CHAPTER 49 Pitanguy breast reduction
Physical evaluation
Physical evaluation of the patient presenting for breast reduction includes:
With patient standing up
• Overall evaluation of patient’s biotype: height, weight, chest girth.
• Examination of breast skin (elasticity, signs of dermal fragility such as striae, maceration or infection from intertrigo).
• Inspection of degree of flaccidity by checking level of nipple with respect to the submammary sulcus.
• Estimation of breast volume (visual and by palpation).
• Verification of excess parenchyma with a two-handed pinching maneuver, also noting distance the nipple–areolar complex (NAC) will have to rise.
• Examination of other breast deformities, such as inverted nipple.
Anatomy
Postoperative anatomy of the breast is also important. All resected tissues are sent to the pathology laboratory for close inspection. As has been published previously, it is interesting to note that the segment where most of breast pathology arises – the lower pole – is exactly the region that is removed in both of the techniques to be described.
The classic Pitanguy breast reduction technique
Indicated for large hypertrophy
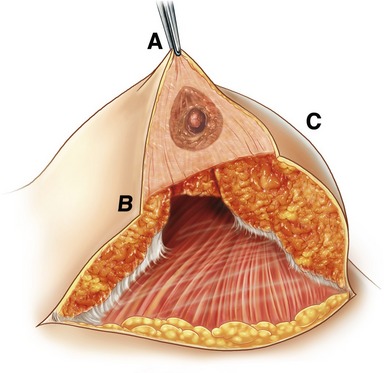
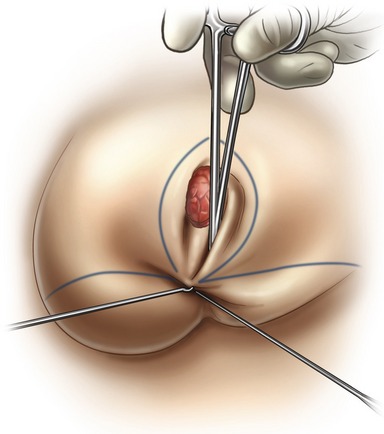
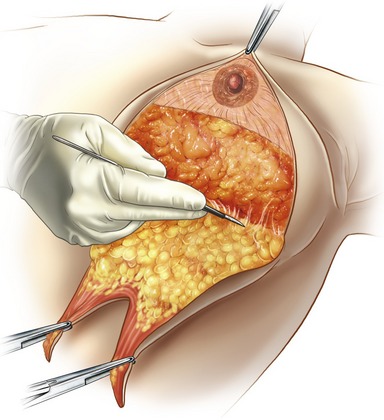
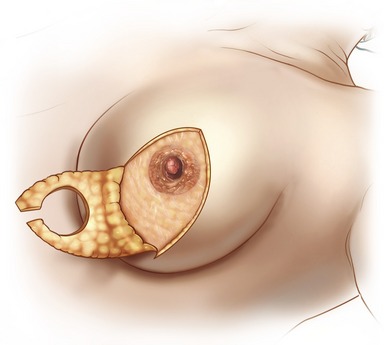
Fig. 49.7 The inverted keel resection should be applied to breasts that are mainly composed of glandular tissue.
• Patient is placed in a semi-sitting position.
• Two long sutures are placed along the midline, to help the surgeon check for symmetry during demarcation and at the end of the procedure.
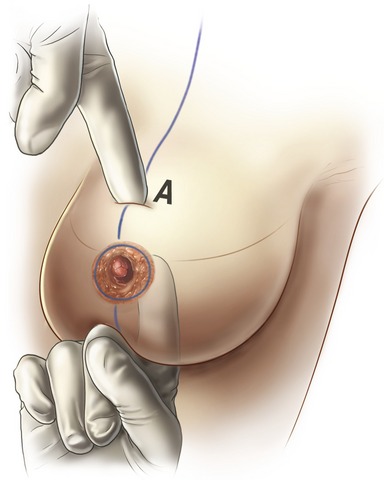
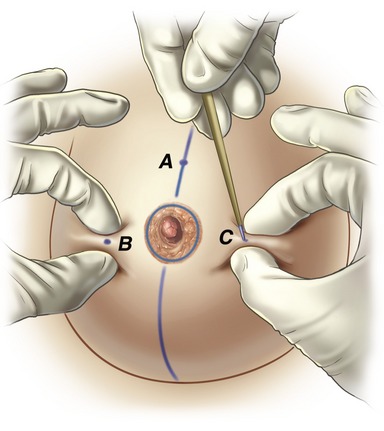
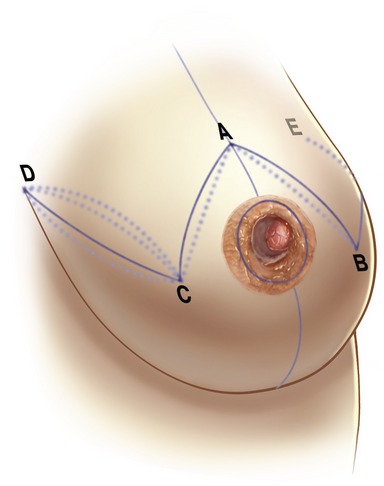
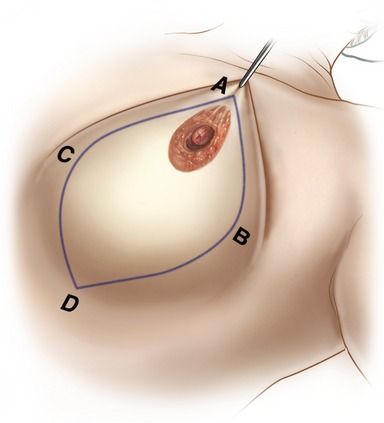
• Midclavicular line is drawn, through the NAC all the way to the sulcus. Point A is determined along this line, at or slightly lower than the breast sulcus. (This point determines the future position of the NAC.)
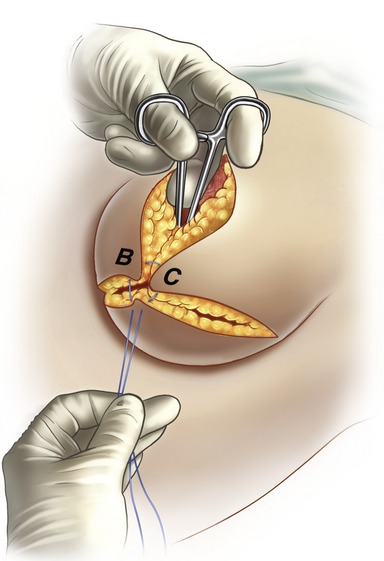
• By pinching excess skin points B and C are determined.
• Two points, D and E, define the medial and lateral extension of the horizontal incision, not extending beyond the midline and the anterior axillary line. The lines uniting these points are curved when excess skin is present.
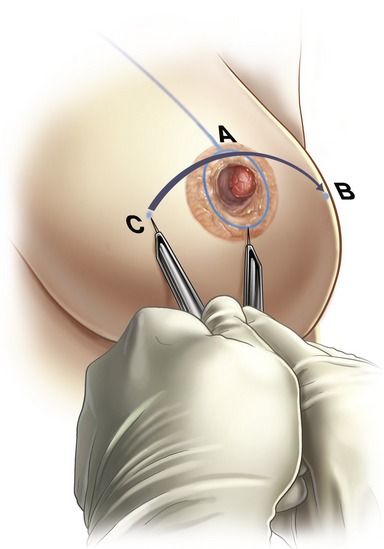
• The area between points A–B–C is de-epithelialized (Schwartzman’s maneuver). This assures the maintenance of the dermal capsule of the superior pole, which is considered the third neurovascular pedicle of the CAM.
• Glandular resection is always restricted to the inferior pole, and is straight when the breast is composed mainly of fatty tissue or in an inverted ship’s keel fashion if the parenchyma is more glandular.
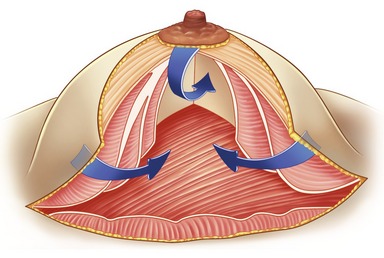
• Two pillars, medial and lateral, are created with both forms of resection. The upper-pedicled NAC will slide upwards as the pillars are approximated, and all dead space is eliminated.
• The operated breast is wrapped in moist towels and the same procedure is done on the opposite breast. The two are then lifted by the assistant, and inspected from a distance to compare remaining parenchyma, one side with the other.
• Tissues are now brought together with one main suture, bringing points A–B–C to the midline. Sutures are done from deep to superficial planes.
• The new position of the NAC is now determined by inspection, and demarcated on both sides. Symmetry is checked once again, using the two long sutures. A main advantages of this technique is that the surgeon feels that he is free to demarcate the new position of the NAC, and is not bound to fixed measures as in other techniques.
See Clinical cases 1–6 (Figs 49.C1–49.C6).
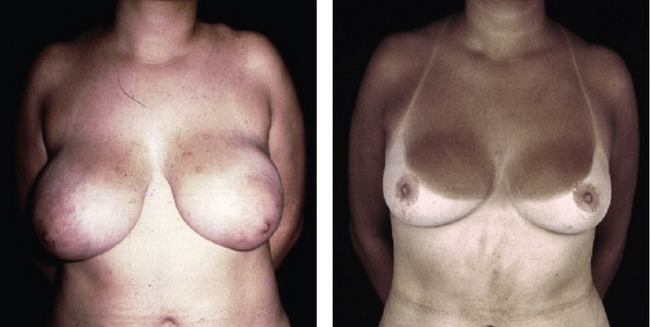
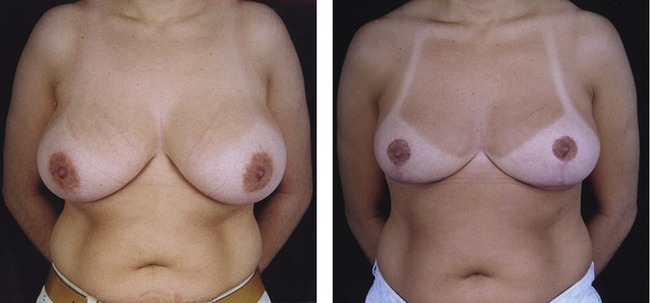
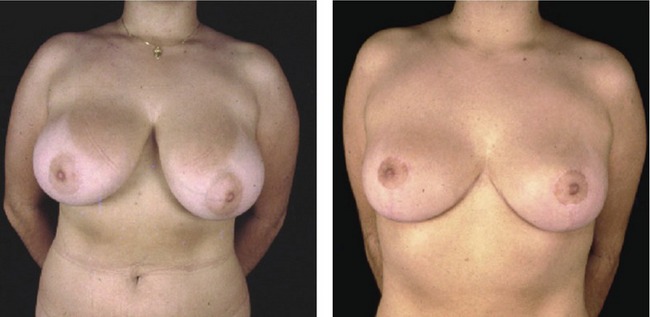
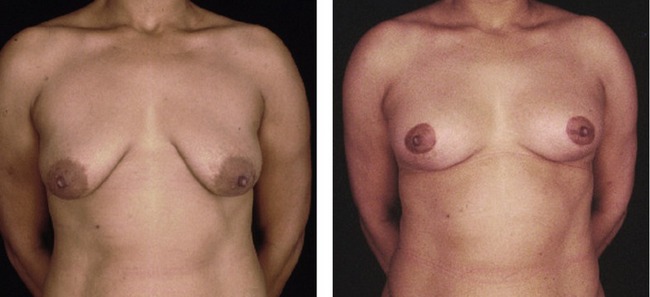
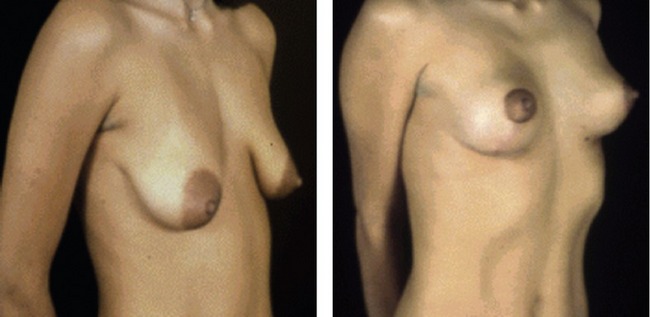
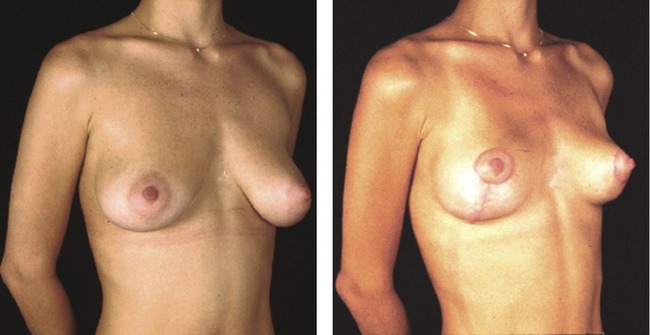
Fig. 49.C3 Clinical case 3: Reducing very large breasts is feasible with the classic Pitanguy approach, as in this 41-year-old woman; she has taken part in outdoor activities, showing her sun marks.
The rhomboid Pitanguy breast reduction technique
Indicated in small to medium hypertrophy and breast ptosis
• The initial demarcation is elliptical or rhomboid and finishes with a single vertical scar.
• Point A is determined as previously described.
• The surgeon estimates how much skin must be removed by pinching the medial and lateral skin on either side of the nipple, and points B and C are determined.
• Point D, which should not be lower than the sulcus, will complete the elliptical demarcation. The final incision is a vertical scar, ending at (or slightly below) the submammary sulcus.
• Resection can be restricted to skin when simple ptosis is present, or can include a variable amount of breast tissue from the lower pole, when the patient desires reduction of volume.
• As described in the classic technique, the inverted keel resection, when indicated, creates two pillars or columns. Once these are approximated, the superior pole is defined and the nipple will rise to the new position.
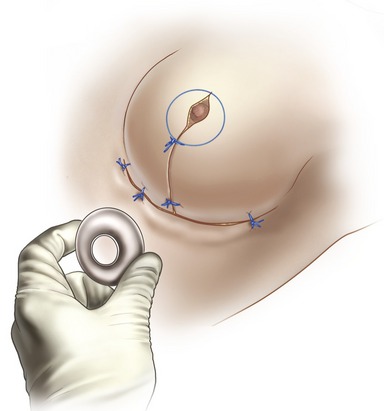
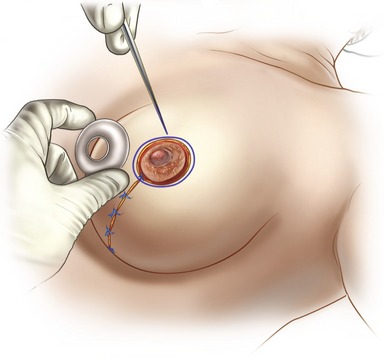
• An appropriate areola demarcator is chosen for placement of the NAC, around the area of point A.
• The final vertical incision may be complemented with a small horizontal component, converting the single scar into an “L” or inverted “T” so as not to extend the scar beyond the sulcus.
Postoperative care
• Patients submitted to reduction mammoplasty are discharged either 24 or 48 hours postoperative.
• Dressings are changed and the breasts are inspected for hematoma collection and skin ischemia.
• The patient returns for follow-ups every 4–7 days until last sutures are removed.
• Silicone sheeting is used routinely, unless there is history of allergy.
• The patient must refrain from physical exercises or strenuous activities that use the upper limbs for the first month.
• Monthly revisions are done until the 6th month and then at one year postoperative. At this time, postoperative photographs are done and touch-ups may be planned.
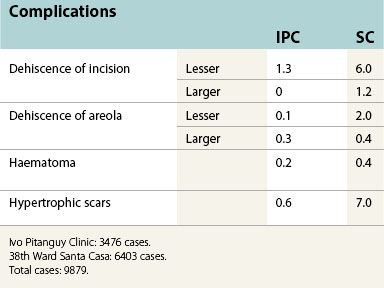
Complications
• The rate of complications following breast reduction using the classic or rhomboid Pitanguy techniques is very low. This is due to no dissection of breast parenchyma, and preservation of the vascular pedicle of the NAC. Also, the inverted keel resection assures that, on closure, all dead space is eliminated.
• Most dehiscences are small and self-limiting; blood collections are very infrequent and rarely require drainage. Vascular insufficiency to the NAC, although rare, is usually transitory, and mostly limited to the epidermis.
| Idade | IPC | SC |
|---|---|---|
| 10–19 years | 4.0 | 11.0 |
| 20–29 years | 26.0 | 33.0 |
| 30–39 years | 32.0 | 29.0 |
| 40–49 years | 21.0 | 17.0 |
| 50–59 years | 14.0 | 7.0 |
| ≥60 years | 3.0 | 3.0 |
Ivo Pitanguy Clinic: 3476 cases.
38th Ward Santa Casa: 6403 cases.
Total cases: 9879.
Pearls & pitfalls
Pearls
• Maintaining function and sensitivity of the breast: The preservation of innervation and vascular supply of the nipple–areola complex are addressed, and the remaining parenchyma will allow breast feeding.
• Achieving satisfactory volume and lasting form: The upper pole is projected by the rotation of the lower pole. As no dissection is performed and all dead space is eliminated, the breast mound maintains its conical shape.
• Reducing scars: Even large breasts may be reduced to a suitable size with final scars that will be easily camouflaged under bathing attire.
Summary of steps
The classic Pitanguy breast reduction technique
1. Patient is placed in a semi-sitting position. Two long sutures are placed along the midline.
2. Midclavicular line is drawn, through the NAC all the way to the sulcus. Point A is determined along this line, at or slightly lower than the breast sulcus.
3. By pinching excess skin, points B and C are determined.
4. Two points, D and E, define the medial and lateral extension of the horizontal incision, not extending beyond the midline and the anterior axillary line.
5. The area between points A–B–C is de-epithelialized (Schwartzman’s maneuver).
6. Glandular resection is always restricted to the inferior pole.
7. Two pillars, medial and lateral, are created with both forms of resection.
8. The operated breast is wrapped in moist towels and the same procedure is done on the opposite breast.
9. Tissues are now brought together with one main suture, bringing points A–B–C to the midline. Sutures are done from deep to superficial planes.
10. The new position of the NAC is now determined by inspection.
The rhomboid Pitanguy breast reduction technique
1. The initial demarcation is elliptical or rhomboid and finishes with a single vertical scar.
2. Point A is determined as previously described.
3. The surgeon estimates how much skin must be removed by pinching the medial and lateral skin on either side of the nipple, and points B and C are determined.
4. Point D, which should not be lower than the sulcus, will complete the elliptical demarcation.
5. The inverted keel resection, when indicated, creates two pillars or columns. Once these are approximated, the superior pole is defined and the nipple will rise to the new position.
6. An appropriate areola demarcator is chosen for placement of the NAC, around the area of point A.
7. The final vertical incision may be complemented with a small horizontal component, converting the single scar into an “L” or inverted “T” so as not to extend the scar beyond the sulcus.
Pitanguy I. Breast hypertrophy. In: Wallace AB, ed. Transactions of the International Society of Plastic Surgeons, Second Congress. Edinburgh: E. & S: Livingstone; 1960:509.
Pitanguy I. Surgical treatment of breast hypertrophy. Br J Plast Surg. 1967;20:78.
Pitanguy I. The breast. In: Pitanguy I, ed. Aesthetic plastic surgery of head and body. Berlin: Springer-Verlag, 1981.
Pitanguy I. Reduction mammaplasty by the personal technique. In: Chang WHJ, ed. The breast: An atlas of reconstruction. Baltimore: Williams & Wilkins; 1984:75–160.
Pitanguy I. Personal preferences for reduction mammaplasty. In: Georgiade ND, ed. Aesthetic surgery of the breast. Philadelphia: W.B: Saunders; 1990:167.
Pitanguy I. Principles of reduction mammaplasty. In: Georgiade ND, ed. Aesthetic surgery of the breast. Philadelphia: W.B: Saunders; 1990:191.
Pitanguy I. Reduction mammaplasty: A personal odyssey. In: Goldwyn RM, ed. Reduction mammaplasty. Boston: Little: Brown; 1990:95.
Pitanguy I, Radwanski HN. Philosophy and principles in the correction of breast hypertrophy. In: Mang WL, Bull HG. Ästhetische Chirurgie. Germany: Einhorn-Presse Verlag; 1996:216–232.
Pitanguy I. Evaluation of body contouring surgery today: A 30-year perspective. Plast Reconstruct Surg. 2000;105:1499.
Pitanguy I, Torres E, Salgado F, Pires V, Giovanni A. Breast pathology and reduction mammaplasty. Plast Reconstruct Surg. 2005;115(3):729–734.