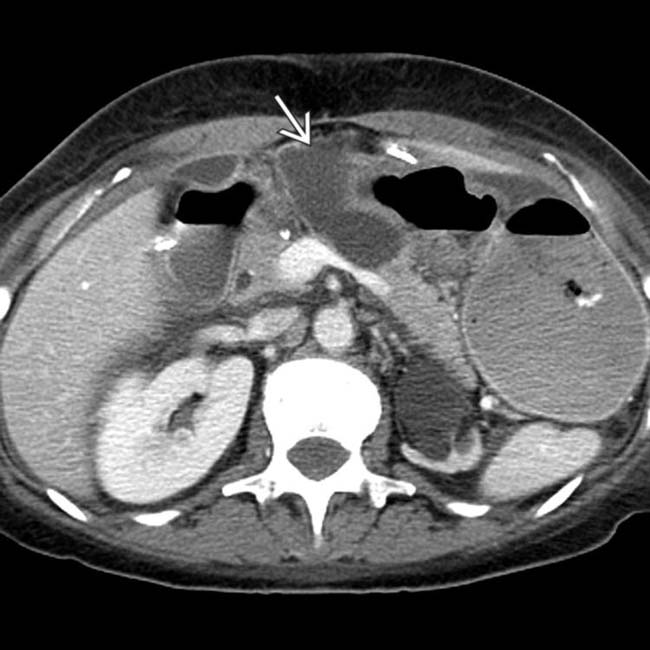
Small free fluid, edema, and fat stranding in surgical bed with reactive subcentimeter lymph nodes in mesentery
 Mild biliary dilatation, gastrojejunostomy thickening, and pancreatic duct dilatation due to anastomotic edema
Mild biliary dilatation, gastrojejunostomy thickening, and pancreatic duct dilatation due to anastomotic edema Pancreatic duct stent (thin linear radiodensity) often placed during surgery (traversing pancreaticojejunostomy) to ↓ risk of pancreatic fistula
Pancreatic duct stent (thin linear radiodensity) often placed during surgery (traversing pancreaticojejunostomy) to ↓ risk of pancreatic fistula• Common complications
 Abscess: Can be intrahepatic, in pancreatic bed, or in subphrenic, subhepatic, or retroperitoneal spaces
Abscess: Can be intrahepatic, in pancreatic bed, or in subphrenic, subhepatic, or retroperitoneal spaces
 Gastrojejunostomy and hepaticojejunostomy leaks: Suspect when focal fluid collection or ectopic gas in close contiguity to anastomosis
Gastrojejunostomy and hepaticojejunostomy leaks: Suspect when focal fluid collection or ectopic gas in close contiguity to anastomosis
 Postoperative hemorrhage: May be due to bleeding from gastroduodenal artery stump or due to structural abnormality (e.g., pseudoaneurysm)
Postoperative hemorrhage: May be due to bleeding from gastroduodenal artery stump or due to structural abnormality (e.g., pseudoaneurysm)
 Anastomotic strictures: Suspect when progressive biliary or pancreatic ductal dilatation without obstructing tumor at anastomotic site
Anastomotic strictures: Suspect when progressive biliary or pancreatic ductal dilatation without obstructing tumor at anastomotic site
 Abscess: Can be intrahepatic, in pancreatic bed, or in subphrenic, subhepatic, or retroperitoneal spaces
Abscess: Can be intrahepatic, in pancreatic bed, or in subphrenic, subhepatic, or retroperitoneal spaces Gastrojejunostomy and hepaticojejunostomy leaks: Suspect when focal fluid collection or ectopic gas in close contiguity to anastomosis
Gastrojejunostomy and hepaticojejunostomy leaks: Suspect when focal fluid collection or ectopic gas in close contiguity to anastomosis Postoperative hemorrhage: May be due to bleeding from gastroduodenal artery stump or due to structural abnormality (e.g., pseudoaneurysm)
Postoperative hemorrhage: May be due to bleeding from gastroduodenal artery stump or due to structural abnormality (e.g., pseudoaneurysm) Anastomotic strictures: Suspect when progressive biliary or pancreatic ductal dilatation without obstructing tumor at anastomotic site
Anastomotic strictures: Suspect when progressive biliary or pancreatic ductal dilatation without obstructing tumor at anastomotic site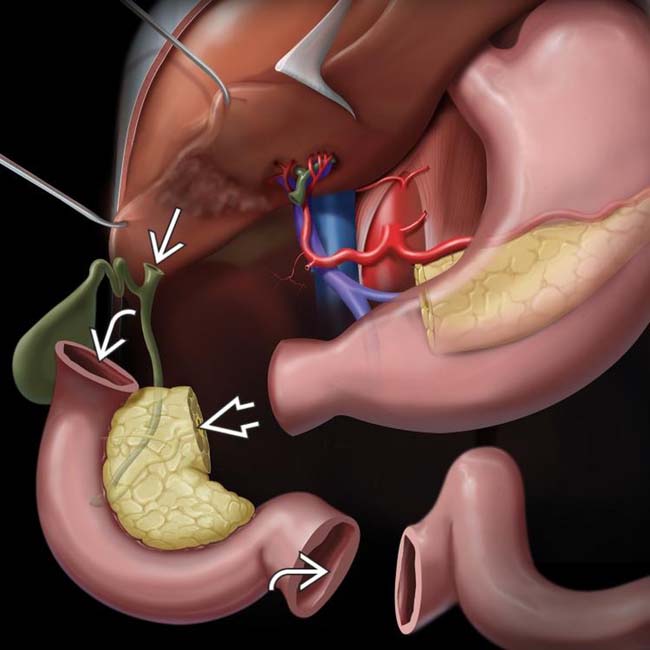
 , the pancreatic margin
, the pancreatic margin  , and the intestinal margins
, and the intestinal margins  .
.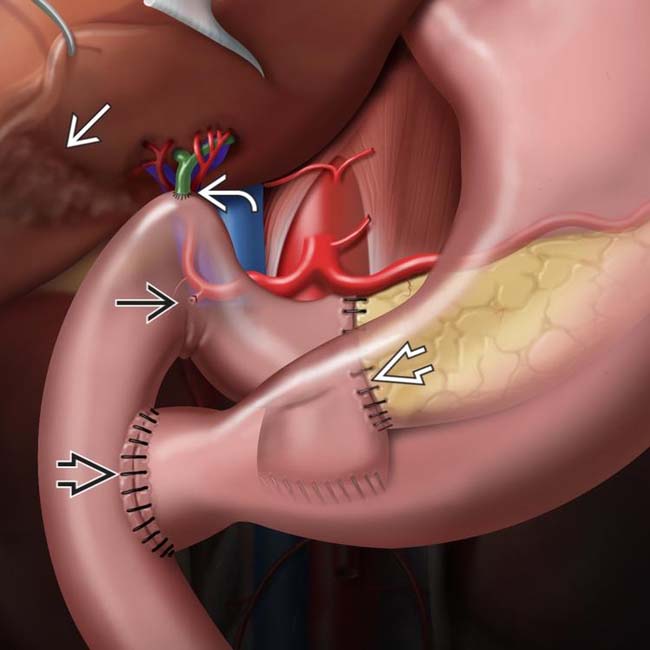
 , choledochojejunostomy
, choledochojejunostomy  , gastrojejunostomy or duodenojejunostomy
, gastrojejunostomy or duodenojejunostomy  , and cholecystectomy
, and cholecystectomy  . The pylorus may be removed or preserved, depending on extent of disease and surgeon preference. Note the ligated gastroduodenal artery
. The pylorus may be removed or preserved, depending on extent of disease and surgeon preference. Note the ligated gastroduodenal artery  .
.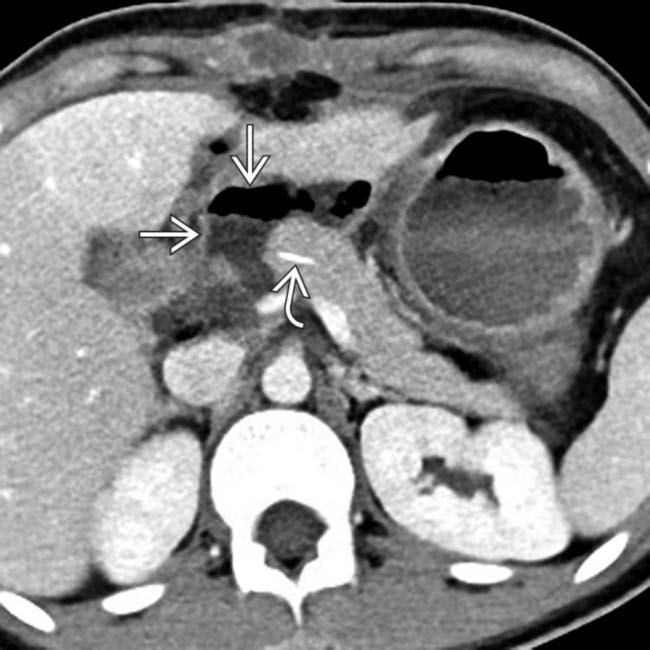
 immediately adjacent to the pancreaticojejunostomy in a patient with an elevated drain amylase, compatible with pancreatic fistula. Note the presence of a pancreatic duct stent
immediately adjacent to the pancreaticojejunostomy in a patient with an elevated drain amylase, compatible with pancreatic fistula. Note the presence of a pancreatic duct stent  .
.
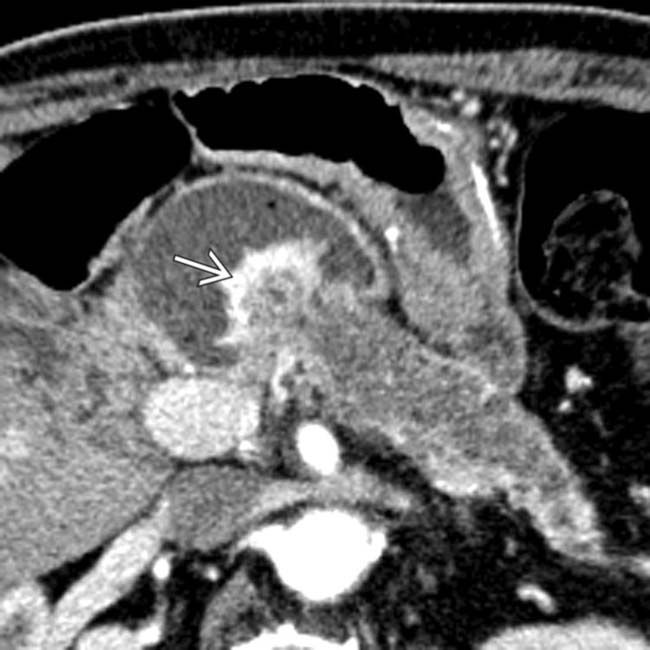
 in the right liver lobe with an internal air-fluid level, compatible with a postoperative hepatic abscess.
in the right liver lobe with an internal air-fluid level, compatible with a postoperative hepatic abscess.IMAGING
General Features
• Best diagnostic clue
• Surgical procedure determined by location and type of pathology
 Whipple procedure most commonly performed for tumors of pancreatic head, uncinate, and proximal neck
Whipple procedure most commonly performed for tumors of pancreatic head, uncinate, and proximal neck
 Central pancreatectomy performed for low-risk lesions (low malignant potential) in pancreatic neck/body
Central pancreatectomy performed for low-risk lesions (low malignant potential) in pancreatic neck/body
 Enucleation performed for lesions with low malignant potential that are small and exophytic (often utilized for insulinomas)
Enucleation performed for lesions with low malignant potential that are small and exophytic (often utilized for insulinomas)
 Whipple procedure most commonly performed for tumors of pancreatic head, uncinate, and proximal neck
Whipple procedure most commonly performed for tumors of pancreatic head, uncinate, and proximal neck
– Classic Whipple procedure (pancreaticoduodenectomy) involves surgical removal of pancreatic head, gastric antrum, proximal duodenum, and gallbladder
 Central pancreatectomy performed for low-risk lesions (low malignant potential) in pancreatic neck/body
Central pancreatectomy performed for low-risk lesions (low malignant potential) in pancreatic neck/body
 Enucleation performed for lesions with low malignant potential that are small and exophytic (often utilized for insulinomas)
Enucleation performed for lesions with low malignant potential that are small and exophytic (often utilized for insulinomas)CT Findings
• Normal findings immediately after Whipple procedure
 Small free fluid, edema, and fat stranding in surgical bed with reactive subcentimeter lymph nodes in mesentery
Small free fluid, edema, and fat stranding in surgical bed with reactive subcentimeter lymph nodes in mesentery
 Small free fluid, edema, and fat stranding in surgical bed with reactive subcentimeter lymph nodes in mesentery
Small free fluid, edema, and fat stranding in surgical bed with reactive subcentimeter lymph nodes in mesentery• Complications
 Pancreatic fistula
Pancreatic fistula
 Abscess
Abscess
 Liver infarct
Liver infarct
 Postoperative hemorrhage
Postoperative hemorrhage
 Portomesenteric venous thrombosis
Portomesenteric venous thrombosis
 Anastomotic strictures
Anastomotic strictures
 Pancreatic fistula
Pancreatic fistula
 Abscess
Abscess
 Liver infarct
Liver infarct
 Postoperative hemorrhage
Postoperative hemorrhage
– May be due to bleeding from gastroduodenal artery stump (first 24 hours after surgery) or due to structural abnormality (pseudoaneurysm, vascular erosion) usually after 5th postoperative day
 Portomesenteric venous thrombosis
Portomesenteric venous thrombosis
 Anastomotic strictures
Anastomotic strictures
CLINICAL ISSUES
Presentation
• Most common signs/symptoms
 Pancreatic fistula defined as drain fluid amylase level 3x > serum amylase level on 3rd postoperative day (or > 50 cc amylase-rich fluid from drains per day)
Pancreatic fistula defined as drain fluid amylase level 3x > serum amylase level on 3rd postoperative day (or > 50 cc amylase-rich fluid from drains per day)
 Most common delayed complications following Whipple procedure include: Anastomotic stricture at biliary (8.2% at 5 years) or pancreatic (4.6% at 5 years) anastomosis, pseudocyst formation from pancreatic leak, and delayed gastric emptying (∼ 50%)
Most common delayed complications following Whipple procedure include: Anastomotic stricture at biliary (8.2% at 5 years) or pancreatic (4.6% at 5 years) anastomosis, pseudocyst formation from pancreatic leak, and delayed gastric emptying (∼ 50%)
 Pancreatic fistula defined as drain fluid amylase level 3x > serum amylase level on 3rd postoperative day (or > 50 cc amylase-rich fluid from drains per day)
Pancreatic fistula defined as drain fluid amylase level 3x > serum amylase level on 3rd postoperative day (or > 50 cc amylase-rich fluid from drains per day)
 Most common delayed complications following Whipple procedure include: Anastomotic stricture at biliary (8.2% at 5 years) or pancreatic (4.6% at 5 years) anastomosis, pseudocyst formation from pancreatic leak, and delayed gastric emptying (∼ 50%)
Most common delayed complications following Whipple procedure include: Anastomotic stricture at biliary (8.2% at 5 years) or pancreatic (4.6% at 5 years) anastomosis, pseudocyst formation from pancreatic leak, and delayed gastric emptying (∼ 50%)
Natural History & Prognosis
• Whipple procedure morbidity and mortality have dramatically fallen
 Mortality rate was once ∼ 25%, and is now 1-3%, despite pancreatic surgeries increasingly being performed for tumors previously considered unresectable
Mortality rate was once ∼ 25%, and is now 1-3%, despite pancreatic surgeries increasingly being performed for tumors previously considered unresectable
 Mortality rate was once ∼ 25%, and is now 1-3%, despite pancreatic surgeries increasingly being performed for tumors previously considered unresectable
Mortality rate was once ∼ 25%, and is now 1-3%, despite pancreatic surgeries increasingly being performed for tumors previously considered unresectableTreatment
• Pancreatic fistulas usually treated conservatively with drainage of fluid collections, antibiotics, and parenteral nutrition (surgery only considered for large pancreaticojejunal anastomotic dehiscence)
• Postoperative fluid collections (abscess or biloma), particularly when sizeable (> 3 cm), are usually treated with percutaneous drainage

 in the porta hepatis adjacent to the hepaticojejunostomy. This was found to be the result of a hepaticojejunostomy leak, but was treated conservatively with a drain.
in the porta hepatis adjacent to the hepaticojejunostomy. This was found to be the result of a hepaticojejunostomy leak, but was treated conservatively with a drain.

 encompassing the entire left hepatic lobe, in keeping with a post-Whipple liver infarct.
encompassing the entire left hepatic lobe, in keeping with a post-Whipple liver infarct.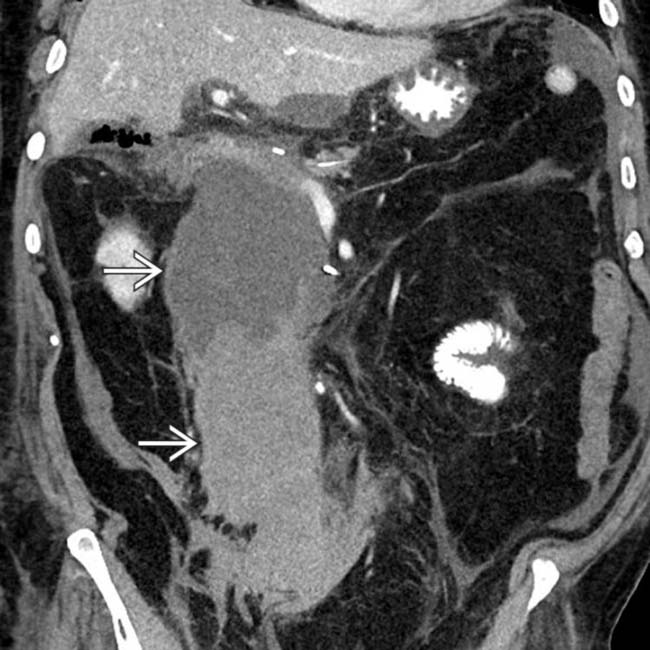
 extending from the pancreaticojejunostomy downwards into the pelvis. The patient was taken to angiography where a gastroduodenal artery (GDA) stump bleed was identified and treated.
extending from the pancreaticojejunostomy downwards into the pelvis. The patient was taken to angiography where a gastroduodenal artery (GDA) stump bleed was identified and treated.
 . The patient was taken to angiography where a vascular erosion was found to be the cause of the bleed. Post-Whipple bleeds can be either intraluminal or in the surgical bed.
. The patient was taken to angiography where a vascular erosion was found to be the cause of the bleed. Post-Whipple bleeds can be either intraluminal or in the surgical bed.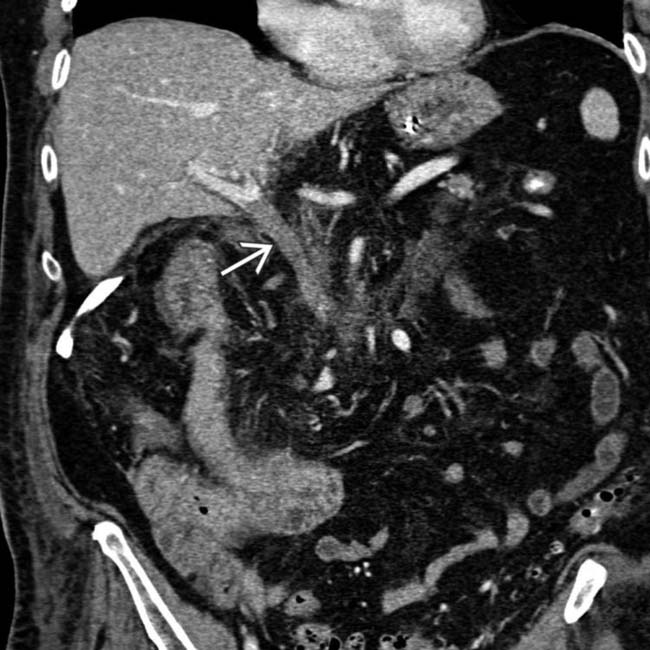
 . The patient was treated with systemic anticoagulation.
. The patient was treated with systemic anticoagulation.

 between the gastric remnant and a collection of gas in the anterior abdominal wall.
between the gastric remnant and a collection of gas in the anterior abdominal wall.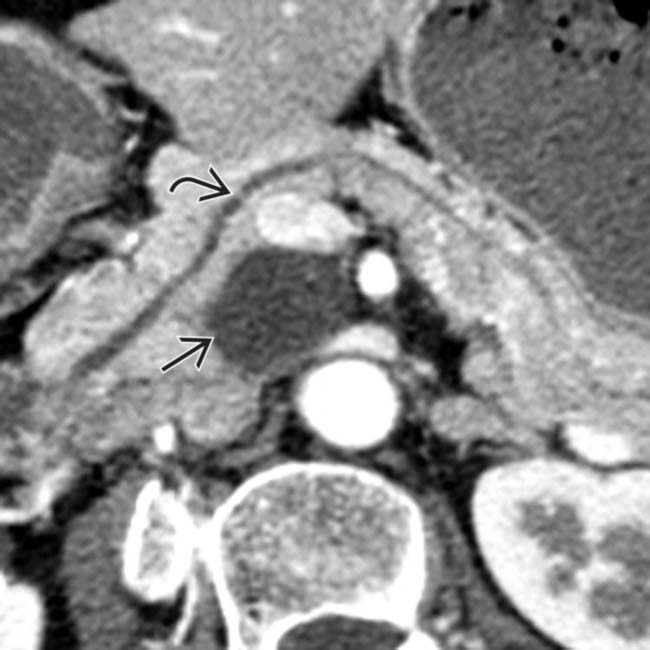
 shows a cystic mass
shows a cystic mass  in the uncinate process that was found at surgery to be a benign side-branch IPMN.
in the uncinate process that was found at surgery to be a benign side-branch IPMN.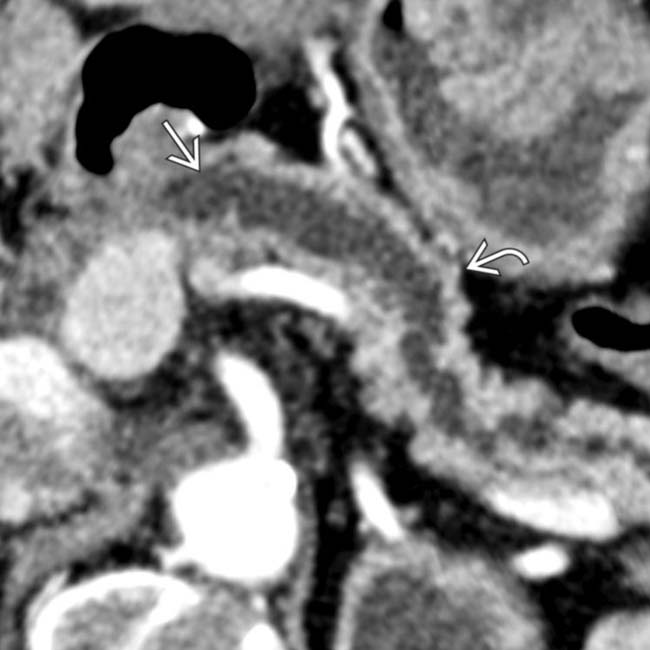
 from a stricture at the pancreatic ductal anastomosis. Note the pancreatic parenchymal atrophy
from a stricture at the pancreatic ductal anastomosis. Note the pancreatic parenchymal atrophy  accounting for the patient’s abnormal glucose levels.
accounting for the patient’s abnormal glucose levels.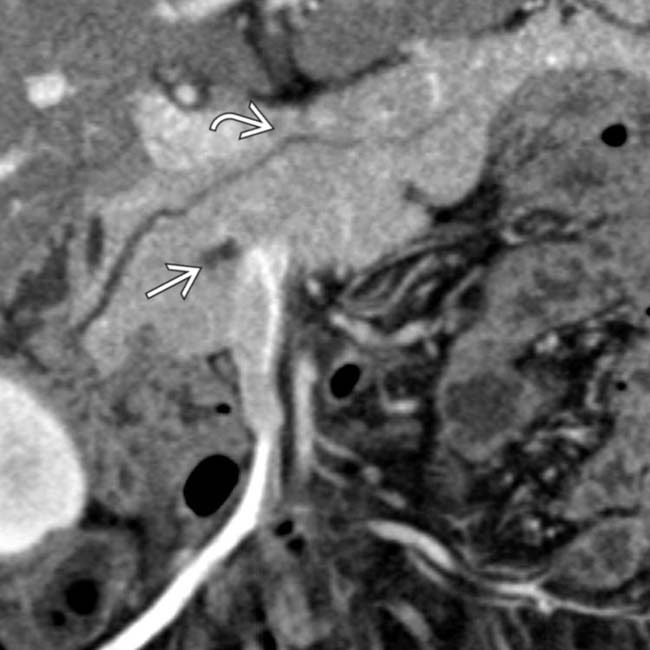
 and a normal caliber pancreatic duct
and a normal caliber pancreatic duct  .
.
 at the site of the central pancreatic resection.
at the site of the central pancreatic resection.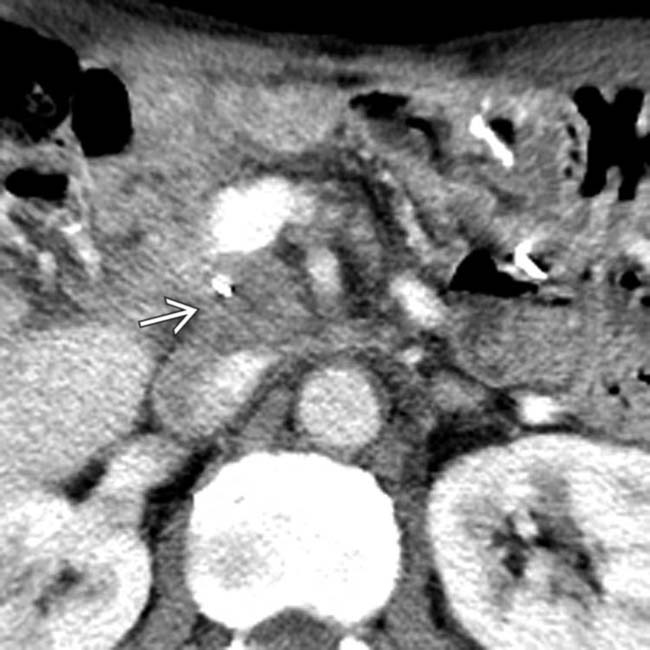
 in the portacaval space 8 months after Whipple resection for carcinoma of the pancreatic head.
in the portacaval space 8 months after Whipple resection for carcinoma of the pancreatic head.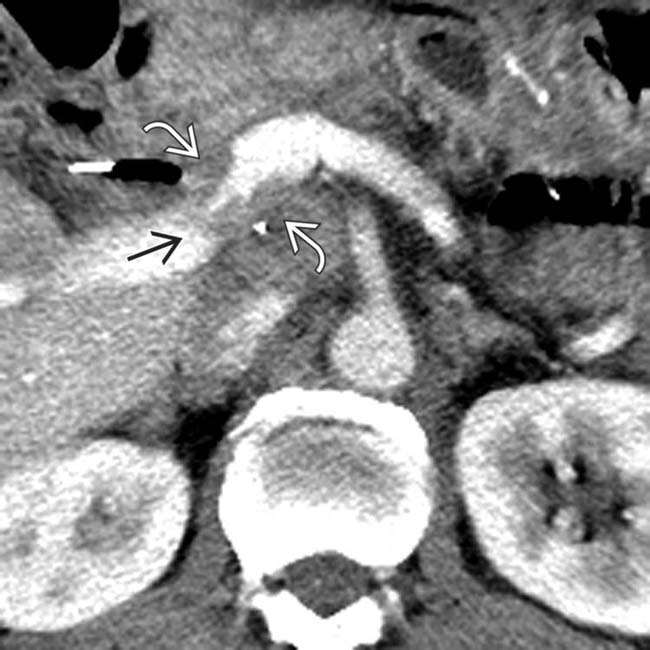
 both anterior and posterior to the splenoportal confluence causing marked narrowing
both anterior and posterior to the splenoportal confluence causing marked narrowing  of the portal vein.
of the portal vein.







































 obstructing the anastomotic site of the pancreatic duct, consistent with a recurrent neuroendocrine tumor.
obstructing the anastomotic site of the pancreatic duct, consistent with a recurrent neuroendocrine tumor.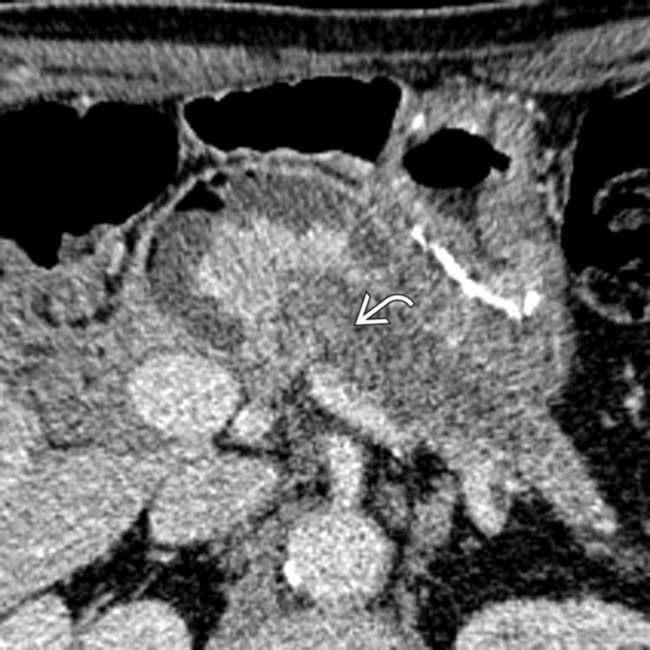
 within the markedly dilated pancreatic duct. Endoscopic ultrasound-guided biopsy confirmed the anastomotic recurrence as well as intraductal growth of neuroendocrine tumor.
within the markedly dilated pancreatic duct. Endoscopic ultrasound-guided biopsy confirmed the anastomotic recurrence as well as intraductal growth of neuroendocrine tumor.


