syndrome”) or some similar reason. If three consecutive readings are high, the patient is said to have high blood pressure (hypertension) (see Chapter 1, Table 1-9). If the readings remain high, further investigation may be warranted.1,43,44 Table 17-3 outlines the risk factors of hypertension.
TABLE 17-3
| Primary | Secondary |
The following examination sections may be part of the primary care examination, but this will depend on what has been found from taking the history and vital signs. Only those sections that the examiner feels are relevant or are areas of concern would normally be investigated.
General Medical Problems
There are general systemic problems that the examiner must always keep in mind when doing an assessment. Some of the general medical (systemic) questions include the following13,27,45:
1. Have you ever been diagnosed with a systemic disease (e.g., diabetes)?
3. Have you ever been told you have cancer?
4. Have you ever had anything similar to what you have now? How often?
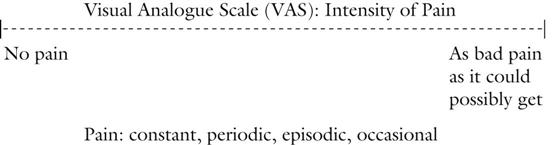
5. Where exactly is your pain? What is the quality, frequency, and pattern of the pain?46 What have you tried to do to alleviate the pain? On a scale of 1 (no pain) to 10 (pain is bad as it could possibly get), how would you rate your pain level?
6. Do you have any other symptoms?
7. Have you ever had any infections? How were they treated?
8. Do you have unexplained fatigue?
The presence of systemic disease (e.g., diabetes) does not rule out work or activity, but the examiner must ensure that there is either good control by the use of medication or that the disease will not cause undue risk to the patient or his or her well-being. It must also be determined whether the extent or intensity of the activity the patient has to do poses a significant threat to the patient’s physical condition.47 The examiner also has to be concerned about problems, such as acute infection and malignancy, and progressive diseases, such as multiple sclerosis.
Acute illnesses tend to be self-limiting and usually require only that the patient temporarily withdraw from work or activity, often to prevent spread to others.29 Dehydration is made worse by febrile illness, which could, in certain circumstances, lead to heat disorders.
Head and Face
Eye Examination
Visual acuity is usually examined with the use of a Snellen or common eye chart. Peripheral vision and depth perception may also be tested. Questions related to the eye examination include the following29,48:
1. Have you had any problems with vision or your eyes?
2. Have you ever injured your eyes?
3. Do you wear glasses, contact lenses, or protective eyewear?
5. Do you have a peripheral vision problem?
Any abnormalities found or positive answers may require further examination. Uncorrected vision of less than 20/40 should be checked further.34 Visual loss of 20/50 means that the patient can read at 20 feet what the average person can read at 50 feet. The health care professional should watch for problems that may preclude work, preclude participation in the chosen activity or sport, or affect the safety of the patient. Vision in only one eye results in lack of depth perception, which can be detrimental in certain activities. Patients with sight in only one eye should work at specific jobs or participate in physical activities only if they have an understanding of the dangers of participating and accept the risks. Such patients should not work or participate in sports for which there is no adequate eye protection.
If the patient wears glasses, the health care professional should ensure that the lenses are plastic, polycarbonate, or heat-treated (safety) glass to prevent them from shattering during work or activity.
Myopia, or nearsightedness, should be noted on the chart; such patients are more likely to suffer retinal degeneration, which increases the possibility of retinal detachment. Patients who have had a retinal detachment are sometimes excluded from contact sports or high-exertion jobs. People who have a retinal tear should be allowed to do strenuous activities only if cleared by a physician or specialist, and they should have a qualifying letter allowing them to return to work.
Pupil size should also be evaluated. In some patients, the pupils are of obvious different sizes (anisocoria). This difference should be noted in case the patient has to be evaluated for a head injury at a later date.49 Assessment of the eyes is shown in Chapter 2.
Dental Examination
Questions to be asked concerning the patient’s dental record include the following48:
1. When did you last see a dentist?
2. Have you ever had any problems with your teeth or gums?
3. Have you ever had any teeth knocked out, damaged, or extracted?
When looking for dental problems, which is usually done by a dentist, it is important to determine how many teeth the patient has and the last time he or she saw a dentist.
Ear Examination
Questions to be asked concerning the patient’s ear problems include the following:
1. Do you have any problems with hearing?
2. Do you have an earache? (What was the onset? How long is the duration?)
Ear problems are commonly referred to a physician or an ear, nose, and throat specialist. Assessment of the ear is shown in Chapter 2.
Nose Examination
Questions to be asked concerning the patient’s nose problems include the following:
1. What is the problem with your nose?
2. Can you breathe through the nose?
3. Do you have any discharge from the nose (e.g., blood, mucus)?
4. Do you use any medication through your nose (nose drops, nasal spray)?
Assessment of the nose is shown in Chapter 2. Nose problems other than colds are commonly referred to a physician.
Neurological Examination and Convulsive Disorders (Including Head Injury)
The neurological examination is very important, especially in contact or collision activities or when there is a suspected head injury. Some of the more common questions asked in the neurological examination include the following13,29:
1. Have you ever been knocked out or been unconscious?
2. Have you ever had a head injury?
3. Have you had or do you have frequent or severe headaches?
4. Have you ever had a stinger or burner?
5. Have you ever had a time when one or more of your limbs went numb or “to sleep” during activity?
6. Have you ever fainted (syncope)?
7. Have you ever had a paralyzed limb?
8. Have you ever lost feeling or muscular control of your arms or legs?
9. Have you ever had a seizure?
10. Have you ever been in a motor vehicle accident or fallen and hit your head?
A positive answer to any of these questions could have a significant impact on what the patient is allowed to do and whether the patient is allowed to return to work or participate in contact or collision activities.
In the neurological examination, the examiner may assess the status of a head injury (see Chapter 2), perform a cranial nerve assessment (see Chapter 2) and sensation scan, and evaluate the different reflexes (see Chapter 1) if problems are suspected. The examiner must check for concussions and nerve palsies. Any positive neurological signs and symptoms uncovered in the examination, such as recurrent concussions or nerve palsies, should preclude strenuous activity until investigated further by a specialist before clearance to return to previous activities is given.
With convulsive disorders, the examiner needs to know the frequency of the episodes; how or whether control of the convulsions has been achieved; the use of routine medication; any circumstances that activate the convulsions; and whether the patient understands the disorder, its hazards, and its predisposing factors. Patients with epilepsy should be discouraged from activities, such as skiing, scuba diving, parachuting, and climbing, because of their inherent dangers.29 If the activity involves water sports (e.g., swimming alone, scuba diving), auto racing, or any activity in which recurrent head trauma or unexpected falls may cause serious injury (e.g., mountain climbing, working at heights), then the patient with convulsive disorders should be discouraged from doing these activities. Patients whose activities should be restricted include those who experience daily or weekly seizures, those who display bizarre forms of psychomotor epilepsy, and those whose postconvalescent state is prolonged or typically includes marked abnormal behavior. It is important to understand whether the medication taken can maintain good control of the patient’s condition, not only in everyday situations but also in stress situations. For example, hyperventilation may precipitate an epileptic seizure, and seizures tend to occur after exercise, not during the event. In addition, it is important to know whether the extent or intensity of the participation poses a significant threat to the patient’s physical condition.
Musculoskeletal Examination
Like the neurological examination discussed previously, the musculoskeletal examination is often a very important part of an evaluation. Questions in the history related to this examination include the following31,50–54:
1. Have you ever pulled (strained) or hurt a muscle?
2. Have you ever torn (sprained) or stretched a ligament?
3. Have you ever subluxated or dislocated a joint or had a bone come out of joint?
4. Have you ever broken (fractured) a bone?
5. Have any of your joints ever swollen?
6. Have you ever had pain in the muscles or joints at work or during or after activity, exercise, or sports (Table 17-4)?
7. Have you ever had regular prolonged (more than 30 minutes) morning stiffness?
8. Have you ever had any rashes, eye infections, diarrhea associated with joint pains, and/or swelling?
9. Have you ever had any proximal weakness, excessive cramping, or muscle fasciculations?
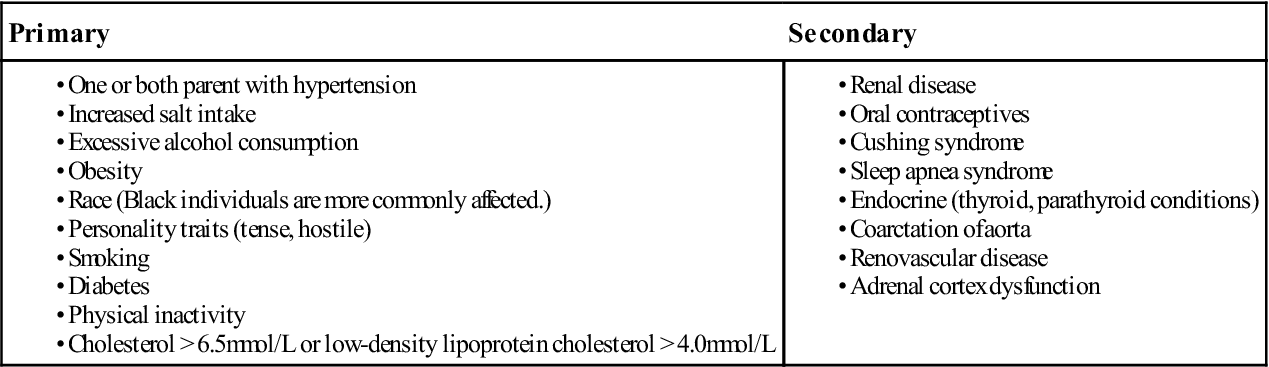
TABLE 17-4
Comparison of Systemic and Musculoskeletal Joint Pain
| Systemic | Musculoskeletal |
From Goodman CC, Snyder TE: Differential diagnosis in physical therapy, Philadelphia, 1995, WB Saunders, p. 526.
A positive response to any of these questions requires further investigation.
The musculoskeletal examination begins with observation of the patient’s posture (see Chapter 15), looking for any asymmetry. Asymmetry, combined with the history, may lead the examiner to do a detailed assessment of a specific joint (see Chapters 3 to 13). If no problems are noted, the examiner can do a quick upper and lower scanning or screening examination to check for potential problems and abnormal movement (e.g., hypomobility, hypermobility, capsular patterns, weakness, abnormal movement patterns, cheating movements).41,55
If any deviation, weakness, or abnormality is found, or if the patient has reported a previous injury to a joint, a more detailed examination may be performed to assess active movements, passive movements, resisted isometric movements, special tests, functional tests, reflexes, sensation, myotomes, joint play, and palpation of that joint or associated joints.
When looking for musculoskeletal problems, it is important to consider whether the patient’s job or what he or she wants to do will exacerbate an existing disease or injury, increase an existing deformity, or cause further bone or joint damage. When looking for musculoskeletal problems, the examiner may look at the patient’s flexibility, strength, and endurance, as well as static and dynamic stability. Spinal instability (especially instability of the cervical or lumbar spine) or spondylolisthesis may preclude the patient from taking part in some activities. Maturation may also have to be considered when dealing with patients who are still growing, as may previous injuries, congenital problems, and growth abnormalities.
Cardiovascular Examination
The cardiovascular examination should be performed in a quiet area because of the need to auscultate. In this part of the evaluation, the examiner looks for subtle but significant cardiac abnormalities to reduce the incidence of unexpected sudden death in sports or similar incidences at work.2,32,56–61 In some cases, electrocardiograms (ECGs) or stress ECGs may be appropriate.62 More than 90% of sudden deaths in exercise and sports among participants younger than 30 years of age involve the cardiovascular system.
The following questions should be asked in the history concerning the cardiovascular system9,13,27,29:
1. Have you ever had a heart attack?
2. Do you have a pacemaker or other device to assist your heart?
3. Have you ever had heart surgery?
4. Have you ever had frequent heartburn?
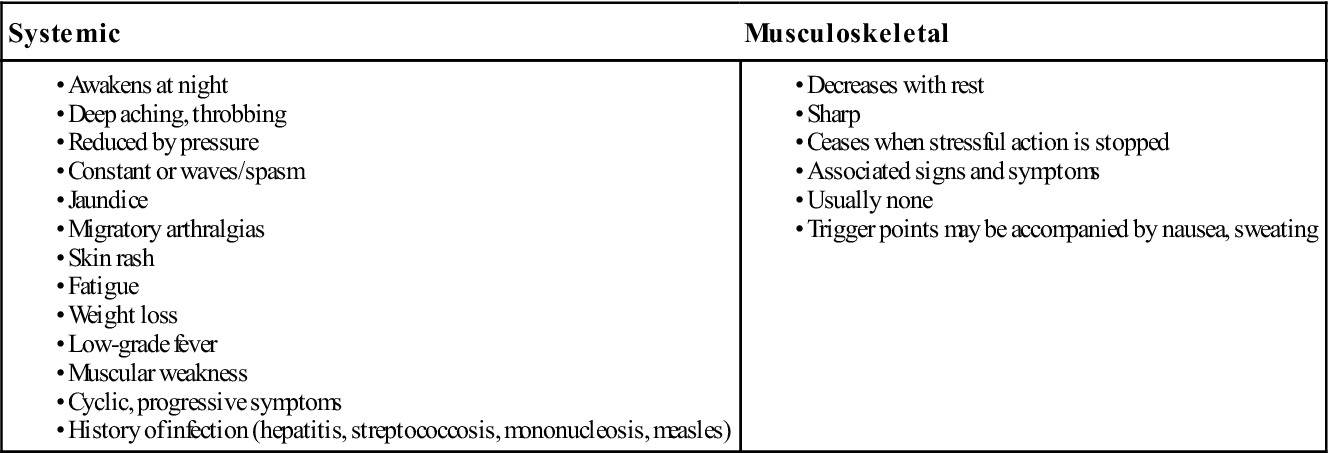
6. Have you ever experienced chest pain, tightness, crushing sensation, squeezing, or pressure in the chest at work or during or after activity, exercise, or sports (Table 17-5 and 17-6)?
8. Have you ever had high blood pressure?
9. Has your heart ever “raced” or skipped beats?
10. Have you ever been told you have a heart murmur?
11. Has anyone in your family ever had or died from heart problems?
12. Has anyone in your family died suddenly before the age of 50 years?
13. Have you had a severe viral infection (myocarditis, mononucleosis) within the last month?
14. Has a physician denied or restricted your participation in any activity for any heart problems?
TABLE 17-5
| Systemic Causes | Neuromuscular Causes |
From Goodman CC, Snyder TE: Differential diagnosis in physical therapy, Philadelphia, 1995, WB Saunders, p. 532.
TABLE 17-6
Characteristics of Cardiac Chest Pain
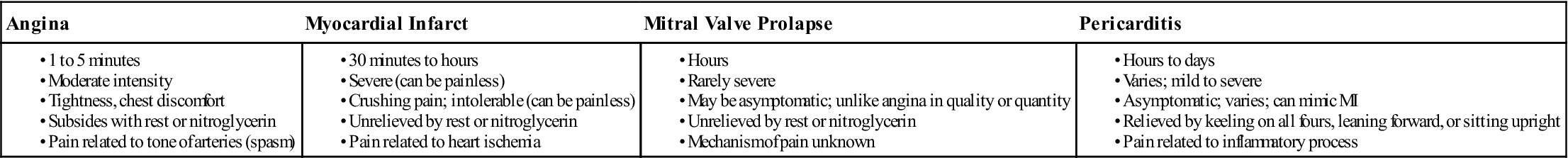
From Goodman CC, Snyder TE: Differential diagnosis in physical therapy, Philadelphia, 1995, WB Saunders, p. 94.
If the answer to any of these questions is yes, the examiner must consider the possibility of cardiomyopathy, conduction abnormalities, arrhythmias, valvular problems, coronary artery defects, and lung or related problems.64 If cardiovascular problems are suspected, the examiner may organize further tests (e.g., ECG, treadmill stress tests, laboratory tests)65 to detect cardiac abnormalities.
When looking for cardiovascular problems, the examiner should be alert for the following unusual or abnormal findings:
1. Heart rate faster than 120 beats/min or inappropriate tachycardia for a specific activity
2. Arrhythmias or irregular beats66
3. Midsystolic clicks, indicating a leaky valve or mitral valve prolapse
The loudness of systolic murmurs is graded from 1 to 6 with grade 1 being a very faint murmur requiring concentration to be heard. A grade 2 murmur is a faint murmur but one that is heard immediately after the stethoscope is placed on the chest. Grade 3 is an intermediate murmur louder than grade 2. Most human dynamically significant murmurs are at least grade 3. Grade 4 is a loud murmur, frequently associated with palpable sensation, known as a thrill. A grade 5 murmur is a very loud murmur still requiring at least the edge of the stethoscope to remain in contact with the chest. The grade 6 murmur is a murmur audible with the stethoscope just breaking contact with the chest.67 Diastolic murmurs are graded from 1 to 4, 1 representing the faintest and 4 the loudest murmur. A benign functional murmur or systemic mitral valve prolapse does not preclude exercise or sports but must be evaluated on an individual basis.
The examiner must be aware of congenital heart abnormalities, such as aortic coarctation (stenosis of the artery), which may be revealed by a difference in the femoral and brachial pulses. In such a case, strenuous activity is contraindicated. As another example, 90% of patients with Marfan syndrome (an autosomal dominant condition) have cardiac abnormalities. The examiner must be aware of atrial septal defects (an abnormal communication between the chambers of the heart), dextrocardia (the heart is moved within the thoracic cavity), and paroxysmal auricular tachycardia (an abnormal increase in heartbeat for short periods). Patients with these conditions should be cleared by a specialist before any strenuous activity because of the possibility of fainting in a stressful situation. The examiner must also be aware of heart enlargement (athlete’s heart). This condition does not necessarily preclude activity but should be investigated further if found. If any of these abnormalities have been surgically corrected, they should be evaluated by a specialist on an individual basis to determine whether the patient can take part in the proposed activity.
Hypertrophic cardiomyopathy is the most common cause of sudden death in athletes, followed by aortic rupture associated with Marfan syndrome, congenital coronary artery anomalies, and atherosclerotic coronary artery disease.29,68 If any of these conditions is present, strenuous activity is precluded.
Other cardiovascular problems include thromboembolic disease, pulse irregularities, valvular problems (such as, mitral insufficiency or mitral valve prolapse), and abnormally high blood pressure (hypertension). Systolic pressure of 140 mm Hg on repeated measurements is considered abnormal (see Chapter 1, Table 1-9).58 Also, patients with labile hypertension (an unstable condition of free and rapid change in tension) or organic hypertension caused by structural problems should be investigated further. These patients should have a complete comprehensive coronary risk factor work-up. Mild hypertension does not preclude strenuous activity, but this slight abnormality should be noted and evaluated on an individual basis.29 When taking blood pressure, a proper cuff size must be used to ensure an accurate reading. If the initial reading is high, the reading should be repeated two or three times after the patient has been lying supine for 20 to 30 minutes. Only if the blood pressure is elevated after the third reading should the patient be considered hypertensive.