Chapter 31 Pericardial Disease (Pericarditis and Pericardial Tamponade)
2 Why do hemodynamic changes occur with the buildup of fluid between the layers of the serous pericardium?
9 How is pericardiocentesis used in diagnosing or treating acute pericarditis?
Pericardiocentesis or surgical drainage should be performed for one of three reasons:
11 How is therapy decided for treatment of acute pericarditis?
Treatment is based on the cause of acute pericarditis as follows:
 Neoplastic: Drainage if hemodynamic compromise, and appropriate chemotherapy.
Neoplastic: Drainage if hemodynamic compromise, and appropriate chemotherapy.
 Viral: Symptomatic and supportive care.
Viral: Symptomatic and supportive care.
 Autoimmune: Nonsteroidal antiinflammatory drugs (NSAIDs) are the mainstay of treatment (class I); corticosteroids may be used if refractory to NSAID therapy.
Autoimmune: Nonsteroidal antiinflammatory drugs (NSAIDs) are the mainstay of treatment (class I); corticosteroids may be used if refractory to NSAID therapy.
 Bacterial or TB: Antibiotics as appropriate by blood or pericardial fluid culture.
Bacterial or TB: Antibiotics as appropriate by blood or pericardial fluid culture.
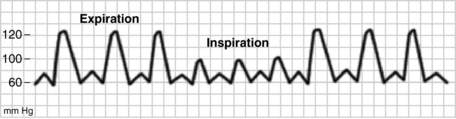
18 What is the differential diagnosis in a patient with pulsus paradoxus by arterial line tracing?
Sensitivity and specificity are 79% and 40% for tamponade. Always use clinical suspicion when diagnosing this or other life-threatening conditions. See Figure 31-1.
19 How is pericardial tamponade diagnosed?
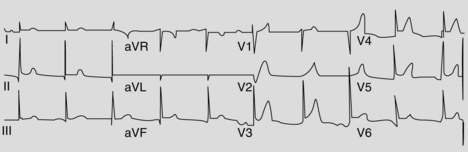
Tamponade is a clinical diagnosis based on history and physical examination results. It usually represents an emergency and can lead to pulseless electric activity (PEA) cardiac arrest if left undiagnosed and untreated. Some common features include jugular venous distention with increased CVP (Kussmaul sign), faint heart sounds, sinus tachycardia, and pulsus paradoxus. If one is unsure of the diagnosis, some studies are helpful in diagnosis. The ECG may demonstrate electrical alternans or sinus tachycardia with low-voltage QRS complexes. Chest radiograph may show an enlarged cardiac silhouette. Echocardiography is extremely useful in diagnosis of this condition and has been given a class I recommendation. On echo, right atrial collapse is more sensitive but less specific than RV collapse. If tamponade is highly suspected, one should not wait for an echo before instituting therapy. See Figure 31-2.
20 Briefly describe the hemodynamic strategy in a patient with suspected pericardial tamponade
The hemodynamic strategy consists of “fast, full, and tight.”
 Fast means allow the patient to have tachycardia (no β-blockers, please).
Fast means allow the patient to have tachycardia (no β-blockers, please).
 Full means to increase preload (fluids wide open).
Full means to increase preload (fluids wide open).
 Tight indicates treatment that allows the patient’s blood pressure to rise either by volume resuscitation or with vasopressors (norepinephrine, epinephrine, or phenylephrine) as indicated.
Tight indicates treatment that allows the patient’s blood pressure to rise either by volume resuscitation or with vasopressors (norepinephrine, epinephrine, or phenylephrine) as indicated.
1 Benumof J. Anesthesia and Uncommon Diseases, 4th ed. Philadelphia: Saunders; 1998.
2 Moore K. Clinically Oriented Anatomy, 3rd ed. Philadelphia: Williams & Wilkins; 1992.
3 Murray M., Coursin D., Pearl R., et al. Critical Care Medicine—Perioperative Management, 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2002.