Consider iatrogenic infarction of hepatic mass or liver parenchyma
 and 2 masses with gas and necrotic debris
and 2 masses with gas and necrotic debris  that are the result of percutaneous radiofrequency ablation.
that are the result of percutaneous radiofrequency ablation.
 but very little fluid in the cholecystectomy bed, mimicking an abscess. Note the surgical clips
but very little fluid in the cholecystectomy bed, mimicking an abscess. Note the surgical clips  . This is bioabsorbable oxidized cellulose (Surgicel), which was used as a hemostatic agent to control bleeding from the operative bed during cholecystectomy.
. This is bioabsorbable oxidized cellulose (Surgicel), which was used as a hemostatic agent to control bleeding from the operative bed during cholecystectomy.
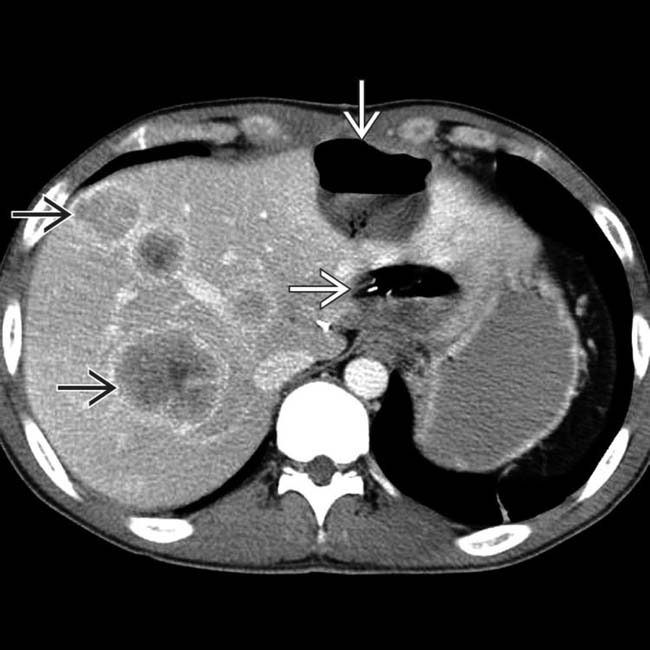
 and portal venous gas
and portal venous gas  , all due to hepatic arterial ligation during attempted resection of a peripheral cholangiocarcinoma.
, all due to hepatic arterial ligation during attempted resection of a peripheral cholangiocarcinoma.
 in the right hepatic artery, with a wedge-shaped collection
in the right hepatic artery, with a wedge-shaped collection  of gas and fluid “downstream.” Needle aspiration and drainage of this collection showed an infected hepatic infarction.
of gas and fluid “downstream.” Needle aspiration and drainage of this collection showed an infected hepatic infarction.IMAGING
Imaging Recommendations
CT Findings
• Gas collection in hepatic or perihepatic lesion
 Iatrogenic infarction of hepatic mass or liver parenchyma
Iatrogenic infarction of hepatic mass or liver parenchyma
 Iatrogenic infarction of hepatic mass or liver parenchyma
Iatrogenic infarction of hepatic mass or liver parenchyma
• Iatrogenic causes of portal venous gas
• Focal hepatic malignancy following chemoembolization
• Consider response to systemic chemotherapy
• Consider prior resection of portions of liver
• Iatrogenic arterioportal (AP) fistula
 Enlarged hepatic arterial branch with early opacification of accompanying portal venous branch and hyperenhancement of subtended segment of liver on arterial phase CECT (or MR)
Enlarged hepatic arterial branch with early opacification of accompanying portal venous branch and hyperenhancement of subtended segment of liver on arterial phase CECT (or MR)
 Enlarged hepatic arterial branch with early opacification of accompanying portal venous branch and hyperenhancement of subtended segment of liver on arterial phase CECT (or MR)
Enlarged hepatic arterial branch with early opacification of accompanying portal venous branch and hyperenhancement of subtended segment of liver on arterial phase CECT (or MR)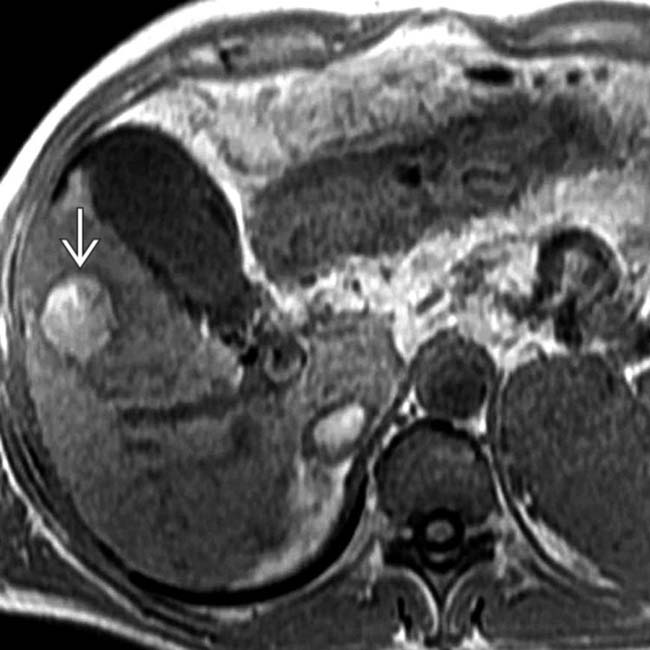
 as hyperintense, which would be unusual for a viable HCC.
as hyperintense, which would be unusual for a viable HCC.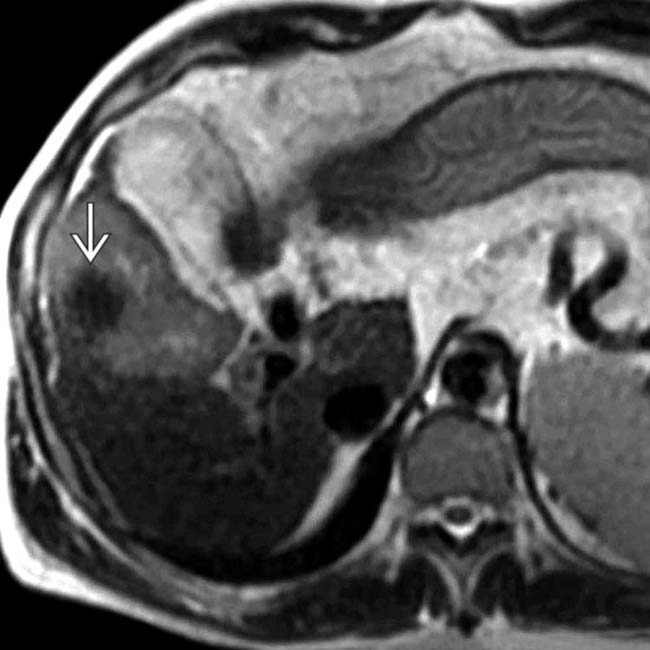
 is hypointense on T2WI, which would be atypical for a viable HCC.
is hypointense on T2WI, which would be atypical for a viable HCC.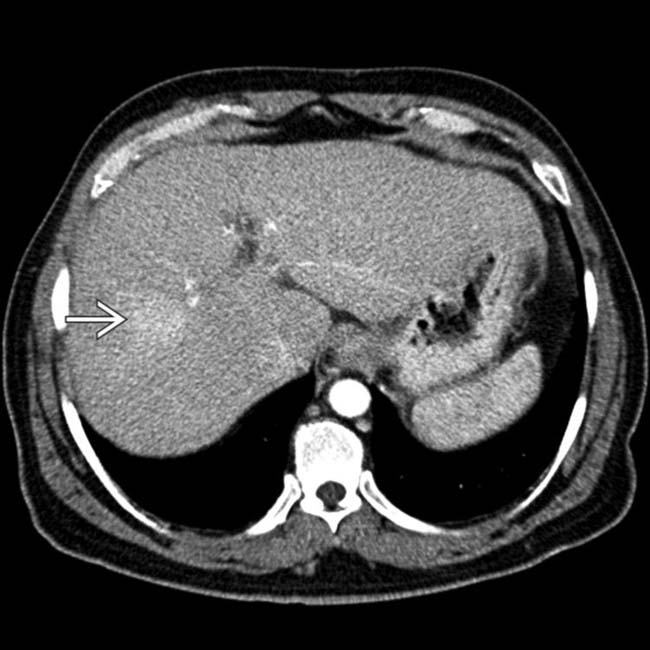
 in the right lobe, along with signs of cirrhosis (widened fissures, etc.).
in the right lobe, along with signs of cirrhosis (widened fissures, etc.).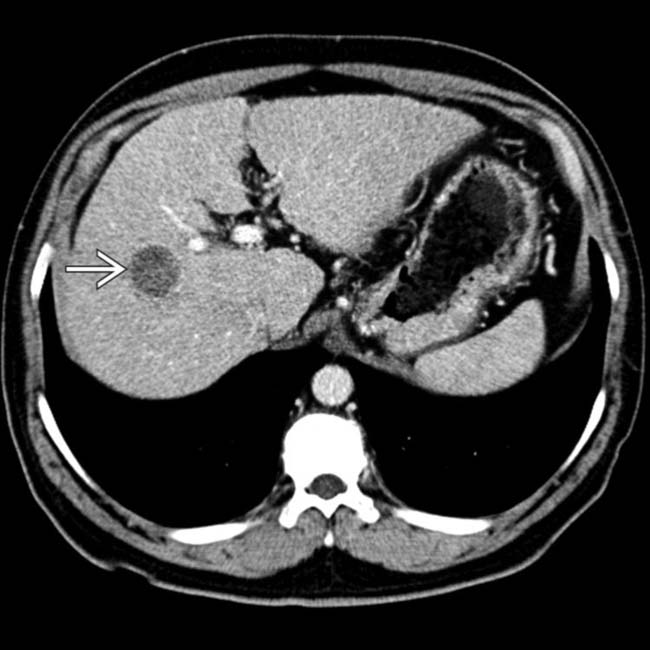
 , essentially diagnostic of hepatocellular carcinoma in this setting. The patient was treated with transarterial chemoembolization, including Lipiodol.
, essentially diagnostic of hepatocellular carcinoma in this setting. The patient was treated with transarterial chemoembolization, including Lipiodol.































 within the tumor. Note the indirect evidence of hepatic injury, with volume loss of the right lobe and ascites.
within the tumor. Note the indirect evidence of hepatic injury, with volume loss of the right lobe and ascites.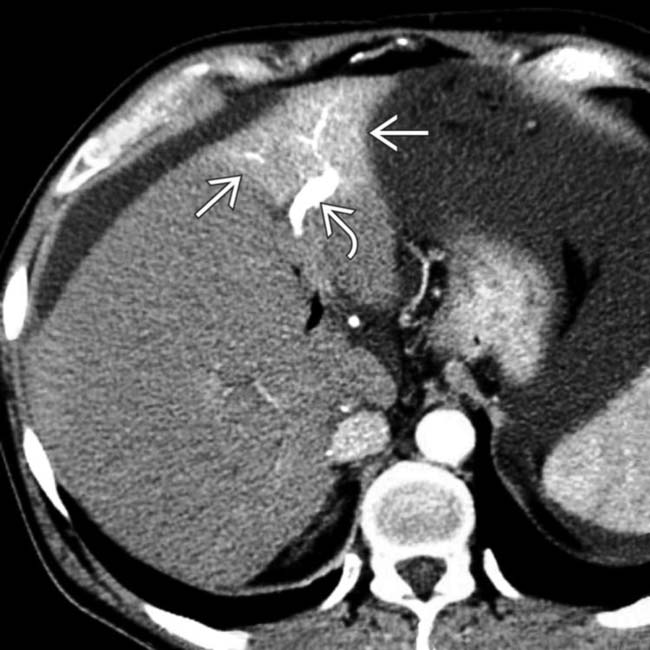
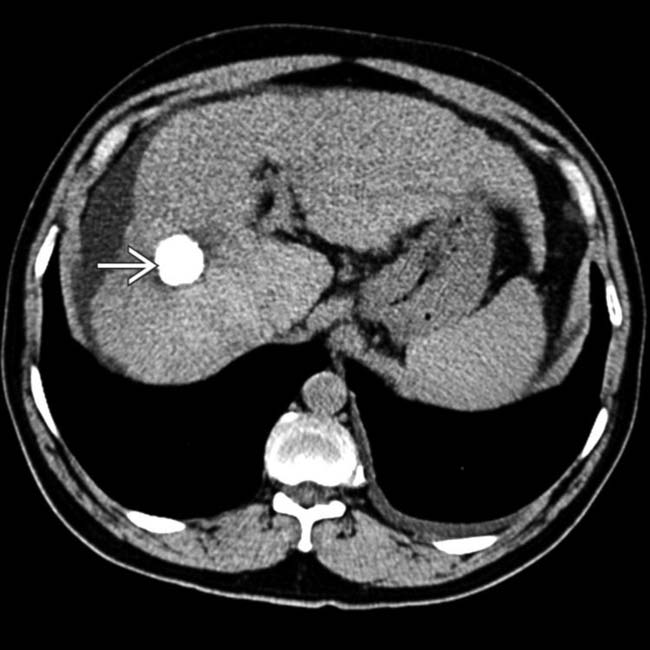
 and early enhancement of the portal vein branch
and early enhancement of the portal vein branch  that drains this segment. This represents an arterioportal shunt and is probably the result of the prior biopsy of the liver at this site.
that drains this segment. This represents an arterioportal shunt and is probably the result of the prior biopsy of the liver at this site.

