Chapter 12 Periocular Reconstruction
PERIOCULAR ANATOMY
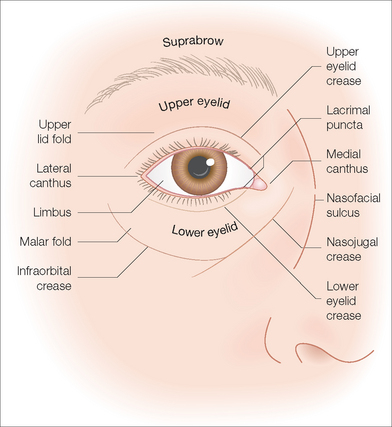
Surface Anatomy
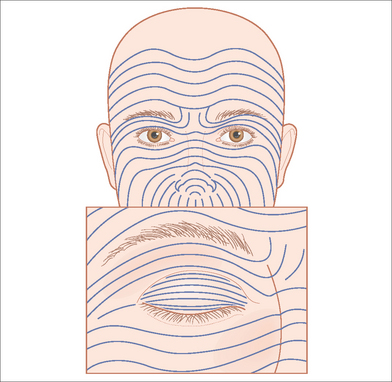
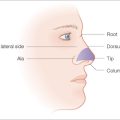
It is useful to conceptually divide the face into aesthetic units when discussing reconstructive techniques.1,2 Recognizing the junction lines between neighboring units is important as they conceal surgical scars well. Most authors use the eyebrow as the superior limit of the periocular aesthetic unit; however, the suprabrow area can also be considered to be part of the periocular area, as closures in this area can affect the eyebrow and upper eyelid (Figure 12.1). The infraorbital and nasojugal creases define the inferior border of the periocular unit. The nasofacial sulcus marks the medial border in the medial canthal area, while the frontal process of the zygomatic bone defines the lateral margin. Anatomically, it is also useful to distinguish the palpebral portions of the upper and lower eyelids, which overlie the globe when the lids are closed, from the orbital portions, which continue over the bony orbital margin to the edge of the periocular aesthetic unit.
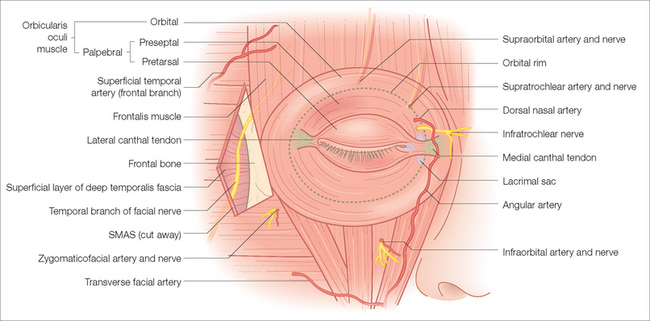
Surgical Anatomy
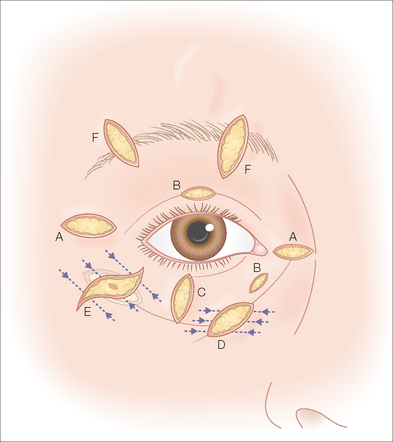
A thorough knowledge of the anatomy of the periocular region is paramount to successful surgery in this area (Figure 12.2). Understanding tissue planes and functional relationships between anatomic structures serve the surgeon well in this complex area. Familiarity with the location of nerves, blood vessels, and “danger zones” is critical to achieving optimal surgical results and avoiding bad outcomes.
The orbicularis oculi muscle lies superficial to the orbital septum. The sphincter muscle of the eyelids, it controls blinking and forceful eyelid closure. It can be divided into palpebral and orbital portions. The palpebral part, confined to the eyelids, arises from the medial canthal tendon and arches across both lids (anterior to the tarsal plates) to insert into the lateral canthal tendon. In oculoplastic surgery it is useful to further subdivide this part into the pretarsal and preseptal portions. The orbital portion of the muscle, located more peripherally, lies flat on the surface of the orbital margin, bordering the forehead and cheek. Its fibers arise from the medial end of the medial canthal tendon and adjoining bone to extend laterally in a series of uninterrupted concentric loops around the orbit. The elevator of the upper lid is the levator palpebrae superioris, a long, flat muscle above the globe. Its aponeurosis fuses with the orbital septum superiorly to insert into the superior tarsus and skin of the upper eyelid.
The temporal branch of the facial nerve is the most superficially located (and thus most susceptible) motor nerve in the periocular area. From its emergence beneath the parotid gland in the preauricular region, its course is roughly delineated by drawing one line from 0.5 cm below the tragus to a point 2 cm above the lateral end of the eyebrow and a second along the zygomatic arch.3,4 The nerve is most superficial in the area of the zygomatic arch, and it is therefore most at risk to damage during a surgical procedure at this site. Anatomically, the four tissue layers of importance in the area of the lateral canthus are the skin and subcutaneous fat, the superficial muscular aponeurotic system (SMAS), the temporalis fascia, and the temporalis muscle. The SMAS is a thin layer of connective tissue that is continuous with the galea superiorly, the frontalis anteriorly, the occipitalis posteriorly, and the muscles of facial expression inferiorly. In the area of the temple, the temporal branch of the facial nerve runs just below the SMAS, within a layer of loose areolar tissue superficial to the temporalis fascia.4 At the lateral forehead the nerve dives under the frontalis muscle, becoming less vulnerable to surgical injury. The temporal nerve innervates the ipsilateral frontalis muscle and, to a lesser extent, the orbicularis oculi muscle, and nerve transection leads to weakness of the ipsilateral forehead with droop of the eyebrow and decreased ability to close the eye tightly. The importance of understanding the course of the facial nerve branches and their anatomic relationship to these tissue planes cannot be overstated.
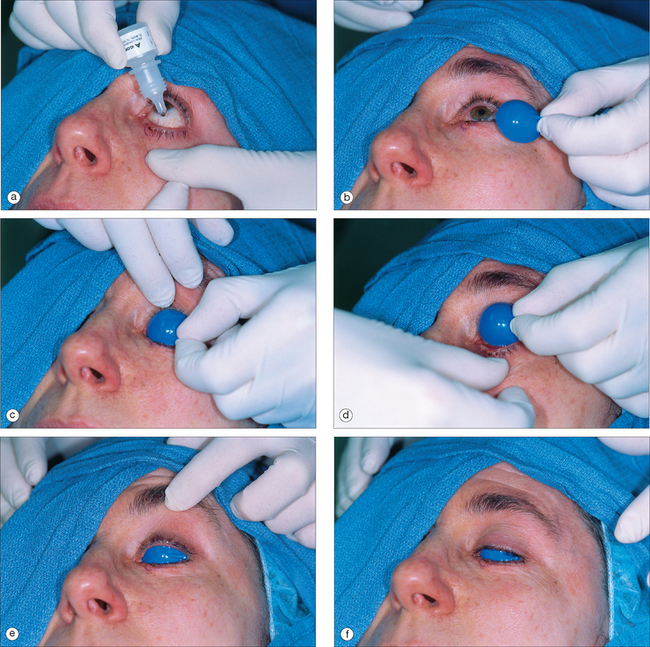
PREPARATION
Consideration should be given to using protective corneal shields to prevent inadvertent surgical trauma,5 especially if the procedure will involve the palpebral portion of the eyelids (Figure 12.3). These shields are inexpensive and easily inserted under the lids after instilling several drops of tetracaine 0.5% or a similar anesthetic into the palpebral fissure. The shields are generally well tolerated. To minimize migration and inadvertent corneal exposure during surgery, the largest size corneal shields that can comfortably be inserted should be used. Besides protecting the globe, the shields also block the patient’s view of the bright surgical lights. Both plastic and metal shields are available; the same metal shields used for laser resurfacing (Jedmed, St Louis) can be used for general reconstructive surgery.
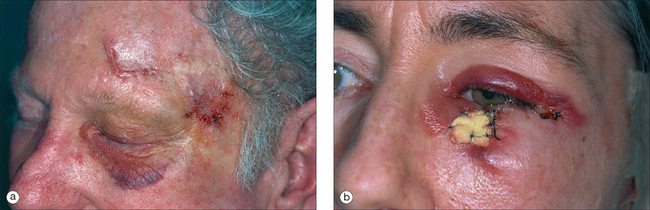
During the discussion of the procedure and expected postoperative course, the surgeon should prepare the patient for the possibility of swelling and bruising, which are not uncommon in the thin, distensible tissues of the eyelids (Figure 12.4). This is an expected part of periorbital surgery. Having the patient sleep with the head in an elevated position for the first few days after surgery may minimize postoperative bruising. Although short-lived and usually painless, the bruising can at times be quite dramatic and alarming to the patient. Because of gravitational forces, periorbital ecchymoses can occasionally extend as inferior as the jaw line.
GENERAL PRINCIPLES OF PERIOCULAR RECONSTRUCTION
How well a surgical scar is hidden is a function of three factors: the tension on the wound, the quality of the tissue used to close the defect, and the placement of skin incisions. Wounds closed with minimal tension heal better and form less prominent scars. Fortunately, there is minimal intrinsic tension in the periocular region when compared to other body areas such as the back or chest, where hypertrophic and spread scars are common. To minimize tension across a wound, it is also important to consider the relaxed skin tension lines (RSTLs) (Figure 12.5). These lines indicate the direction of least tension in relaxed skin (incisions parallel to them experience less tension while healing). Perpendicular to the RSTLs are the lines of maximum extensibility (LME). Placing a fusiform excision parallel to the RSTLs will thus simultaneously provide maximal tissue extensibility to close the wound and minimal tension while healing, resulting in an optimal scar.
Another critical factor in camouflaging a surgical recon-struction is the quality of skin used to close the defect. Repairs are most effectively hidden when the texture and thickness of the skin closing the defect closely matches the surrounding skin, thus de-emphasizing any border between the two. For this reason, simple, side-to-side closures, where the tissue that slides over the defect is the neighboring skin, are often aesthetically ideal. In contrast, skin grafts, which are taken from distant, often poorly matching tissues, often demonstrate conspicuous “patch” appearances with obvious borders. Flaps are best designed using skin from the same aesthetic unit, which is most similar in thickness and texture; this also avoids crossing junction lines into neighboring units.
METHODS OF CLOSURE
Granulation (Second Intent Healing)
Some defects of the periocular area can be allowed to granulate with good functional and cosmetic results. In general, smaller wounds on concave surfaces can achieve excellent cosmetic results through granulation.6 In the periocular area, the concave profile of the medial canthus (and in some cases the lateral canthus) lends itself well to second intention healing, with one caveat. Wounds undergo significant contraction with granulation, and they should be monitored during this time to ensure that ectropion or epicanthal webbing does not occur. Contraction begins around the third postoperative day and rapidly progresses through an exponential phase until the completion of wound contraction, after which any remaining defect heals by scar deposition and reepithelialization.6 One recent study showed that wounds in the medial canthal area contracted approximately 78% when allowed to heal by second intent.6 Although such significant contraction means that the final scar will be significantly smaller then the original defect, the contraction can also significantly distort nearby free margins and anatomic landmarks such as the canthal angle. Pericanthal wounds selected to heal by granulation should be small (ideally less than 1 cm in diameter) and distributed equally above and below the canthus in order to minimize the chance of canthal displacement during wound contraction. Second intent healing in other periocular subunits gives variable results and has more risk for lid retraction and ectropion.6 Although some patients prefer the simplicity of second intent healing over primary surgical repair, several weeks of compliant daily wound care may be required. In debilitated patients or those with limited capability to monitor and clean the wound, primary repair is typically a better choice.
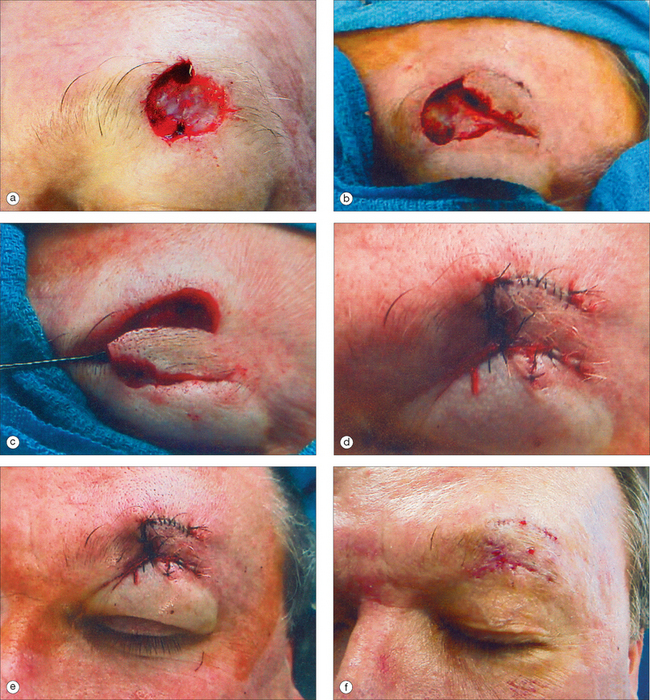
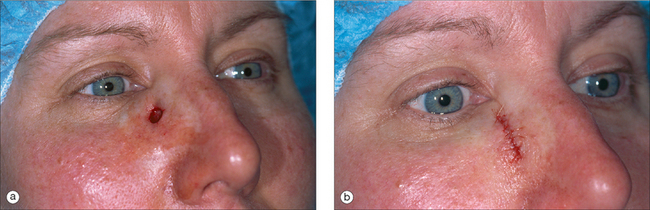
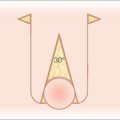
Side-to-Side Closure
The simplest method of wound repair for small to medium-sized periocular surgical defects is usually side-to-side closure. This often requires removal of adjacent redundant tissue to convert the circular defect into a fusiform shape to facilitate closure. The orientation of the ellipse should be designed to fall within or parallel to a wrinkle line, contour line, or RSTL. Since tissue is shifting (some classify large side-to-side closures as “sliding” flaps), care must be taken to avoid tension on free margins (eyelids, canthi) and landmarks (eyebrow, hairline). Since adjacent tissue moves perpendicularly to the long axis of a fusiform defect in side-to-side closure, the traction on the eyelid is maximal when the ellipse parallels the lid margin (Figure 12.6). Larger wounds (which necessitate more movement by adjacent tissues) and wounds closer to the lid margin provide greater risks of unacceptable traction on the lid. Therefore, the vectors of wound closure tensions should be parallel to the lid margin. The most direct way to do this, of course, is to orient the ellipse perfectly perpendicular to the lid.18 Since it is cosmetically preferable to orient the majority of the ellipse within wrinkles and other lines, one compromise is to curve the tip of the fusiform defect as it approaches the lid margin to be perpendicular to the margin near its border. In defects that diagonally approach the lid, sutures should be oriented parallel to the lid margin, rather than perpendicularly across the elliptical wound, to avoid unnecessary vertical tension on the lid. This closure technique may create slightly more redundant tissue (“dog-ear”) than placing sutures perpendicularly across the wound, but the prevention of tension on the lid margin is more important. Any resultant dog-ear can be “pushed” inferiorly through suturing technique and be subsequently removed away from the lid (inferiorly or laterally). Modified ellipses, such as the m-plasty technique, can also be used to shorten the length of the incision to avoid free margins and landmarks.7–10
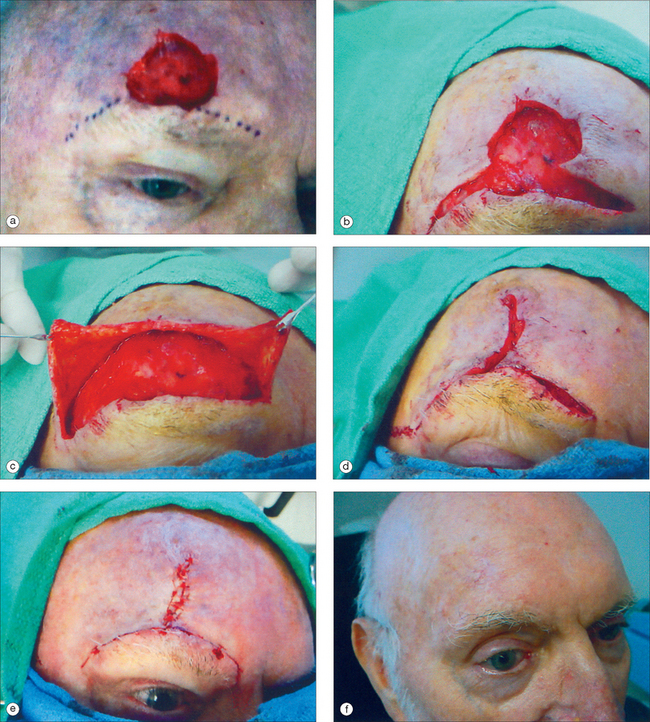
Skin Flaps
Functionally and cosmetically, local skin flaps are often superior to grafts for several reasons. Flaps retain their own blood supply, are less likely to undergo ischemic necrosis, and are more resistant to wound infection.11 Flaps undergo less contraction than FTSGs, and they often have better color and texture matches because of their origins within adjacent skin. Adnexal structures usually survive well in periocular flaps and contribute to texture matches with the surrounding skin. However, flaps can be more technically difficult, and their successes are a function of how well they are executed.
Most importantly, the surgeon should choose flaps that avoid tension on free margins and surface landmarks. With advancement and rotation flaps the “secondary movement,” which occurs opposite the primary movement of the flap, must be anticipated in order to minimize free margin displacement. With large flaps in this area, it is often necessary to use periosteal anchoring sutures to hold the weight of the flaps and minimize downward pull on the eyelid. In transposition flaps, maximal tension typically results from closing the secondary defect. A thorough understanding of the lines of maximal tension is important for successful execution of flaps in the periocular area.11 Regardless of flap selection, the surgeon should prospectively envision the tension vectors that will be created by secondary movement and should test for adequate tissue extensibility using a thumb and forefinger (“pinch test”) prior to cutting any flap.
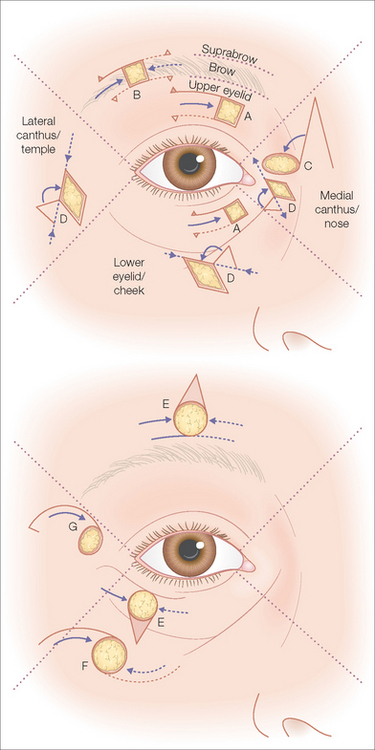
APPROACH TO RECONSTRUCTION BY PERIOCULAR SUBUNITS
From a reconstructive perspective, it is useful to divide the periocular area into six aesthetic subunits2 and consider each unit separately (Figure 12.7). Each subunit has its own contour, skin thickness, surface quality, danger zones, free margins, and surface landmarks that must be considered when choosing repair options. A great number of periocular flaps have been described, and all are not included here. Instead, some of the more commonly used flaps are highlighted (Figure 12.8) and pertinent operative points are briefly mentioned. Many larger and more complicated flaps are variations on these few examples. Several excellent reviews discuss the execution of these flaps in more detail.7,10,11
Lower Eyelid/Cheek Subunit
The lower eyelid subunit is a challenging area for reconstruction, as repairs here produce higher risks of lid malposition and ectropion. Fusiform side-to-side closures can be hidden along the RSTLs, but as the size of the primary defect and the proximity to the lid margin increases, so does the risk of ectropion. In larger defects, flaps often provide more options to alter the vectors of tension and avoid pull on the lid margin. Ectropion can be a direct result of inappropriate flap design and the resulting tension vectors that pull the lid inferiorly. However, even in properly designed and executed repairs, the weight of temporary postoperative edema and expansion of soft tissue at the lid margin can contribute to the development of ectropion.
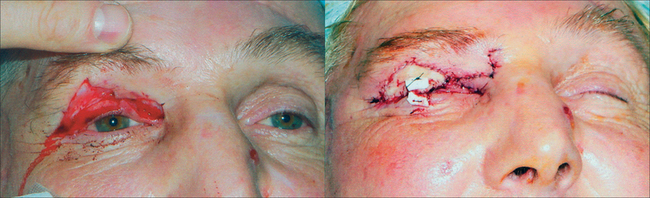
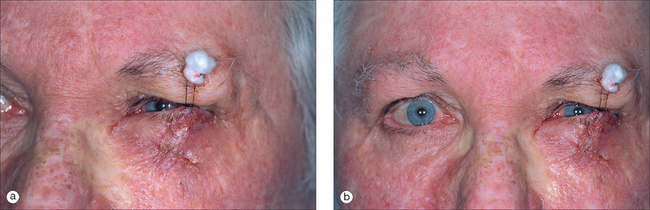
A special maneuver designed to counteract these temporary gravitational forces is the placement of a Frost suspension suture.18 Placement is straightforward: After completion of a flap or full-thickness skin graft that lies close to the lid margin and raises concern for tension, a suture is passed through the tarsus of the lower lid. Both ends of the suture are then attached to the overlying brow to create a suspension sling. The suture can be anchored at the brow with tape or sutured over a cotton bolster (Figure 12.17). Any type of suture may be used, and 4-0 nylon is an acceptable choice. Although some authors suggest placing the lid in its normal anatomic position, the lid may also be suspended slightly superior to its normal position to ensure there is no unwanted downward tension on the lid margin during healing. The suture placement through the tarsus and the anchoring points at the brow should be positioned so that vision is not obstructed and the cornea is not traumatized. Although the palpebral fissure will obviously be narrowed, the patient should still be able to see out of the eye in forward gaze. The suture is removed in 5–7 days, or as soon as most of the postoperative edema has resolved and thus reduced the risk of ectropion. Most importantly, the purpose of the suspension suture is not to correct an ectropion present at the time of closure (from improperly placed tensional forces) but rather to prevent it (by counteracting transient gravitational forces from edema).
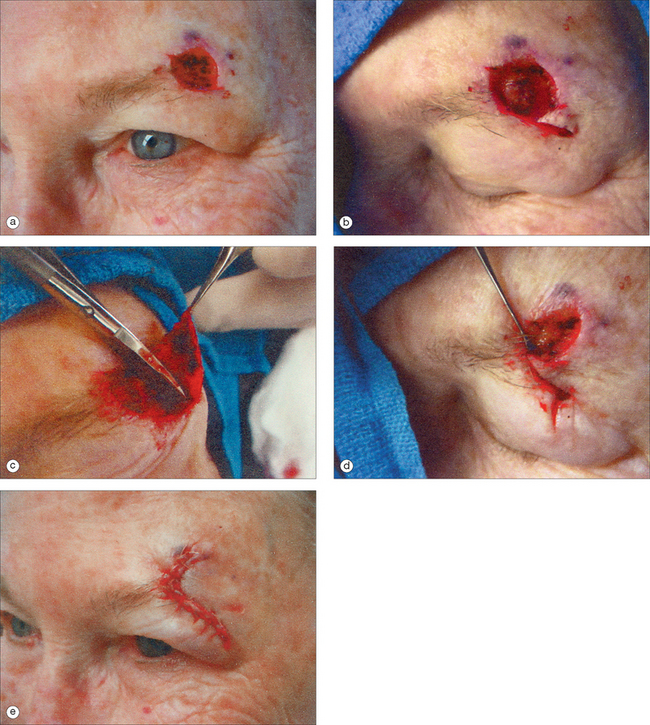
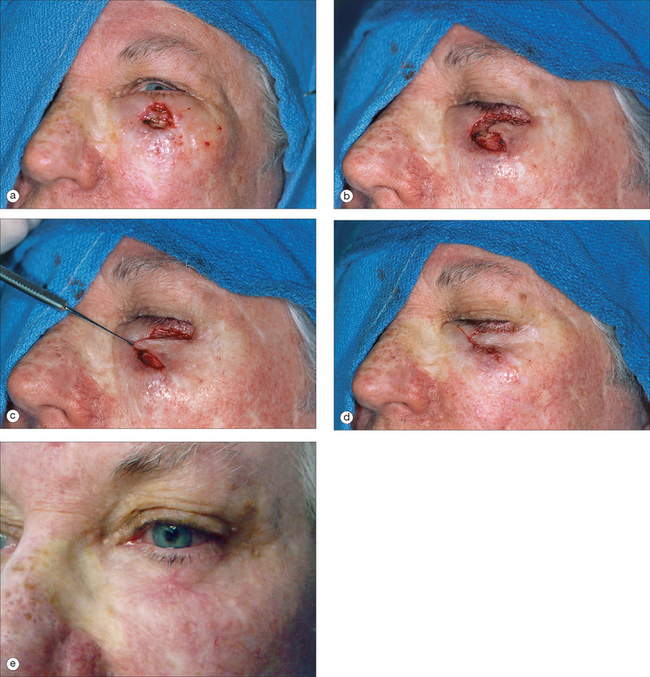
Lateral Canthus/Temple Subunit
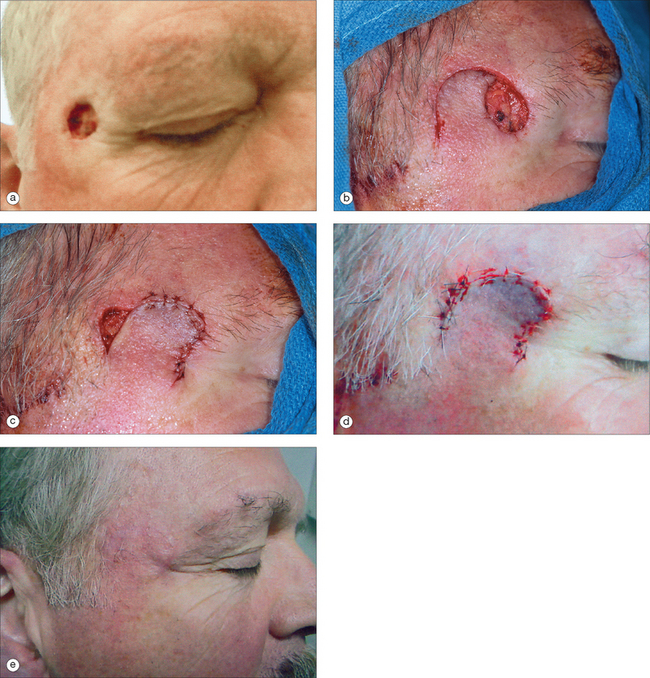
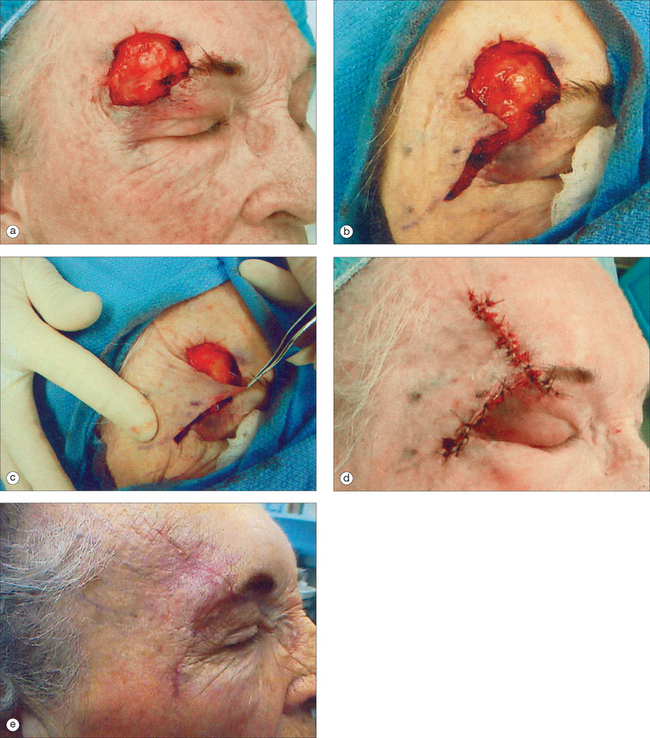
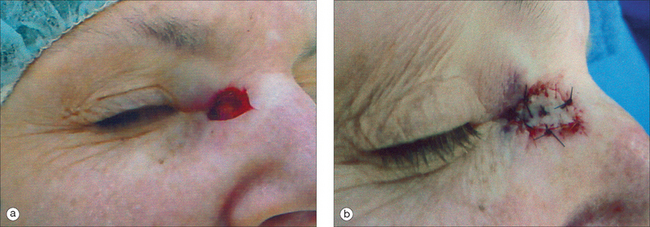
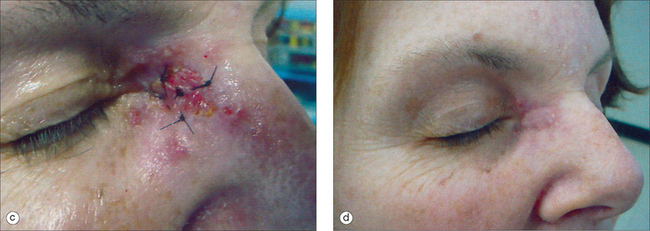
Figure 12.19 (a) Small circular defect of the right temple after Mohs micrographic surgery. Although this defect is smaller than the one in Figure 12.18, it is slightly more inferior and closer to the lateral canthus. (b) In contrast to the side-to-side repair in Figure 12.18, this rotation flap design will keep the repair within the temple, away from the lateral canthus and the anterior view of the face. Lateral placement of the incision will conceal any long-term scar from the anterior view, and the wide pedicle and inferior drainage of the flap result in a predictably excellent cosmetic result in most cases. (c) Closing the “primary” defect first helps to ensure the flap is positioned to most effectively minimize tension on the eyebrow, upper eyelid, and lateral canthus. Then zipping the “secondary” defect closed from anterior to posterior serves to push the closure laterally, away from the central face, so that any standing cones can be removed along the hairline. However, the long curving incision usually allows the secondary defect to be gradually sutured out such that no “dog-ear repair” is needed. (d) Immediately after repair. (e) Surgical result 3 months postoperatively.
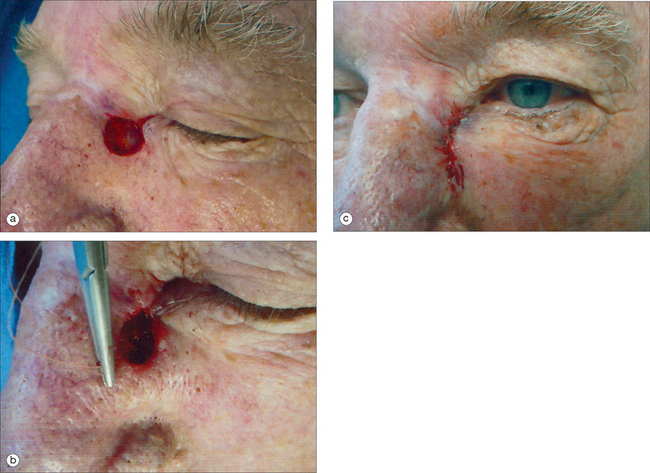
Medial Canthus/Nose Subunit
The medial canthal area can be a difficult area to reconstruct, and there are multiple repair options for defects in this area. Because of its concave profile, the medial canthus is the most appropriate periocular subunit for second intent healing. Wound contraction can displace the canthus, however, so wounds optimally suited for granulation should extend evenly above and below the canthus. Canthal webbing can also be a distracting problem, and it should be avoided when reconstructing the area with cutaneous flaps. The glabellar area often has sufficient donor skin to contribute a transposition flap, as does the nasal sidewall and upper medial cheek. When designing a transposition flap, it is important to make certain that the tension vector used to close the secondary defect does not displace the eyelid or canthus.
COMPLICATIONS
In addition to the familiar complications that can occur with any surgical procedure in any anatomical site—wound dehiscence, infection, hematoma, and tissue necrosis—special complications may arise in the periorbital area. Probably the most unfortunate late “complication” of periocular excisional surgery is the recurrence of a malignant tumor. Several studies describe increased recurrence rates for malignancies in this area, due to early deep invasion and inadequate resection margins.13,14 Mohs micrographic surgery is an especially valuable approach to tumors in this region, as it is the most likely method to achieve complete tumor extirpation while preserving the maximal amount of normal periocular tissue.15 Recurrent periocular tumors can destroy the intricate structures of the eye, endanger vision, invade the bony orbit, and even extend into the brain.
The free margins of the upper and lower eyelids must be monitored when reconstructing defects (and during wound contracture of second intent healing) to ensure eyelid malposition does not occur. Because of gravity, malposition of the lids is more common in the lower than in the upper eyelids, and it can be graded as mild when there is slight eversion of the eyelashes with or without scleral show, moderate when there is eversion and descent of the lid margin with scleral show, and severe when frank ectropion is present.5 Ectropion is eversion of the eyelid margin away from the globe, which exposes the conjunctival mucosa and can lead to exposure keratopathy. These complications can usually be avoided with appropriate preoperative evaluation and surgical technique. Multiple factors, including mechanical tension, gravity, wound edema, preexisting lid laxity, and scar contraction, can contribute to postoperative ectropion. Inappropriately directed wound closure tensions are the most common and the most preventable reasons for postoperative ectropia.
Prior to surgery, several simple tests can be performed to identify patients who already have lower eyelid laxity and are therefore at increased risk of developing lid malposition (Table 12.1). First, with the patient sitting up and in primary gaze (looking straight ahead with the head in a normal horizontal position) any amount of “scleral show” should be measured. Ideally, the lower eyelid will overlie the inferior limbus (edge of the cornea) by about 1 mm.16 If the lid lies below this, the white sclera inferior to the cornea is exposed, which should raise suspicion for eyelid laxity. Patients with more than 1 mm of scleral show often demonstrate significant lid laxity.16 Second, lid resilience can be evaluated with the patient sitting up. In the lid retraction (“snap back”) test, the skin of the lower eyelid is grasped between the thumb and forefinger, pulled inferiorly away from the globe, and released. An abnormal result is delayed return to the globe surface or return only after blinking or manipulation.17 Alternatively, in the lid distraction test, the distance that the lower lid can be manually displaced inferiorly from the globe is measured, with distances of 8 mm or more indicating laxity.16 Although not every patient with lid laxity will inevitably develop an ectropion after periorbital surgery, these high-risk patients should have reconstructive procedures that are carefully chosen and executed in this area so that lid malposition is avoided. Alternatively, patients who demonstrate significant lid laxity may benefit from a horizontal lid-tightening procedure in conjunction with repair of the surgical defect.
| EVALUATION | MEASUREMENT | INCREASED RISK OF LAXITY IF |
|---|---|---|
| “Scleral show” measurement | Vertical exposure of sclera (inferior limbus to lower lid margin) | >1-mm exposure |
| Lid retraction (“snap back”) test | Speed of lid returning to globe surface after being manually pulled away and then released | Delayed return to the globe surface or return only after blinking or manipulation |
| Lid distraction test | Distance lid can be manually displaced from globe | Displacement ≥8 mm |
| Maximal tension (“yawn”) test | Observe lower lid margin as patient opens eyes and mouth widely and directs gaze upward | Lid margin pulls away from globe |
During reconstruction, it is important to frequently check for tension on the lower eyelid margin as a result of tissue movement. The saying that “the lower eyelid begins on the upper lip” illustrates that movements of the facial musculature and mandible can contribute to functionally important tension on the lower lid. Intraoperatively, a test for lid laxity that demonstrates this transmission of tensional forces during animation can be employed. The patient is asked to open the eyes widely and look toward the top of the head while simultaneously opening the mouth widely (this is called the maximal tension or “yawn” test) (Figure 12.24). This maneuver will maximally stretch the lower eyelid skin and reveal any tension on the lid margin that might otherwise be inapparent until after the completion of the surgical procedure. Ideally, the lid should remain snugly opposed to the globe during this maneuver. While this yawn test can be useful for evaluating a patient during surgical repair, it should also be performed postoperatively, while the patient is sitting upright, to fully account for any gravitational effects on lid positioning.
Knowledge of the lymphatic drainage pattern of the periocular area is important when designing flaps. Inferiorly based flaps are often preferred to avoid the potential pincushion or “trapdoor” deformity that may partially result from trapped edema. In the periocular area, persistent lymphedema can similarly become a problem in the lower eyelid if there is significant disruption of the lymphatic system. Although many flaps involve horizontal incisions below the eyelid, those flaps that either extend around the lateral canthus and along much of the infraorbital area or are incised at a deep plane are especially prone to developing persistent edema.18
1 Sherris DA, Heffernan JT. Techniques in periocular reconstruction. Facial Plast Surg. 1994;10:202-213.
2 Larrabee WF, Sherris DA. Principles of Facial Reconstruction. Philadelphia: Lippincott-Raven, 1995.
3 Seckel BR. Facial danger zones: avoiding nerve injury in facial plastic surgery. St. Louis, MO: Quality Medical Publishing, 1994;12-17.
4 Cheney ML, Bilyk JR. Surgical anatomy of the face. In: Cheney ML, editor. Facial surgery: plastic and reconstructive. Hong Kong: Williams and Wilkins; 1997:17-51.
5 Jelks GW, Jelks EB. Prevention of ectropion in reconstruction of facial defects. Clin Plast Surg. 2001;28:297-302.
6 Mott KJ, Clark DP, Stelljes LS. Regional variation in wound contraction of Mohs surgery defects allowed to heal by second intention. Dermatol Surg. 2003;29:712-722.
7 Patrinely JR, Marines HM, Anderson RL. Skin flaps in periorbital reconstruction. Surv Ophthalmol. 1987;31:249-261.
8 Becker FF. Reconstructive surgery of the medial canthal region. Ann Plast Surg. 1981;7:259-268.
9 Jewett BS, Shockley WW. Reconstructive options for periocular defects. Otolaryngol Clin N Am. 2001;34:601-625.
10 Borges AF. Pitfalls in flap design. Ann Plast Surg. 1982;9:201-210.
11 Wiggs EO. Periocular flaps. J Dermatol Surg Oncol. 1992;18:1069-1073.
12 Desciak EB, Eliezri YD. Surgical pearl: Temporary suspension suture (Frost suture) to help prevent ectropion after infraorbital reconstruction. J Am Acad Dermatol. 2003;49:1107-1108.
13 Reim M, Quinkler G. Complications of lid surgery. Dev Ophthal. 1987;13:1-8.
14 Spector JG. Surgical management of cutaneous carcinomas at the inner canthus. Laryngoscope. 1985;95:601-607.
15 Mohs FE. Micrographic surgery for the microscopically controlled excision of eyelid cancers. Arch Ophthalmol. 1986;104:901-909.
16 Shagets FW, Shore JW. The management of eyelid laxity during lower eyelid blepharoplasty. Arch Otolaryngol Head Neck Surg. 1986;112:729-732.
17 Koch RJ, Hanasono MM. Aesthetic facial analysis. In: Papel ID, editor. Facial plastic and reconstructive surgery, 2nd edn. New York: Thieme; 2002:135-144.
18 Custer PL. Conceptual approach to eyelid reconstruction. Otolaryngol Clin N Amer. 1990;23:991-1002.