25 Posttraumatic Stress Disorder
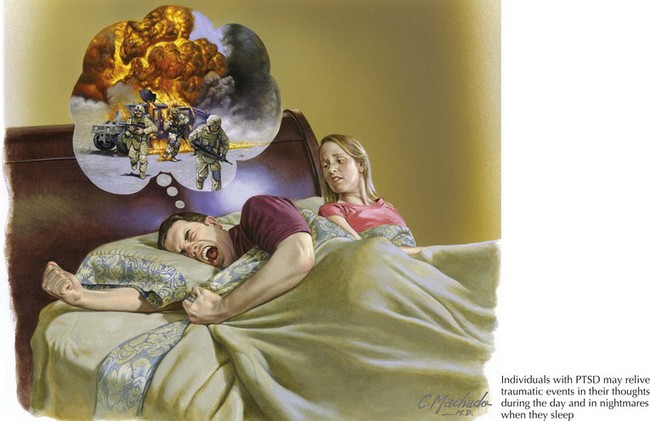
PTSD—initially described as “shell-shock” or “combat fatigue” —was first recognized in military veterans at least as early as World War I, when it was referred to as neurasthenia, a term that previously had a broader definition encompassing civilian as well as military experiences. In earlier versions of the Diagnostic and Statistical Manual of Mental Disorders (DSM), one could only diagnose PTSD in individuals who had suffered trauma “outside the range of usual human experience” (Fig. 25-1). However, as lesser traumas can trigger the syndrome in susceptible individuals, PTSD is relatively common, with a lifetime prevalence in the United States of 8%.
Aerni A, Traber R, Hock C, et al. Low-dose cortisol for symptoms of posttraumatic stress disorder. Am J Psychiatry. 2004 Aug;161(8):1488-1490.
Davidson JRT, Rothbaum BO, van der Kolk BA, et al. Multicenter, double-blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Arch Gen Psychiatry. 2001;58:485-492.
Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048-1060.
Koenen KC, Moffitt TE, Poulton R, et al. Early childhood factors associated with the development of post-traumatic stress disorder: results from a longitudinal birth cohort. Psychol Med. 2007;37:181-192.
McNally RJ. Psychological debriefing does not prevent posttraumatic stress disorder. Psychiatric Times. April 1, 2004. Vol. 21 No. 4
Ozer EJ, Best SR, Lipsey TL, et al. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129:52-73.
Pitman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol. Am J Psychiatry. 2004 Aug;161(8):1488-1490.
Raskind MA, Peskind ER, Hoff DJ, et al. A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with post-traumatic stress disorder. Biol Psychiatry. 2007 Apr 15;61(8):928-934.