44
Precipitate labour and slow labour
Introduction
Abnormal uterine activity has no clear definition, partly because the range of normal uterine activity itself has no clear definition. It is tempting to refer to uterine ‘overactivity’ as that which results in labour progressing too quickly, and ‘inadequate’ uterine activity as that which is insufficient to provide adequate progress, but the rate of progress has no precise definition either and is dependent on parity. In practice, overactivity presents as rapid painful contractions often associated with fetal distress, and inadequate uterine activity as absent or slow cervical dilatation.
Precipitate labour has been defined as expulsion of the fetus within less than 3 h of the onset of contractions and results from uterine overactivity. Slow labour may result from inadequate uterine activity, cephalopelvic disproportion, or more commonly, a combination of the two.
Cephalopelvic disproportion refers to how well the fetal head fits through the pelvis and may occur if the fetal head is too big or the pelvis too small. It is subdivided into ‘true’ cephalopelvic disproportion if the head is in the correct position and ‘relative’ cephalopelvic disproportion if the obstruction is caused by the head presenting in a position other than occipitoanterior.
Precipitate labour
Spontaneous hypercontractility is rare, perhaps occurring in only 1:3000 pregnancies. The contractions may be excessively long in duration or be excessively frequent and there is a risk of fetal hypoxia due to interference with the placental blood supply. Spontaneous uterine hypercontractility may be associated with placental abruption (see p. 278).
Uterine hyperstimulation occurs much more commonly, however, and by definition is caused by the use of oxytocics. Both syntocinon (synthetic oxytocin that is administered by injection or infusion) and prostaglandins may be implicated. The choice of dosage regimens for each represents a compromise between efficacy and the risk of hyperstimulation. The appropriate dose of syntocinon remains controversial, but there is good evidence for starting at a low dose, around 0.5–4 mU/min, and increasing over 4 or 5 h to 12 mU/min. While the licensed maximum dose is currently 20 mU/min, some clinicians support the use of regimens up to 40 mU/min.
With prostaglandins, hyperstimulation is also a significant risk but is less likely if their administration is intravaginal, rather than oral, intracervical or directly extra-amniotic.
Precipitate labour resulting from either spontaneous hypercontractility or uterine hyperstimulation may lead to fetal distress. Placental blood supply is via intramyometrial blood vessels which are constricted during the contraction, and excessively long or frequent contractions reduce the chance of recovery in the short times when blood flow is returned (Fig. 44.1). Precipitate labour may also predispose to uterine rupture in parous women, particularly if there is a pre-existing caesarean section scar.
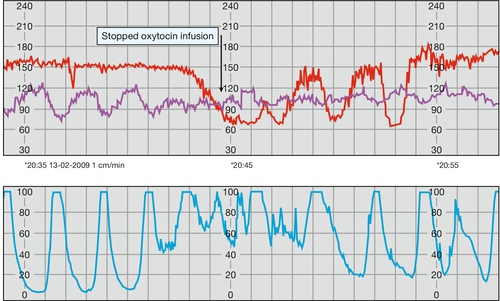
Fig. 44.1Cardiotocograph trace in precipitate labour.
There is hyperstimulation secondary to syntocinon administration. When the syntocinon is stopped, the contractions become less frequent and the CTG improves.
Management of precipitate labour is largely dependent on the fetal condition. If a syntocinon infusion is running, it should be stopped and the mother given a tocolytic, e.g. a bolus of subcutaneous terbutaline or intravenous ritodrine. If severe fetal distress is apparent, it may be necessary to deliver the baby either instrumentally or by caesarean section, depending on the dilatation of the cervix. If a caesarean section is arranged, it is worth carrying out a vaginal examination prior to starting the operation, as the cervix may dilate rapidly during the time taken in the transfer to theatre, especially in a parous woman.
Precipitate labour is associated with complications for the mother including: cervical and perineal tears, retained placenta, postpartum haemorrhage and the need for a blood transfusion.
As mentioned above, it is important to remember that frequent uterine contractions are also a feature of placental abruption. Contractions with a frequency of more than one every 2 min are highly suggestive of this problem and these frequent contractions may increase the distress of a fetus already compromised by partial placental separation. The diagnosis of placental abruption is even more likely if there is associated lower abdominal pain, backache or vaginal bleeding. As a general rule, tocolytic drugs should not be used to manage the uterine hypercontractility associated with placental abruption, as uterine relaxation may exacerbate the bleeding and precipitate further placental separation.
Slow labour
Slow progress in labour is usually diagnosed by assessing the rate of cervical dilatation. As discussed on page 328 and 351, progress can be monitored on a partogram and alert lines can be used to identify women who are progressing slowly. Early identification and correction of abnormal labour makes it more likely that the mother will achieve a vaginal delivery. Unfortunately the definition of slow labour is controversial; traditional obstetric practice suggested that any nulliparous woman with a rate of cervical dilatation less than 1 cm/h required treatment for slow progress. More recently, a rate of cervical dilatation of < 0.5 cm/h has been adopted as the threshold.
Slow labour is associated with:
![]() eventual fetal ‘distress’ and risk of fetal hypoxic injury
eventual fetal ‘distress’ and risk of fetal hypoxic injury
![]() an increased risk of intrauterine infection leading to fetal and maternal morbidity
an increased risk of intrauterine infection leading to fetal and maternal morbidity
![]() maternal anxiety and longer-term ‘psychological’ scarring
maternal anxiety and longer-term ‘psychological’ scarring
![]() a loss of confidence in those providing maternity care.
a loss of confidence in those providing maternity care.
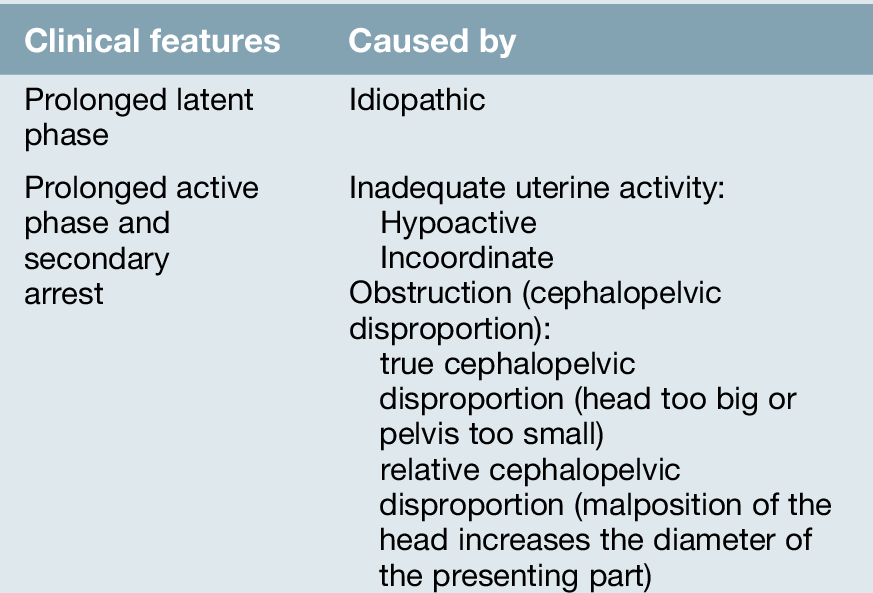
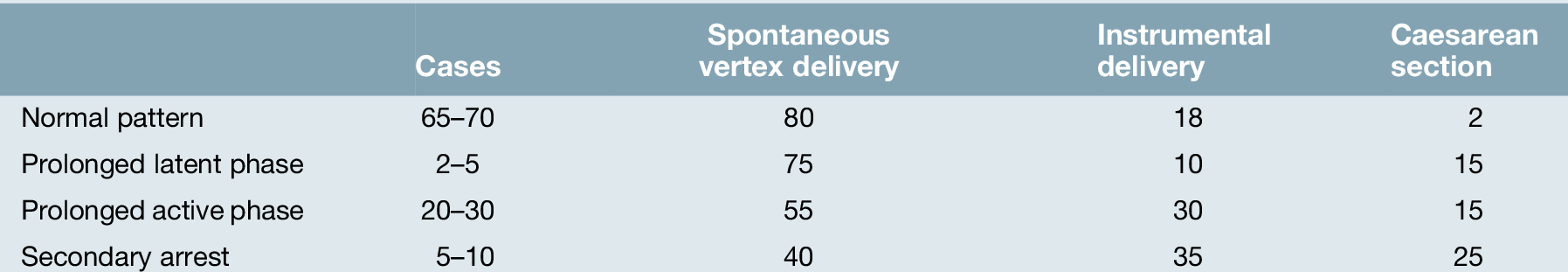
These in turn are associated with a greater chance of the mother being delivered by caesarean section or requiring an instrumental delivery. The causes of slow labour are summarized in Table 44.1 and the outcome in Table 44.2.
Prolonged latent phase
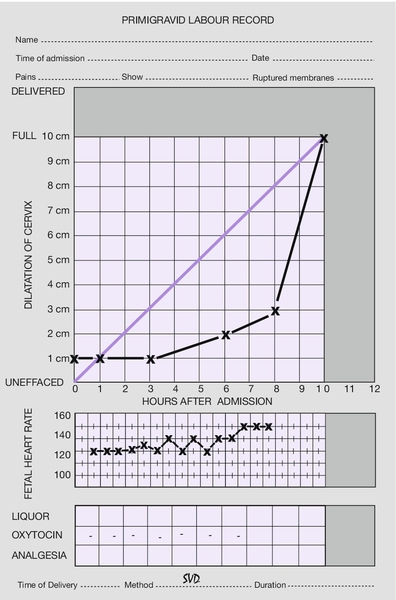
Chapter 40 describes how the first stage of labour is divided into two parts: the latent phase (from the onset of contractions until the cervix is fully effaced) and the active phase (when the cervix begins to dilate). The latent phase is most likely to be prolonged in those whose cervix is unfavourable, and a prolonged latent phase is therefore much more common in primigravidae (Fig. 44.2).
There is rarely any serious cause for a prolonged latent phase. Cephalopelvic disproportion usually presents at more advanced stages of cervical dilatation. Only very rarely are the symptoms mimicked by dehiscence of a previous caesarean section scar. With a prolonged latent phase, the mother often becomes weary, exhausted and demoralized from what can sometimes be discomfort over a number of days. Within reason, it is important to resist the temptation to actively intervene by artificially rupturing the membranes or administering oxytocics, at least until the cervix is 2 or 3 cm dilated and fully effaced with a well-applied presenting part. These measures may actually increase the risk of further obstetric intervention in what might, with patience, have been an uneventful labour. Reassurance, encouragement and appropriate analgesia over this time are extremely important.
Prolonged active phase and secondary arrest
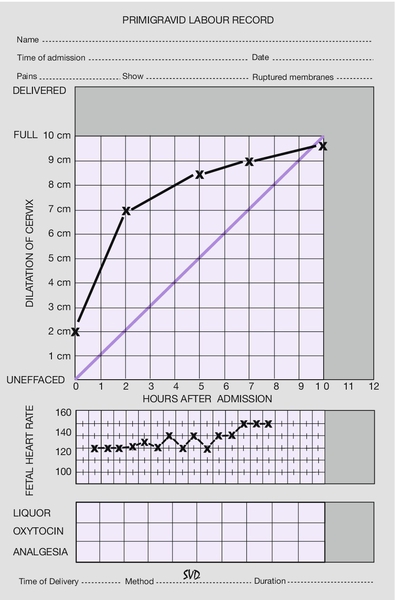
The active phase may be prolonged because of inadequate uterine activity or cephalopelvic disproportion (Fig. 44.3).
Inadequate uterine activity
The uterus may be hypoactive or incoordinate. A hypoactive uterus is one with low resting tone and only weakly propagated contractions. There is often a longer interval between contractions and the contractions are not particularly painful.
Incoordinate uterine activity may occur because of inadequate ‘fundal dominance’. Normal uterine contraction begins at a pacemaker point close to the junction of the uterus and the fallopian tube. It spreads from this point downwards, with its intensity maximal at the fundus (where the muscle is thickest), intermediate at the mid-zone and least at the lower segment. Uterine contractions can be described in terms of baseline tone, amplitude, frequency and duration. With incoordinate uterine activity, the intensity profile appears to be reversed, with the maximal intensity in the lower segment (where the muscle is thinnest) and weakest at the fundus. This is much less efficient. The resting tone is increased throughout and the threshold for pain is therefore reached earlier in the contraction. Incoordinate uterine activity is common, especially in women in their first labour. Contractions may be incoordinate in terms of frequency or duration/strength or a combination of both.
Inadequate uterine activity has no specific cause. It may simply be a developmental feature of the uterine muscle and there is evidence that many will resolve spontaneously given sufficient time. There is also some evidence that inadequate uterine activity is associated with cephalopelvic disproportion. This is because cervical dilatation itself may improve uterine activity, but is less likely to occur if the presenting part is pressing less firmly on the cervix.
If progress is satisfactory, there is no need to consider treatment of incoordinate uterine activity. Most will respond well to oxytocics, usually given by a stepwise i.v. syntocinon infusion as described above. As labour is likely to be prolonged, care should be taken to make sure that the mother does not become dehydrated or ketotic, as this will further exacerbate the uterine problem.
Cephalopelvic disproportion (CPD)
This may occur because:
1. The baby’s head is presenting in the optimal way but is too large relative to the pelvis (‘true’ cephalopelvic disproportion). It is diagnosed only if the head does not become engaged despite adequate uterine activity. It is not possible to predict CPD antenatally and even using the strictest antenatal criteria many of those considered to be at risk by clinical pelvic assessment will go on to have a vaginal delivery. More complicated attempts to predict CPD using ultrasound measurements of the fetal head together with X-ray or CT pelvimetry measurements have also proved to be unreliable and only lead to unnecessary surgical intervention. Short maternal stature or small shoe size are not predictive of CPD. The only true test is labour itself.
2. There is a malpresentation or malposition of the baby’s head so that a wider part of the head is being presented to the pelvis. This is ‘relative’ cephalopelvic disproportion. It may occur with deflexed malpresentations (particularly of the brow and face, p. 355) but the most common cause of relative CPD occurs when the head rotates to the occipito-posterior (p. 363) rather than the occipito-anterior position. The first stage and second stage progress more slowly and, although spontaneous delivery is quite possible with the head coming out ‘face to pubis’, secondary arrest is not uncommon.
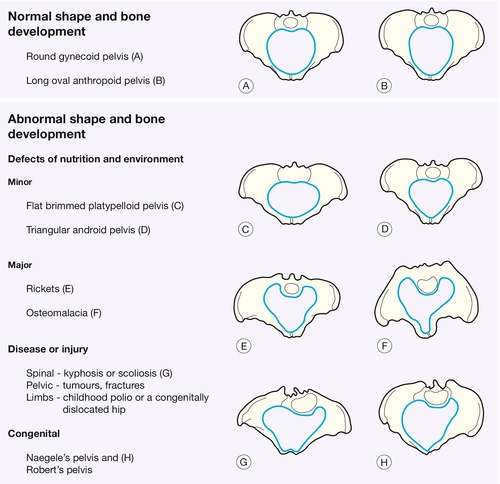
3. There is some form of pelvic abnormality. Major abnormalities are uncommon, particularly in affluent societies, and are usually associated with disease, injury or severe nutritional problems. The obstetric classification is based on the shape of the pelvic brim, as it is the pelvic inlet, which seems to be the major determinant of successful delivery (Fig. 44.4).
Pelves with normal shape and bone development
The round ‘gynaecoid’ pelvis is the commonest and, as would be teleologically predicted by the theory of natural selection; it is obstetrically ideal. The long oval ‘anthropoid’ pelvis is also relatively common but is associated with occipitoposterior presentation.
Pelves with abnormal shape and bone development
Defects of nutrition and environment
Minor
The flat-brimmed ‘platypelloid’ pelvis and the triangular ‘android’ pelvis are considered to be minor variations associated with adverse nutrition in infancy and childhood. The flat-brimmed pelvis is found relatively more commonly in African women and the triangular pelvis in those from southern Europe.
Major
Rickets is caused by prolonged vitamin D deficiency in early life leading to poorly mineralized bones containing large areas of soft uncalcified osteoid. Weight bearing produces bony deformities by pushing the sacral promontory forward and pivoting the sacrum backwards. The result is a marked reduction in the anteroposterior measurement of the pelvic brim, with possible further mid-cavity narrowing in severe cases as the acetabula are also forced inwards. As the diet in many western countries contains adequate calcium and vitamin D, and many ‘developing’ countries have plenty of exposure to sunshine, rickets is uncommon. Osteomalacia – caused by adult calcium deficiency – is rare, except in certain parts of northern India and China.
Disease or injury
Abnormal pressure on the pelvis from kyphosis or scoliosis gradually moulds the pelvis into funnelled or asymmetric shapes. Asymmetrical weight bearing from polio or a congenitally dislocated hip may also mould the pelvis to less favourable proportions. Pelvic fractures may leave the pelvis asymmetrical, and excessive bone formation at the fracture site may further narrow the passage.
Congenital malformations
Congenital absence of one or both sacral masses (Naegele’s pelvis and Robert’s pelvis, respectively) results in direct fusion of the sacrum to the ilium and marked narrowing.
Management of slow labour
When progress is slow or when there is secondary arrest, it is important to distinguish whether the cause is inadequate uterine activity or cephalopelvic disproportion.
The strength of contractions is difficult to assess reliably and cannot be done from a cardiotocograph recording. Direct intrauterine pressure monitoring using a pressure catheter is essentially only a research tool and is rarely, if ever, used in clinical practice. Some idea of the strength can be gained through maternal observation and abdominal palpation of contractions. The examining hand is placed between the umbilicus and the uterine fundus and the duration and frequency of the uterine contractions is assessed over a 10 min period. With an experienced observer, this can provide useful clinical information. In the presence of cephalopelvic disproportion there will be caput (a diffuse swelling of the scalp) and moulding (an alteration in the relation of the fetal cranial bones), and malposition or malpresentation may be identified by careful vaginal examination.
In practice, the clinical decision is whether or not to start a syntocinon infusion. The main risks of starting syntocinon are of:
![]() hyperstimulation of the uterus and subsequent fetal distress
hyperstimulation of the uterus and subsequent fetal distress
![]() rupture of the uterus (this applies almost exclusively to multiparous mothers and is more likely in those with a previous caesarean section scar).
rupture of the uterus (this applies almost exclusively to multiparous mothers and is more likely in those with a previous caesarean section scar).
In primigravidae with slow progress or secondary arrest who do not have a prohibitive malpresentation (e.g. brow presentation) it is reasonable to start syntocinon. This is not appropriate if there is suspected fetal distress and should only be after the membranes have been ruptured or have ruptured spontaneously. The aim is to titrate the infusion to the point where the contractions are coming at a frequency of three or four every 10 min. Vaginal examinations should be repeated every 3–4 h after the infusion is started, to ensure adequate progress. If progress is still inadequate, then operative delivery will be required.
In parous women, the decision is more difficult, mainly because of the risk of uterine rupture (p. 376). Rupture can occur suddenly and leads to expulsion of the fetus into the peritoneal cavity. In this situation, fetal hypoxia and death is not uncommon. If the mother has had a previous vaginal delivery, true cephalopelvic disproportion is extremely unlikely, but if the only previous delivery was an elective caesarean section (e.g. for breech presentation), there is no guide to the likelihood of true obstruction. Syntocinon should therefore be used only with caution and only in those women thought to have inadequate uterine activity with no evidence of obstruction. Vaginal examinations should again be repeated every 3–4 h to ensure adequate progress, with a lower threshold for caesarean section in those thought to have some degree of cephalopelvic disproportion.