Ascites may be slightly higher in attenuation (15-30 HU) on CT than simple ascites
 Internal complexity within ascites fluid (septations, debris) is common and easier to appreciate on MR or US
Internal complexity within ascites fluid (septations, debris) is common and easier to appreciate on MR or US• Other imaging findings may reveal cause of peritonitis (i.e., diverticulitis, appendicitis, low-attenuation nodes in TB)

 . There are bilateral drains
. There are bilateral drains  in place.
in place.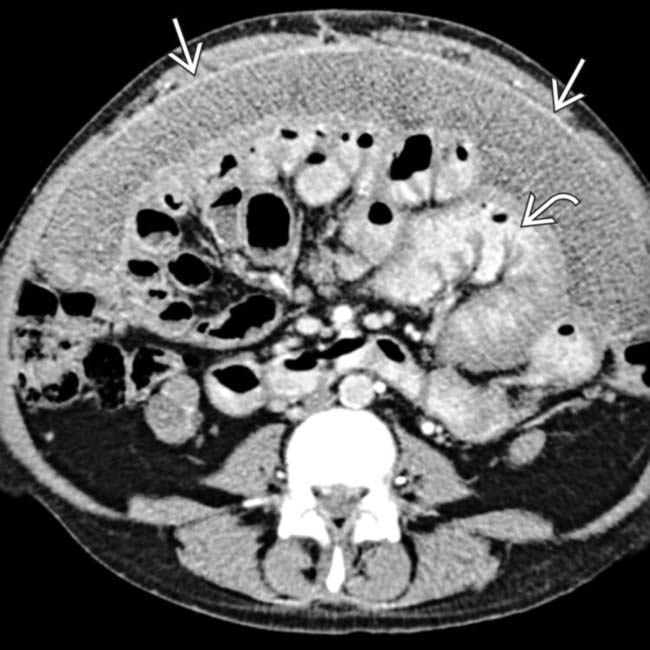
 with thickened, enhancing parietal/visceral peritoneum encasing the small bowel and creating functional obstruction. Note the dilated segments of bowel
with thickened, enhancing parietal/visceral peritoneum encasing the small bowel and creating functional obstruction. Note the dilated segments of bowel  .
.
 and thickening of the peritoneal lining.
and thickening of the peritoneal lining.
 surrounding bowel loops in the pelvis. These findings are classic for sclerosing peritonitis, most typically seen in patients on chronic peritoneal dialysis.
surrounding bowel loops in the pelvis. These findings are classic for sclerosing peritonitis, most typically seen in patients on chronic peritoneal dialysis.IMAGING
General Features
CT Findings
• Smooth, regular thickening and enhancement of peritoneum (can be either localized adjacent to site of inflammation or generalized throughout abdomen)
• Other imaging findings may reveal cause of peritonitis (i.e., diverticulitis, appendicitis, low-attenuation nodes in tuberculous peritonitis)
Ultrasonographic Findings
DIFFERENTIAL DIAGNOSIS
Peritoneal Carcinomatosis
• Metastatic disease to omentum, peritoneum, or mesentery (most commonly ovarian cancer and gastrointestinal malignancies)
PATHOLOGY
General Features
• Etiology
 Traumatic peritonitis
Traumatic peritonitis
 Peritonitis does not necessarily always imply infection: Sterile peritonitis also possible
Peritonitis does not necessarily always imply infection: Sterile peritonitis also possible
 Traumatic peritonitis
Traumatic peritonitis
– May result from either frank perforation of bowel or traumatic disruption of peritoneum allowing infection
 Peritonitis does not necessarily always imply infection: Sterile peritonitis also possible
Peritonitis does not necessarily always imply infection: Sterile peritonitis also possible
– Sterile peritonitis most commonly iatrogenic, such as foreign body reaction to retained foreign body after surgery or chronic peritoneal inflammation due to peritoneal dialysis catheter

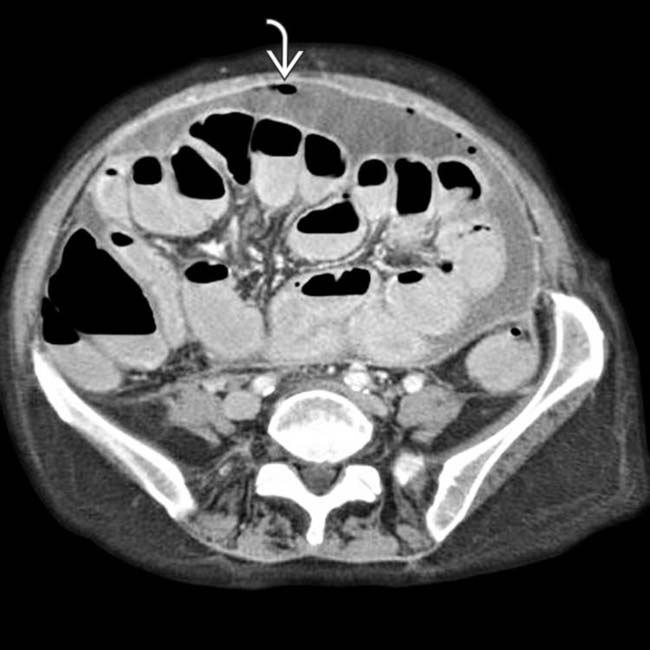
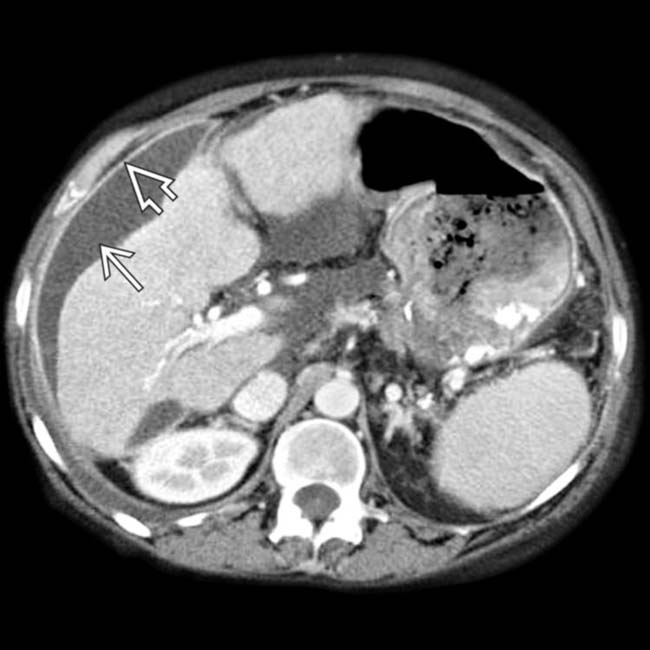
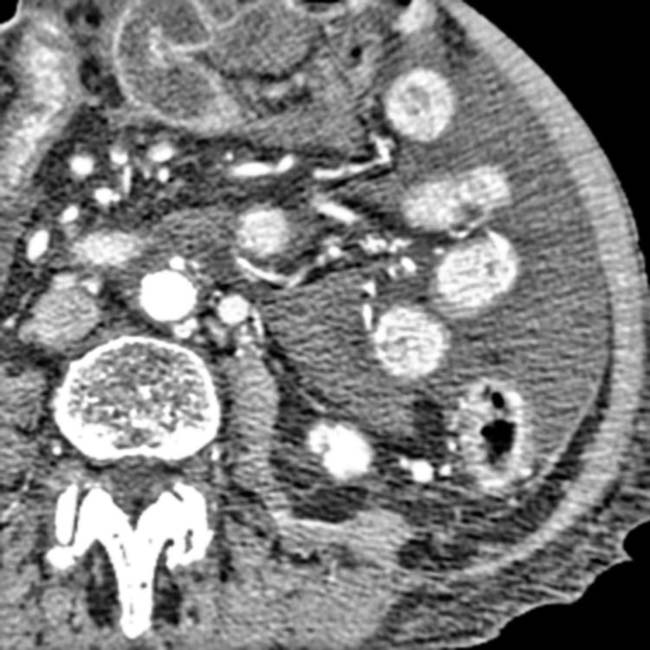
 , and calcification
, and calcification  within a thickened omentum.
within a thickened omentum.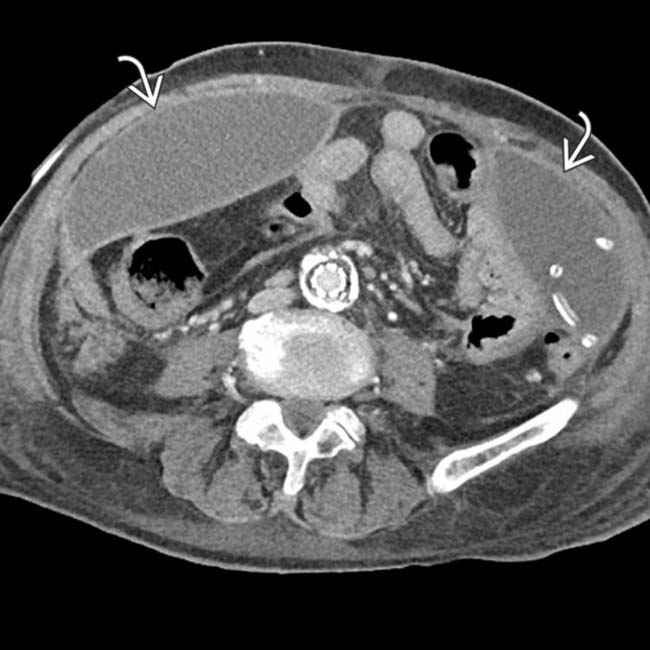
 .
.
 .
.
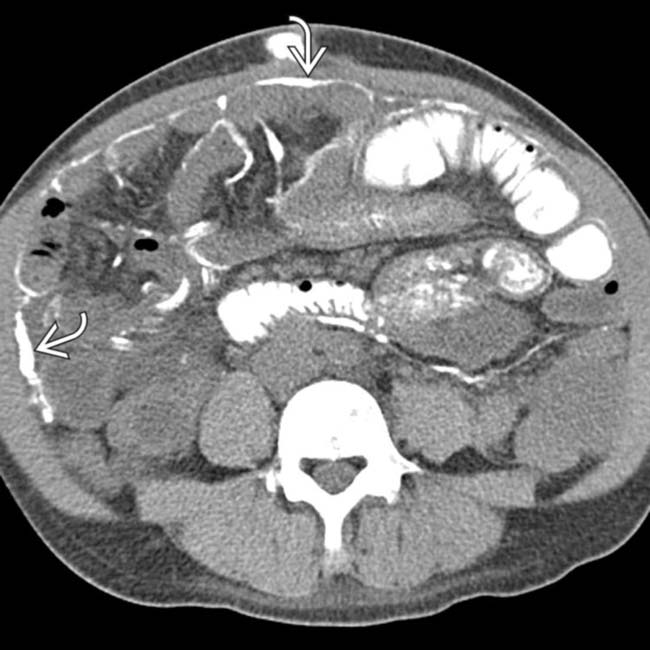
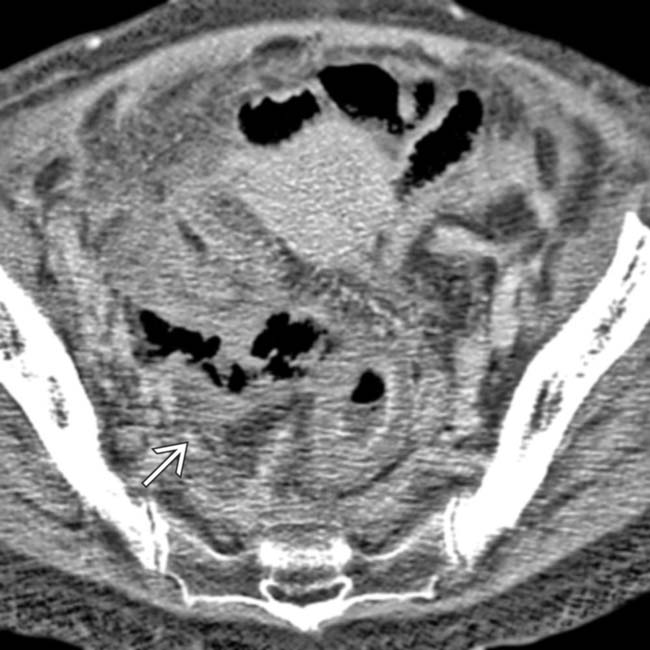
 within the ascites fluid, a classic imaging finding of bacterial peritonitis.
within the ascites fluid, a classic imaging finding of bacterial peritonitis.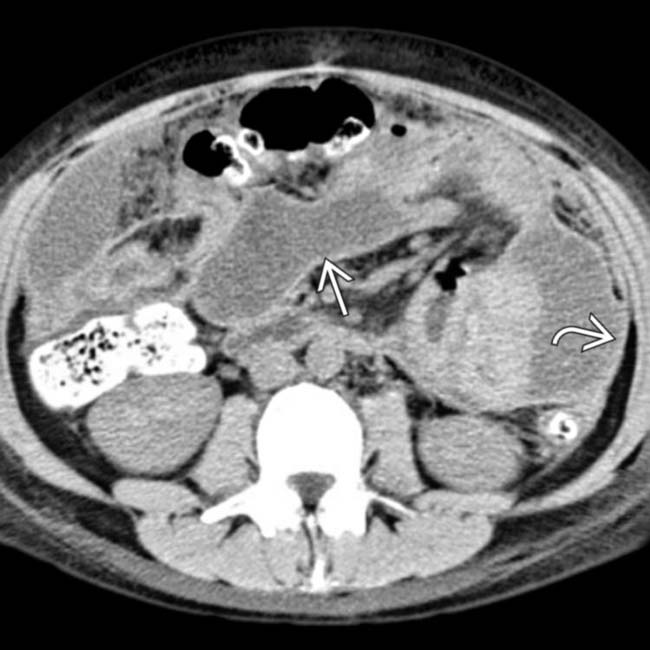
 . The thickened parietal peritoneum
. The thickened parietal peritoneum  is further evidence of an inflammatory or exudative etiology for this process.
is further evidence of an inflammatory or exudative etiology for this process.
 and mesenteric fat due to the generalized inflammatory process and peritonitis.
and mesenteric fat due to the generalized inflammatory process and peritonitis.
 , thickening of the parietal peritoneum
, thickening of the parietal peritoneum  , and nodular infiltration of the omentum
, and nodular infiltration of the omentum  .
.
 and cystic disease of dialysis
and cystic disease of dialysis  .
.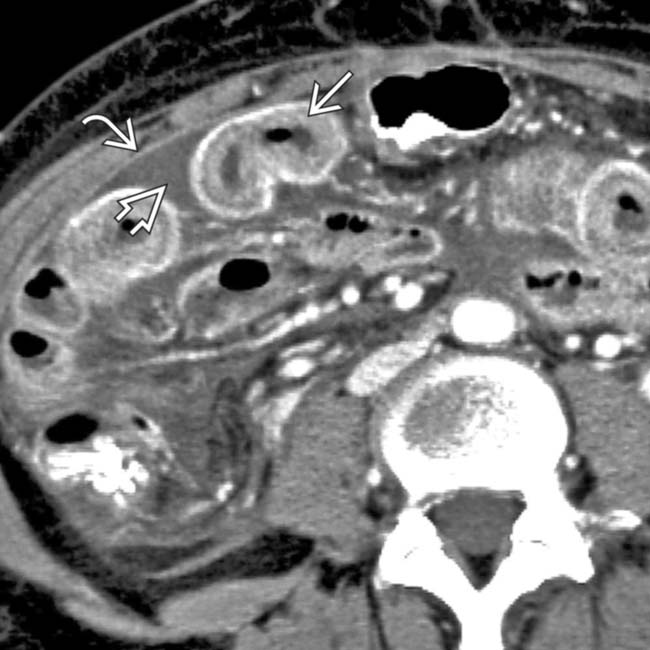
 , ascites
, ascites  , and peritoneal enhancement
, and peritoneal enhancement  .
.
 and peritoneal enhancement
and peritoneal enhancement  .
.
 and the thickened and enhancing parietal peritoneum
and the thickened and enhancing parietal peritoneum  .
.
 and thickened parietal peritoneum
and thickened parietal peritoneum  . A gas bubble
. A gas bubble  is also evident within the fluid.
is also evident within the fluid.
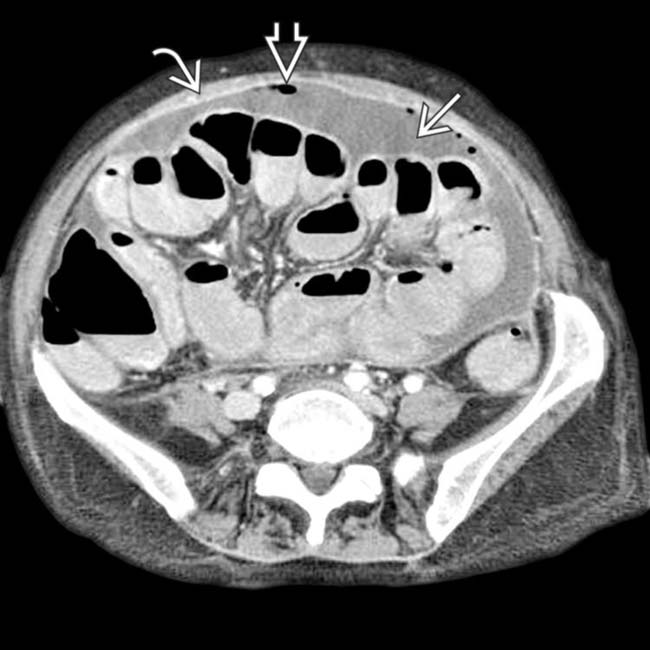
 and ectopic gas
and ectopic gas  adjacent to the thickened sigmoid colon
adjacent to the thickened sigmoid colon  .
.
 . Diffuse pelvic peritonitis was found at surgery.
. Diffuse pelvic peritonitis was found at surgery.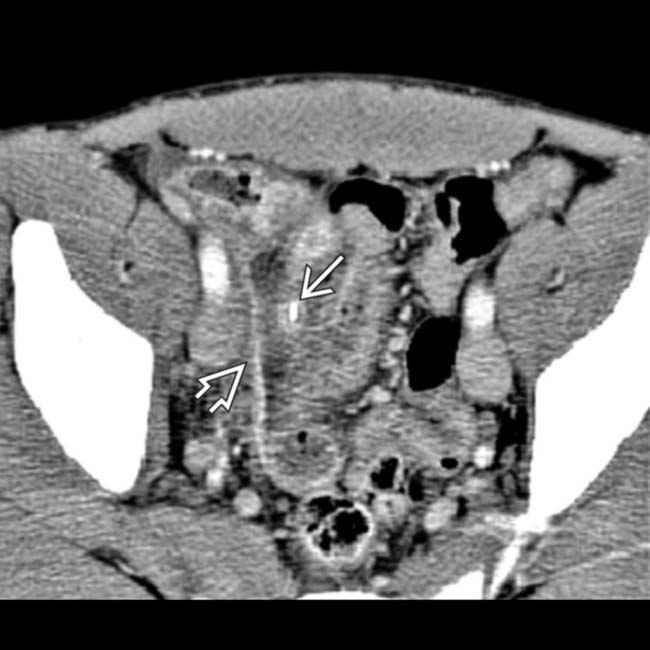
 , symmetric thickening of the peritoneum
, symmetric thickening of the peritoneum  , and adjacent low-attenuation pus.
, and adjacent low-attenuation pus.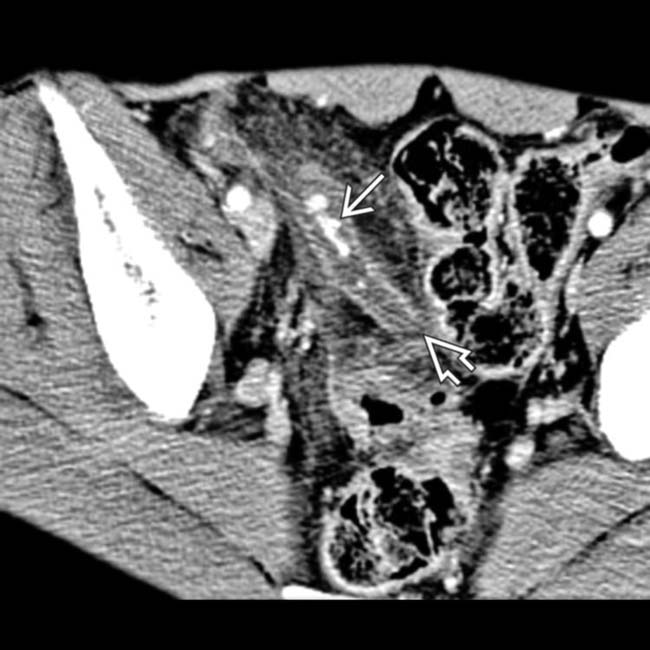
 with a nonenhancing necrotic tip of the appendix
with a nonenhancing necrotic tip of the appendix  and surrounding soft tissue infiltration.
and surrounding soft tissue infiltration.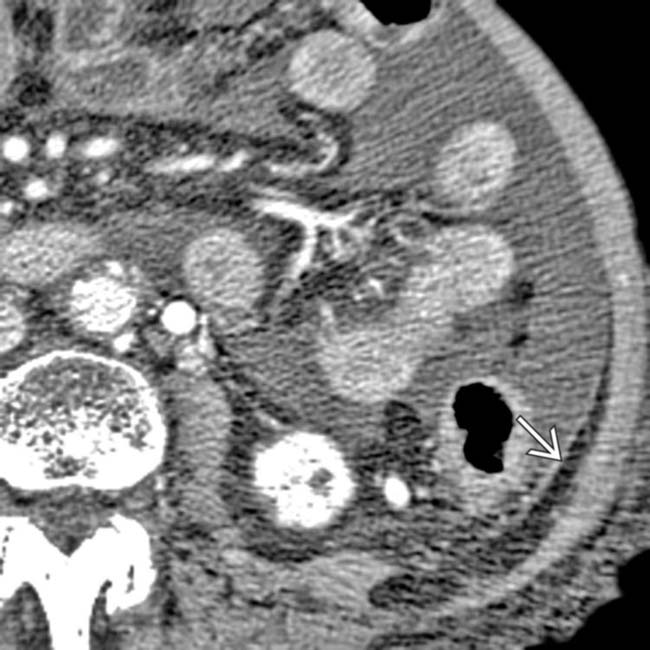
 .
.
 and a hyperemic thickened small bowel
and a hyperemic thickened small bowel  .
.
 and massive perihepatic low-density fluid.
and massive perihepatic low-density fluid.
 with an adjacent clot
with an adjacent clot  and a large amount of bile in the peritoneal cavity.
and a large amount of bile in the peritoneal cavity.
 and marked serosal thickening and enhancement of the jejunum
and marked serosal thickening and enhancement of the jejunum  .
.
 encasing loops of small bowel.
encasing loops of small bowel.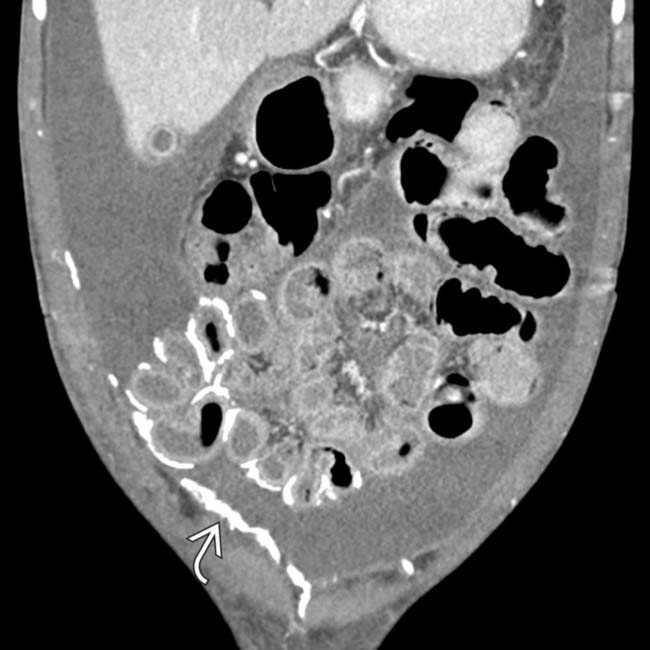










































 and peritoneum.
and peritoneum.
 with innumerable cysts and the present of a massive, highly loculated ascites.
with innumerable cysts and the present of a massive, highly loculated ascites.
 .
.


