2 Pharmacology
Ocular Pharmacology
Pharmacodynamics
the study of the biochemical and physiologic effects of drugs and their mechanisms of action.
Bioavailability
amount of drug absorbed (penetration into ocular tissues)
Routes of Administration
Topical
absorption related to corneal penetration
Anesthetics
Structure
2 classes; do not necessarily have allergic cross-reactivity
Topical
disturb intercellular junction of corneal epithelium (increase permeability)
Parenteral
General
all agents decrease IOP except ketamine, chloral hydrate, N2O, and ether
Autonomic System
Sympathetic
Extensive system for mass response (‘fight or flight’) (Table 2-1)
| Organ / Function | Sympathetic (fight / flight) | Parasympathetic (homeostasis) |
|---|---|---|
| HR | Increase | Decrease |
| BP | Increase | Decrease |
| GI motility | Decrease | Increase |
| Bronchioles | Dilate | Constrict |
| Bladder | Constrict | Dilate |
| Vessels | Constrict | Dilate |
| Sweat | Decrease | Increase |
| Pupils | Dilate | Constrict |
| Eyelids | Elevate | Normal |
Synapses near cord (superior cervical ganglion)
Adrenergic receptors
Parasympathetic
More limited system for discrete response (homeostatic)
Cholinergic Drugs
Indirect-acting agonists
Muscarinic antagonists
Adrenergic Drugs
Sympathomimetics
Ocular Hypotensive (Glaucoma) Medications
β-Blockers
Nonselective (β1 and β2)
timolol (Timoptic), levobunolol (Betagan), metipranolol (Optipranolol), carteolol (Ocupress)
Miotics
Pilocarpine
only direct cholinergic agonist; peak action at 2 hours, 8-hour duration
Echothiophate (phospholine iodide)
Carbonic Anhydrase Inhibitors (CAIs)
Carbonic anhydrase catalyzes the reaction
Sulfonamide derivative (do not administer to patients with sulfa allergy)
Oral
acetazolamide (Diamox; PO / IV), methazolamide (Neptazane, PO; more lipid soluble, less toxicity)
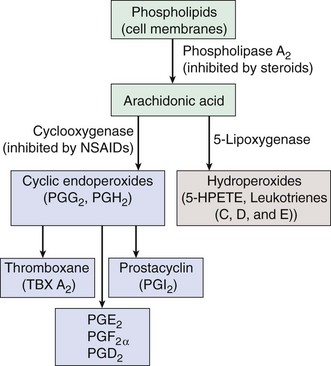
Prostaglandin Analogues / Prostanoids
Hyperosmotic Agents
Glycerin (Osmoglyn; PO; 50% solution)
may cause hyperglycemia in diabetics (metabolized by liver into glucose)
Isosorbide (Ismotic; PO)
not metabolized (can be used in diabetics); secreted 95% unchanged in urine
Anti-Inflammatory Drugs
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Steroids
Preparations (ketones)
Potency
increased by 1–2 double bond(s), 9 fluorination, 6 methylation, O at C11; IOP elevation from deoxygenation at C21 (Table 2-2)
| Steroid | Relative potency |
|---|---|
| Hydrocortisone | 1 (the standard) |
| Cortisone | 0.8 |
| Triamcinolone | 4 |
| Prednisone | 4 |
| Prednisolone | 5 |
| Dexamethasone | 25–30 |
| Betamethasone | 25–30 |
| Fluorometholone | 40–50 |
| Fluocinolone | 240 |
Subconjunctival / sub-Tenon’s injection (Table 2-3)
produces higher ocular concentration and longer duration; beware in IOP responder
| Generic name | Trade name |
|---|---|
| Topical | |
| Prednisolone acetate 1% | Pred Forte, Omni Pred |
| Fluorometholone acetate 0.1% | Flarex |
| Dexamethasone alcohol 0.1% | Maxidex |
| Fluorometholone alcohol 0.1% | FML |
| Prednisolone phosphate 1% | Inflamase |
| Dexamethasone phosphate 1% | Decadron |
| Difluprednate 0.05% | Durezol |
| Loteprednol etabonate 0.5% | Lotemax |
| Loteprednol etabonate 0.2% | Alrex |
| Subconjunctival | |
| Dexamethasone phosphate | Decadron |
| Methylprednisolone acetate | Solumedrol, Depomedrol |
| Prednisolone acetate | Durapred |
| Triamcinolone acetonide | Kenalog |
| Betamethasone | Celestone |
| Intravitreal | |
| Triamcinolone acetonide | Kenalog, Triesence |
Indications
conjunctivitis, keratitis, scleritis, uveitis, hyphema, CME, macular edema, CNV, endophthalmitis
Adverse effects
Antiallergy Medications
Immunosuppressive Agents
Cytotoxic Alkylating Agents
Immunomodulator
Anti-Infective Drugs
Antibiotics
Inhibitors of Intermediary Metabolism
Inhibitors of Cell Wall Synthesis
β-Lactams (cidal)
Penicillins (PCN)
least toxic; variable protein binding
Cephalosporins
more resistant to β-lactamases; 20% cross react with PCN-allergic patients
Non β-Lactams (cidal)
Inhibitors of Protein Synthesis
Aminoglycosides
cidal; inhibit 30S ribosome; poor GI absorption
Tetracyclines
Others
Fluoroquinolones
Anti-TB Agents
Antivirals
Topical
Antifungals
Polyenes
bind to ergosterol; damages fungal membranes
Antiamoebics
Miscellaneous
Aminocaproic acid (Amicar)
Botulinum toxin (Botox)
neurotoxin that blocks release of acetylcholine from nerve terminal; paralyzes muscle (1–3 months)
Ocular Toxicology (Table 2-4)
Anticholinergics (atropine, scopolamine, Donnatal)
| Ocular structure | Effect | Drug |
|---|---|---|
| Extraocular muscles | Nystagmus, diplopia | Anesthetics, sedatives, anticonvulsants, propranolol, antibiotics, phenothiazines, pentobarbital, carbamazepine, MAO inhibitors |
| Lid | Edema | Chloral hydrate |
| Discoloration | Phenothiazines | |
| Ptosis | Guanethidine, propranolol, barbiturates | |
| Conjunctiva | Hyperemia | Reserpine, methyldopa |
| Allergy | Antibiotics, sulfonamides, atropine, antivirals, glaucoma medications | |
| Discoloration | Phenothiazines, chlorambucil, phenylbutazone | |
| Cornea | Keratitis | Antibiotics, phenylbutazone, barbiturates, chlorambucil, steroids |
| Deposits | Chloroquine, amiodarone, tamoxifen, indomethacin, gold | |
| Pigmentation | Vitamin D | |
| Increased IOP | Open angle | Anticholinergics, caffeine, steroids |
| Narrow angle | Anticholinergics, antihistamines, phenothiazines, tricyclic antidepressants, haloperidol, sulfonamides (Topamax) | |
| Lens | Opacities / cataract | Steroids, phenothiazines, ibuprofen, allopurinol, long-acting miotics |
| Myopia | Sulfonamides, tetracycline, prochlorperazine, autonomic antagonists, duloxetine (Cymbalta) | |
| Retina | Edema | Chloramphenicol, indomethacin, tamoxifen, carmustine |
| Hemorrhage | Anticoagulants, ethambutol | |
| Vascular damage | Oral contraceptives, oxygen, aminoglycosides, talc, carmustine, interferon | |
| Pigmentary degeneration | Phenothiazines, indomethacin, nalidixic acid, ethambutol, isotretinoin, chloroquine, hydroxychloroquine | |
| Optic nerve | Neuropathy | Ethambutol, isoniazid, sulfonamides, digitalis, imipramine, streptomycin, busulfan, cisplatin, vincristine, chloramphenicol, disulfiram |
| Papilledema | Steroids, vitamin A, tetracycline, phenylbutazone, amiodarone, nalidixic acid, isotretinoin |
Antibiotics
Phenothiazines (chlorpromazine, thioridazine)
pigmentary retinopathy, corneal deposits, cataracts, angle closure
Review Questions (Answers start on page 357)
Doughty M. Ocular Pharmacology and Therapeutics: A Primary Care Guide. Philadelphia: Butterworth-Heinemann; 2001.
Fraunfelder FT, Fraunfelder FW, Randall JA. Drug-Induced Ocular Side Effects, 5th edn. Philadelphia: Butterworth-Heinemann; 2001.
Fraunfelder FT, Roy FH. Current Ocular Therapy, 5th edn. Philadelphia: WB Saunders; 2000.
Grant WM, Schuman JS. Toxicology of the Eye, 4th edn. Springfield, IL: Charles C. Thomas; 1993.
Greenbaum S. Ocular Anesthesia. Philadelphia: WB Saunders; 1997.
2012 Physicians’ Desk Reference for Ophthalmic Medicines. Montvale, NJ: Medical Economics, 2012.
Zimmerman TJ. Textbook of Ocular Pharmacology. Philadelphia: Lippincott-Raven; 1997.


 β2)
β2)