Chapter 36 Postanesthesia Recovery
1. What is the postanesthesia care unit (PACU)?
2. What are the requirements for monitoring in the PACU?
3. What are the American Society of Anesthesiologists (ASA) practice guidelines for post anesthesia care?
4. What are some postoperative physiologic disorders that may manifest in the PACU?
Airway obstruction
5. What is the usual mechanism of airway obstruction in the post general anesthesia patient? How does it present clinically?
6. What is the initial intervention to deal with airway obstruction?
7. How may residual neuromuscular blockade manifest in an awake patient?
8. How is residual neuromuscular blockade assessed in an awake patient?
9. What are some factors that contribute to prolonged nondepolarizing neuromuscular blockade in the PACU?
10. What are some factors that contribute to prolonged depolarizing neuromuscular blockade in the PACU?
11. What operative factors may result in life-threatening airway edema in the immediate postoperative period?
12. What leak tests can be performed to evaluate airway patency in patients at risk for airway edema prior to extubation of the trachea?
13. What are some special considerations for patients with obstructive sleep apnea for postanesthesia care?
Hypoxemia in the PACU
14. What are some potential causes of hypoxemia in the PACU? Which of these is most common?
15. What are some potential causes of postoperative hypoventilation?
16. What is the ventilatory response to carbon dioxide?
17. In the PACU, how can hypoxemia secondary to hypercapnia be reversed?
18. What is diffusion hypoxia?
19. Describe the hypoxic pulmonary vasoconstriction (HPV) response and list the conditions and medications that may inhibit it.
20. What is the significance of an increased venous admixture in the PACU?
Oxygen supplementation
25. What is the FIO2 that can be delivered through simple nasal cannula? What are some other options for oxygen delivery in the PACU?
26. What is a high flow nasal cannula? What is its advantage?
27. Is there a role for continuous positive airway pressure (CPAP) and noninvasive positive-pressure ventilation (NIPPV) in the PACU?
Hemodynamic instability
28. What is the significance of hypertension in the PACU?
29. What are some factors associated with significant hypertension in the PACU?
30. What are some causes of hypotension in the PACU?
31. How is myocardial ischemia detected in the PACU?
32. What are some factors which may contribute to cardiac arrhythmias in the PACU?
33. What are some possible causes of sinus tachycardia in the PACU?
34. How should new-onset atrial fibrillation be managed in the PACU?
35. What drugs may contribute to ventricular tachycardia in the PACU?
36. What are some possible causes of bradycardia in the PACU?
Renal dysfunction
40. What is the differential diagnosis of postoperative renal dysfunction?
41. How is oliguria defined? What are some causes of oliguria in the PACU?
42. What are the risk factors for postoperative urinary retention?
43. What are some specific causes of oliguria presenting in the PACU that require immediate attention to prevent ongoing injury?
Answers*
1. The postanesthesia care unit (PACU) is the area equipped and staffed to monitor and care for patients as they emerge from general anesthesia and surgery. Clinical monitoring in the unit is focused on the cardiopulmonary system, with vigilant attention to airway patency and protection, oxygenation, and ventilation, as well as hemodynamic stability. Vital signs are recorded at the minimum every 15 minutes. The unit is located adjacent to the operating room to allow for prompt intervention by anesthesia and surgical staff if needed. (632)
2. Standards and practice parameters for postanesthesia care have been adopted by the ASA. The Standards for Postanesthesia Care is a document that delineates the minimal requirements for monitoring and care in the unit. These are minimal standards that are to be exceeded when deemed appropriate by the judgment of the anesthesia caregiver.
3. Unlike the general ASA standards, the ASA practice guidelines for postanesthesia care provide specific recommendations for clinical evaluation and therapeutic intervention for physiologic disorders that may present in the PACU. (632)
4. A number of postoperative physiologic disorders may manifest in the PACU. These include nausea and vomiting, oliguria, hypoventilation, bleeding, hypothermia, delirium, pain, and delayed awakening. Not surprisingly, data from the U.S. closed claims database show that the most devastating outcomes are the result of airway, respiratory, or cardiovascular compromise. Hypertension or hypotension, cardiac arrhythmia, airway obstruction, hypoventilation, and hypoxemia require immediate attention and intervention. (632, Table 39-1)
Airway obstruction
5. Airway obstruction in the PACU is most often due to the loss of pharyngeal tone resulting from the residual depressant effects of inhaled and intravenous anesthetics and/or the persistent effects of neuromuscular blocking drugs. In awake patients, the pharyngeal muscles contract synchronously with the diaphragm. This activity serves to pull the tongue forward and tent the airway open as the diaphragm creates the negative pressure for inspiration. In the PACU, this pharyngeal muscle activity may be lost and the resultant compliant pharyngeal tissue collapses with negative inspiratory pressure causing obstruction. When this occurs there is a characteristic paradoxic breathing pattern consisting of retraction of the sternal notch and exaggerated abdominal muscle activity. This rocking motion becomes more prominent with increasing airway obstruction. Airway obstruction can be associated with arterial hypoxemia and desaturation on pulse oximetry. (632)
6. Airway obstruction can usually be treated by the jaw thrust maneuver. When this is not sufficient to relieve the obstruction, CPAP can be applied via face mask. If necessary, this can be followed by placement of nasal and oral airways, and in extreme cases laryngeal mask airway or endotracheal tube placement. (632)
7. Residual neuromuscular blockade in the awake patient may manifest as a struggle to breathe. In a patient whose mental status is not clear enough to communicate clearly the patient may appear agitated. (633)
8. Clinical assessment of residual neuromuscular blockade is preferred to the application of the train-of-four ratio and titanic stimulation in awake patients, as both are painful interventions. Clinical evaluation includes grip strength, tongue protrusion, the ability to lift the legs off the bed, and the ability to lift the head off the pillow for a full 5 seconds. Of these, the sustained head lift most directly reflects the ability of the patient to maintain and protect the airway. An extubated patient’s ability to oppose and fix the incisor teeth against a tongue depressor is another clinically reliable indicator to pharyngeal tone. This maneuver correlates with an average train-of-four ratio of 0.85. (633)
9. Factors which may contribute to prolonged nondepolarizing neuromuscular blockade include drugs, diseases, and metabolic states. Drugs which prolong neuromuscular blockade include residual inhaled anesthesia, local anesthetics (lidocaine and other sodium channel blockers), cardiac antiarrhythmic drugs (procainamide), antibiotics (aminoglycosides most commonly), calcium channel blockers, furosemide, and corticosteroids. Metabolic states which may prolong neuromuscular blockade include hypothermia, respiratory acidosis, renal or hepatic failure, hypermagnesemia, and hypocalcemia. Of these, hypothermia and respiratory acidosis are easily recognized and reversible. (633, Table 39-2)
10. Factors which may contribute to prolonged depolarizing neuromuscular blockade include excessive doses of succinylcholine, reduced plasma cholinesterase activity, inhibited cholinesterase activity, and atypical plasma cholinesterase which is a genetic variant. Plasma cholinesterase activity may be reduced due to decreased plasma levels, extremes of age, disease states (hepatic failure, malnutrition, uremia), pregnancy, plasmapheresis, glucocorticoids, and contraceptives. Inhibited cholinesterase activity may be reversible (neostigmine, edrophonium) or irreversible (echothiophate). (633, Table 39-2)
11. Operative factors which may result in life-threatening airway edema in the immediate postoperative period include prolonged procedure in the prone or Trendelenburg position; aggressive fluid resuscitation; surgical procedures on tongue, pharynx, and neck (most common examples are thyroidectomy, carotid endarterectomy, and cervical spine procedures); and hematoma at the surgical site (again, common examples include thyroidectomy and carotid endarterectomy). In the case of volume resuscitation and procedures requiring prone or trend positioning, airway edema may be accompanied by facial and/or scleral edema. In cases such as neck dissection, carotid endarterectomy, and thyroidectomy, life-threatening airway edema may be the result of increased pressure from a hematoma that is not evident on external physical examination. (634)
12. Leak tests can be performed to evaluate airway patency in patients at risk for airway edema prior to extubation of the trachea. One leak test evaluates the patient’s ability to breathe around an occluded endotracheal tube (ETT) with the cuff deflated. One can also measure the intrathoracic pressure required to produce an audible leak around the ETT with the cuff deflated. Another method is to measure the exhaled tidal volume before and after the ETT cuff is deflated. (634)
13. There are some special considerations for patients with obstructive sleep apnea for postanesthesia care. These patients should not be tracheally extubated until they are fully awake. Because of their increased risk for airway obstruction, one should minimize the use of opioids and avoid benzodiazepines or any drugs that depress respiratory drive or promote sleepiness. To this end, the application of continuous regional anesthetic techniques should be used whenever possible. Patients should have CPAP available postoperatively. The patient’s home CPAP or BiPAP (bilevel positive airway pressure) device should be placed on the patient upon admission to the unit. The time in the PACU should be used to evaluate the patient to determine the appropriate degree of monitoring required once discharged from the unit. As a general rule, patients should be monitored with continuous pulse oximetry on the surgical ward. However, because pulse oximetry will not detect carbon dioxide retention in a patient that is receiving supplemental oxygen, many patients with sleep apnea will require intensive care unit level monitoring. (634)
Hypoxemia in the pacu
14. There are multiple potential causes of hypoxemia in the PACU. These include shunting, V/Q mismatch, congestive heart failure, pulmonary edema, alveolar hypoventilation, diffusion hypoxia, aspiration of gastric contents, pulmonary embolus, pneumothorax, posthyperventilation hypoxia, increased oxygen consumption (as from shivering), acute lung injury (e.g., sepsis or transfusion related), advanced age, and obesity. Of these, atelectasis (shunt) and alveolar hypoventilation are the most common causes of postoperative hypoxemia in the PACU. (635, Table 39-3)
15. Among the potential causes of postoperative hypoventilation is anesthetic drugs, residual neuromuscular blocking drugs, impaired ventilatory muscle mechanics, increased levels of carbon dioxide production, and coexisting pulmonary disease. Each of these causes of alveolar hypoventilation leads to a corresponding increase in arterial partial pressure of carbon dioxide (PaCO2). In a patient breathing room air at sea level, hypoventilation to a PaCO2 of 80 will result in hypoxemia, even when the patient has normal lungs without significant A-a gradient. This is demonstrated through the alveolar gas equation. Alveolar oxygen pressure (PaO2) in this scenario is 50. Supplemental oxygen can mask alveolar hypoventilation by leading to normal saturation of oxygen detected by pulse oximetry. (635, Table 39-4, Figure 39-1)
16. Minute ventilation increases in response to elevated PaCO2. Normally minute ventilation increases by approximately 2 L/min for every 1 mm Hg increase in arterial PCO2. In the PACU, this linear response to PCO2 may be depressed by residual vapor or intravenous anesthetics in addition to the administration of narcotics and benzodiazepines. (635)
17. Reversal of hypercapnic hypoxemia can be achieved by the addition of or increase in the concentration of supplemental oxygen and/or the normalization of PCO2. Normalization of PCO2 can be accomplished by stimulation of the patient to wakefulness, the pharmacologic reversal of the effects of narcotics, benzodiazepines and muscle relaxants, or in some cases control of the airway and initiation of positive-pressure ventilation. (636)
18. Diffusion hypoxia refers to the rapid diffusion of nitrous oxide into the alveoli at the end of a nitrous oxide anesthetic. Nitrous oxide dilutes the alveolar gas producing a transient decrease in alveolar oxygen pressure that can persist for up to 5 to 10 minutes after discontinuation of nitrous oxide. In the absence of supplemental oxygen, arterial hypoxemia may ensue. (636)
19. The hypoxic pulmonary vasoconstriction (HPV) response is the attempt of normal lungs to optimally match ventilation and perfusion by constricting vessels that perfuse poorly ventilated alveoli. This vasoconstrictive response shifts blood flow to well-ventilated regions of the lung. The HPV response is inhibited by agents that produce pulmonary vasodilation: inhaled anesthetics, Nipride, and dobutamine to name a few. Physiologic conditions that inhibit this response include pneumonia and sepsis. (636)
20. Increased venous admixture refers to the contribution of mixed venous blood to arterial hypoxemia. This effect is typically significant only in cases of low cardiac output where blood returns to the heart in a severely desaturated state. In the normal lung only, 2% to 5% of the cardiac output is shunted through the lungs, but conditions that increase shunt fraction may significantly increase the effect of venous admixture to hypoxemia. In the PACU, conditions that may increase pulmonary shunt fraction include atelectasis, pulmonary edema, and the aspiration of gastric contents. (636)
Pulmonary edema in the pacu
21. Pulmonary edema in the immediate postoperative period is most often due to cardiogenic causes. Noncardiogenic causes of pulmonary edema in the PACU include pulmonary aspiration, sepsis, and transfusion-related lung injury. (637)
22. Postobstructive pulmonary edema is a transudative edema that results from the exaggerated negative pressure generated by inspiration against an obstructed airway. This negative intrathoracic pressure further promotes venous return, which additionally contributes to transudation of fluid. Young muscular healthy males are most at risk due to their increased muscle mass and ability to generate significant inspiratory force. The most common cause of postobstructive pulmonary edema is laryngospasm. Objective data include hypoxemia and associated bilateral diffuse infiltrates. The diagnosis depends on clinical suspicion once other causes of pulmonary edema are ruled out. (637)
23. TRALI refers to pulmonary edema associated with fever and systemic hypotension after the transfusion of plasma containing blood products. Although fresh frozen plasma and whole blood are the obvious culprits, packed red blood cells and platelets also contain plasma and can trigger TRALI. Typically the physiologic effects of TRALI are manifest within 1 to 2 hours after transfusion, but can occur up to 6 hours after transfusion. A complete blood count obtained with the onset of symptoms would reveal an acute decrease in the white blood cell count reflecting the sequestration of granulocytes within the lung and exudative fluid. The diagnosis is made by an increased alveolar-to-arterial oxygen difference and bilateral pulmonary infiltrates in a chest radiograph. If TRALI is suspected, the transfused blood container bag should be returned to the blood bank for evaluation. (637)
24. TRALI may be difficult to differentiate from transfusion-associated circulatory overload since both manifest as pulmonary edema after the transfusion of blood products. They can be distinguished by the fever and hypotension associated with TRALI, as well as by the characteristics of the resulting edema fluid; exudative in the case of TRALI and transudative in the case of transfusion-associated circulatory overload. In either case treatment is supportive, including supplemental oxygen and diuresis. (637)
Oxygen supplementation
25. As a general rule, each liter per minute of oxygen flow through simple nasal cannula will increase the FIO2 by 0.04. The delivery of oxygen by this method is limited by lack of humidification and temperature correction of the gas. The maximum rate of 6 L/min results in approximately 0.44 FIO2. Other options for oxygen delivery in the PACU include a face mask, non-rebreather face mask, high flow nebulizers, and high flow nasal cannula. Other than the high flow nasal cannula, each of these oxygen delivery methods are limited in the FIO2 they can provide secondary to the entrainment of room air when the patient inhales. (637)
26. High flow delivery systems, such as the high flow nasal cannula, can deliver oxygen at a rate of 40 L/min. Patients tolerate such high flows because the inspired gas is humidified and warmed to 99.9% relative humidity and 37° C. These devices deliver oxygen directly to the nasopharynx throughout the respiratory cycle, and the high flow may enhance the FIO2 by a CPAP effect. (638)
27. The decision to use noninvasive modes of ventilation in the PACU must be guided by careful consideration of both patient and surgical factors. Hemodynamic instability, refractory hypoxemia, and the inability to protect the airway due to altered mental status are standard contraindications to NIPPV. Additional contraindications to consider in this setting include an increased risk of aspiration due to the surgical procedure (i.e., esophagectomy), inability to properly apply the nasal or facemask delivery apparatus because of facial surgery (sinus surgery), or the need to avoid oropharyngeal and gastric distention by positive-pressure ventilation (esophageal and gastric operations, etc.). With the above considerations in mind, home settings of CPAP are recommended routinely for patients with obstructive sleep apnea in the PACU. In the appropriate patient population, application of CPAP in the PACU has been shown to reduce the incidence of intubation, pneumonia, and sepsis in patients who undergo abdominal surgery. (638)
Hemodynamic instability
28. Hypertension and tachycardia in the PACU have been shown to be predictive of unplanned admission to the critical care unit. (638)
29. Patients with essential hypertension are at greatest risk for postoperative hypertension in the immediate postoperative period. Some additional factors to consider include pain, emergence excitement, hypercarbia, gastric distention, drug withdrawal, increased intracranial pressure, and urinary retention. Craniotomy and carotid endarterectomy are surgical procedures that place the patient at increased risk. (638, Table 39-5)
30. A combination of one or more of the following physiologic derangements may account for hypotension in the PACU. These include a decrease in preload, a decrease in afterload, or intrinsic pump failure.
A high spinal anesthetic is an example of all three, because it results in a sympathectomy that dilates venous and arterial vasculature to produce decreased preload and afterload. It also affects the cardioaccelerator fibers of T4, resulting in intrinsic cardiac failure secondary to bradycardia. (638-639, Table 39-6)
31. It is difficult to reliably detect myocardial ischemia in the PACU, because patients are often unable to identify or communicate symptoms of cardiac ischemia in the immediate postoperative period. Patients with postoperative myocardial infarction complained of chest pain less than 20% of the time. Often PACU patients will attribute cardiac pain to incisional pain or vice versa. Furthermore, interpretation of the postoperative EKG must be done with the patient’s cardiac history and risk index in mind. In low-risk patients, ST segment changes do not usually reflect myocardial ischemia. Relatively benign causes of ST segment changes in low-risk patients include anxiety, esophageal reflux, hyperventilation, and hypokalemia.
32. Factors which may contribute to cardiac arrhythmias in the PACU may include hypoxemia, hypercarbia, pain, agitation, electrolyte abnormalities, myocardial ischemia, endogenous or exogenous catecholamines, hypertension, fluid overload, anemia, drug withdrawal, hyperthermia, and hypothermia. (640, Table 39-7)
33. Possible causes of sinus tachycardia in the PACU include pain, agitation, fever, hypercarbia, hypovolemia, anemia, and shivering. Less common and more ominous causes include the onset of cardiogenic or septic shock, pulmonary embolism, thyroid storm, and malignant hyperthermia. (640)
34. New-onset atrial fibrillation which presents in the PACU should be rapidly treated. If the patient is hemodynamically unstable, prompt cardioversion is indicated. Control of the heart rate is a goal of treatment in these patients and can be achieved with β-adrenergic blockers or calcium channel blocking drugs. Diltiazem is the calcium channel blocker of choice in this circumstance. Often rate control is enough to convert the heart rhythm from new-onset atrial fibrillation to sinus rhythm in the PACU. If chemical conversion is indicated, an amiodarone loading dose can be initiated. (640)
35. Premature ventricular contractions and ventricular bigeminy are common in the PACU. They are most often a result of increased sympathetic tone as may accompany pain or hypercarbia. Ventricular tachycardia is rare in the PACU, and is indicative of underlying cardiac abnormality. In the case of torsades de pointes, the administration of drugs that prolong the QT interval, such as amiodarone, procainamide, droperidol, and serotonin uptake inhibitors to name only a few, may contribute to the cardiac abnormality. (640)
36. Bradycardia in the PACU is often iatrogenic. Drug related causes include the administration of β- or calcium channel blockers, anticholinesterase reversal of neuromuscular blockade, narcotic administration, and sedation with dexmedetomidine. Procedure-related and patient-related causes include bowel distention, increased intracranial pressure or intraocular pressure, and high spinal anesthesia that blocks the cardioaccelerator fibers originating from T1 to T4. Underlying conduction abnormalities and myocardial ischemia are indications for emergent intervention. (641)
Delirium
37. The incidence of postoperative delirium in patients older than 50 years old is approximately 10%. The incidence is highest in patients undergoing joint replacement. (641)
38. Postoperative delirium may be patient-related, iatrogenic, or surgery-related. The most significant predictors of postoperative delirium are advanced age, preoperative cognitive impairment, decreased functional status, alcohol abuse, and previous history of delirium. Intraoperative factors that are predictive of postoperative delirium include surgical blood loss, hematocrit less than 30, and the number of intraoperative transfusions. Some additional causative factors include arterial hypoxemia, hypercapnia, pain, sepsis, inadequate hydration, medications, and electrolyte abnormalities. (641)
39. Emergence excitement is a transient confusional state that is associated with the emergence of general anesthesia. It is more common in children than adults, with a peak incidence in children between the ages of 2 and 4 years. More than 30% of children will experience delirium at some period during their PACU stay. It typically resolves quickly and is followed by an uneventful recovery. (641)
Renal dysfunction
40. The differential diagnosis of postoperative renal dysfunction includes preoperative, intraoperative, and postoperative causes. Frequently the cause is multifactorial, and a preexisting renal insufficiency may be exacerbated by an intraoperative insult. For example, preoperative infection, contrast radiologic studies, or hepatic dysfunction may put patients at risk for decompensation of renal function from intravascular volume depletion intraoperatively. In the PACU, diagnostic efforts should focus on the identification and treatment of readily reversible causes of oliguria. (642)
41. Oliguria is defined as a urine output of less than 0.5 mL/kg/hr. Postoperative oliguria may be due to prerenal, renal, or postrenal causes. Prerenal causes include hypovolemia due to bleeding, sepsis, third space fluid loss, inadequate volume resuscitation, hepatorenal syndrome, low cardiac output, renal vascular obstruction, or intraabdominal hypertension. Intrarenal causes include acute tubular necrosis, radiographic contrast dyes, rhabdomyolysis, tumor lysis, and hemolysis. Postrenal causes include urinary retention, surgical injury or obstruction to the ureters, or mechanical obstruction to the urinary catheter. The most common cause of oliguria postoperatively is the depletion of intravascular volume. (642, Table 39-9)
42. Postoperative urinary retention refers to the inability to void despite a bladder volume of more that 500 to 600 mL. Risk factors include age over 50, male gender, intraoperative volume resuscitation, duration of surgery, bladder volume on admission, and type of surgery, in particular anorectal procedures or joint replacement. Other contributors include perioperative medications such as anticholinergics, β-blockers, and narcotics. (642)
43. Three causes of oliguria presenting in the PACU that should be immediately treated to prevent ongoing injury include intraabdominal hypertension, rhabdomyolysis, and contrast nephropathy. Intraabdominal hypertension should be ruled out by measuring the bladder pressure in any oliguric patient with a tense abdomen postoperatively. Persistently elevated intraabdominal pressure impedes renal perfusion and leads to renal ischemia.
Body temperature and shivering
44. The incidence of postoperative shivering may be as high as 65% after general anesthesia. Postoperative shivering is not always associated with a decrease in body temperature; shivering in normothermic patients is thought to result from uninhibited spinal reflexes manifested as clonic activity. Postoperative shivering can be treated with opioids and clonidine. Meperidine is the most effective treatment for postoperative shivering. (643)
45. Adverse effects of postoperative hypothermia include shivering, inhibition of platelet function, coagulation factor activity, and drug metabolism. These may result in exacerbation of postoperative bleeding, prolonged neuromuscular blockade, and delayed awakening. Forced air warmers can be used to warm patients with postoperative hypothermia. (643)
Postoperative nausea and vomiting
46. Patient-related factors associated with an increased incidence of postoperative nausea and vomiting (PONV) include female gender (postpuberty), nonsmoking status, childhood (past infancy), and history of motion sickness or PONV. Anesthetic factors include use of volatile anesthetics or nitrous oxide, administration of large doses of neostigmine, and perioperative opioids. Significant surgical factors include type of procedure, such as eye muscle or middle ear surgery, gastric distention as in swallowed blood, and duration of surgery. (643)
47. There is a simplified risk score for identifying patients at risk for PONV. It is a four point score that allots a single point for each of the following factors: (1) female gender, (2) history of motion sickness or PONV, (3) nonsmoking, (4) use of postoperative opioids. A score of 0, 1, 2, 3, or 4 correlates to an incidence of 10%, 21%, 39%, 61%, and 79%, respectively. Although prophylactic measures to prevent PONV are more effective than rescue drugs administered in the PACU, some patients have PONV despite prophylaxis. There are several drugs available for the treatment of PONV, including scopolamine, hydroxyzine, promethazine, droperidol, metaclopromide, ondansetron, dolasetron, and dexamethasone. Dexamethasone is most effective when given prophylactically at the start of surgery, and ondansetron is most effective when given 30 minutes before the end of anesthesia. (643-644)
Delayed awakening
48. Residual effects of anesthetic or sedating drugs are the most common cause of delayed awakening in the PACU. If narcotic or benzodiazepines are suspected, then careful titration of the reversal drugs, naloxone and flumazenil, can be used. For example, in adults 20- to 40-μg increments of naloxone are used to avoid abrupt reversal of analgesia and associated hypertension and tachycardia. The use of flumazenil should be done with caution to avoid precipitation of seizures. Both naloxone and flumazenil have short half-lives, so the patient should be carefully observed for resedation. Rarely physostigmine may be used to reverse the CNS effects of anticholinergic drugs. Hypothermia and hypoglycemia should also be considered as potential causes of delayed awakening postoperatively. (644)
Discharge criteria
49. PACU discharge criteria are based on the principles that patients must be observed until they are no longer at risk for respiratory depression and their mental status has returned to baseline. No specific length of stay is required and hemodynamic parameters are based on the patient’s baseline measurements. (645)
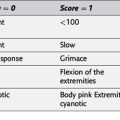
50. The Aldrete scoring system is an objective measure assigning points, or a score, to a patient to determine readiness for discharge. Components of the Aldrete scoring system include an activity, breathing, circulation, consciousness, and oxygen saturation. The patient must be able to breathe comfortably, clear secretions, and oxygenate adequately. (645)