62 Pelvic Fixation of the Aging Spine
KEY POINTS
Introduction
Reliable fixation to the pelvis was first achieved in the 1970s with Luque instrumentation which utilized a bar with a curved distal end that could be advanced into the iliac crest. A decade later, the Galveston method was introduced, which provided even greater fixation because it allowed for the application of contoured rods, which were inserted though the posterior superior iliac spine, in between the inner and outer tables of the pelvis, toward the sciatic notch. Nevertheless, these early systems were still found to give rise to an relatively high incidence of pseudarthrosis, ranging from 6% to 41%.1
Iliac screws improve on these initial approaches by taking advantage of innovations in implant design and modularity. These constructs are not only more rigid; their pull-out strength has been shown to be three times greater than that of a standard Galveston rod.2 Given their superior biomechanical properties, it is anticipated that the use of iliac screws may reduce the risk of pseudarthrosis compared to other types of lumbosacral constructs. However, the proper placement of this instrumentation requires an intricate knowledge of pelvic anatomy in order to avoid cortical breaches through the ileum or penetration into the acetabulum.3 Furthermore, the surgeon must also take into account the position of the screws for the purpose of contouring the rod and ensure adequate soft tissue coverage to ensure the heads will not be too prominent, which could contribute to patient discomfort.4
Case Studies
Clinical Case #1—Degenerative Scoliosis
Posteroanterior and lateral scoliosis x-rays display a right thoracic curve from T5 to T11 and a left lumbar curve from T11 to L4, measuring 58 degrees and 67 degrees, respectively (Figure 62-1). However, her overall coronal and sagittal alignment appears to be reasonably balanced. These films demonstrate clear progression compared to previous radiographs acquired several years ago. Aside from her deformity, an MRI study of her entire spine reveals no intraspinal abnormalities or significant compression of the neural elements.
Clinical Case #2—Pathologic Fracture
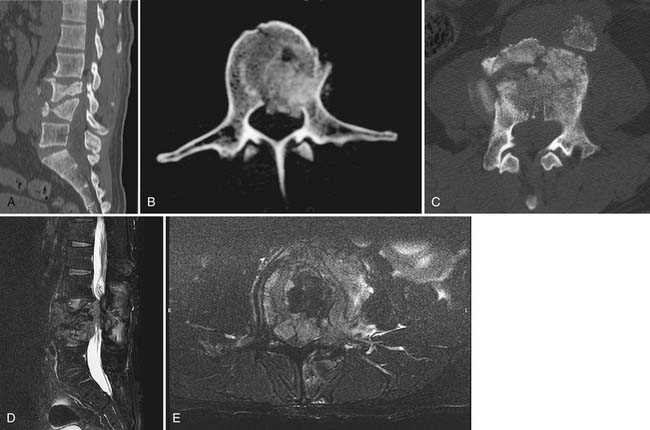
Imaging studies include plain films of the lumbar spine, which demonstrate L3 and L4 vertebral body fractures (Figure 62-2). These fractures were confirmed to be burst-type injuries on a subsequent CT scan with obvious height loss, focal kyphosis, and retropulsion of fragments with approximately 25% canal compromise. An MRI study displays a large soft tissue mass extending into the epidural space at these levels, which results in significant spinal stenosis with near-obliteration of the thecal sac.
Basic Science and Biomechanical Studies
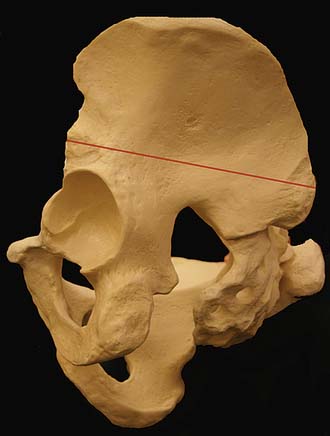
A thorough understanding of the osseous and soft tissue anatomy of the lumbosacral spine and pelvis is critical for the safe and effective insertion of iliac fixation. The sacrum is composed of five fused vertebrae and serves as a functional keystone that links two paired hemipelves posteriorly through bilateral sacroiliac articulations. Because this instrumentation is introduced into the iliac wings, which form the lateral borders of the pelvic ring, it is necessary to consider a number of different parameters such as intrailiac distance, width between the inner and outer tables, and cortical thickness. The longest intrailiac path proceeds along a line connecting the posterior superior iliac spine to the anterior inferior iliac spine, which averages approximately 141 mm in males and 129 mm in females. Similarly, the width of the iliac crest should allow for the placement of 8-mm screws in males and 6- to 7-mm implants in females; the mean cortical thickness in males and females has been shown to be 5.2 mm and 4.7 mm, respectively.3
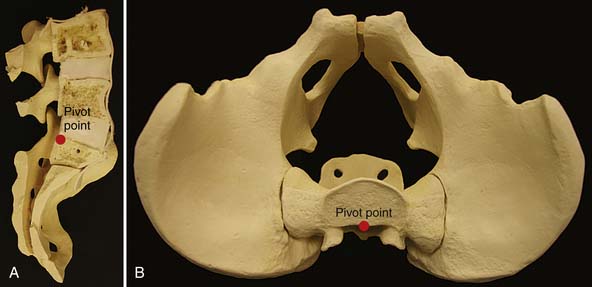
In their comparison of 10 different methods of lumbosacral fixation, McCord and colleagues5 reported that the two constructs associated with the highest loads to failure both obtained solid purchase within the iliac crests. Based on this in vitro data, the concept of the lumbosacral pivot point was elucidated, which is located at the intersection of the middle osteoligamentous column and the L5-S1 interspace (Figure 62-3). According to this paradigm, pelvic implants that extend anterior to this fulcrum increase the overall stiffness of the instrumentation because the resultant biomechanical vectors are transformed from in-line forces to cantilever bending.6
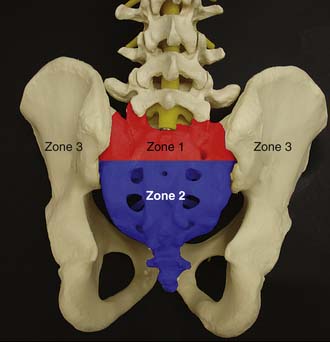
Three distinct zones have been designated for the purpose of categorizing sacropelvic fixation (Figure 62-4).7 Zone 1 refers to the S1 vertebral body, Zone 2 encompasses the sacral alae and the region between S2 and the coccyx, and Zone 3 denotes the paired iliac wings. In general, the degree of stability imparted by these screws has been found to improve as they are positioned more laterally within the lumbopelvic ring (i.e., from Zone 1 to Zone 3); implants situated in Zone 3 are also better able to resist the pull-out forces that are generated by bending moments arising from the lumbosacral junction than those directed toward either Zone 1 or 2.
The use of internal fixation in the setting of osteoporosis may be particularly problematic because this instrumentation is likely to be more susceptible to loosening or failure, especially in cases involving traumatic injuries or deformity correction where it may be subjected to tremendous stresses and strains. Consequently, in these situations it may be preferable to employ longer implants that will traverse the entire length of the iliac column and engage the cortical bone superior to the acetabulum, so that they are able to withstand more significant forces.2 Another approach that has been advocated for osteoporotic patients is the incorporation of two screws into each iliac crest. However, there are some concerns that the application of rigid iliac fixation could lead to stress shielding of an already compromised pelvis, which may predispose these individuals to insufficiency fractures.8
Clinical Case Examples: Treatment and Future Challenges
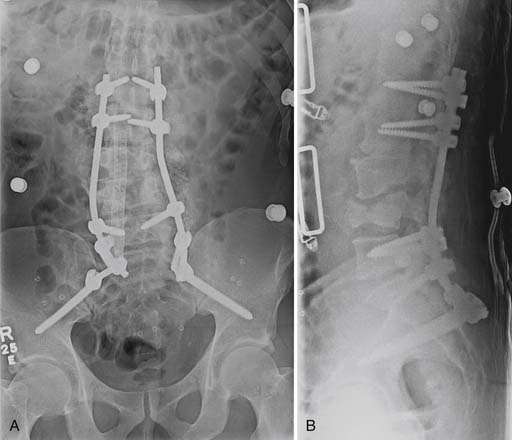
Both of the cases presented earlier involved posterior-based spinal constructs that were reinforced with pelvic implants. The first patient with degenerative scoliosis underwent a circumferential procedure performed in a staged fashion consisting of anterior releases and interbody fusions from L2-S1 with polyetheretherketone (PEEK) cages followed by a posterior spinal arthrodesis extending from T5 to the ileum with instrumentation and autogenous bone (Figure 62-5). In the second case example, the pathologic fractures of the L3 and L4 vertebral bodies were addressed with a posterior decompression of those levels, in conjunction with an instrumented fusion of the motion segments between L1 and the pelvis with local and iliac crest autograft (Figure 62-6). In both of these situations the decision was made to include supplemental pelvic fixation because such extensive constructs would be expected to subject the distal screws to substantial forces that may bring about hardware failure or loosening, especially in these individuals who were suspected of having osteoporosis. Thus the purpose of adding pelvic implants was to augment the rigidity of the instrumentation and create a more stable, “balanced” construct that would hopefully reduce the incidence of pseudarthrosis.
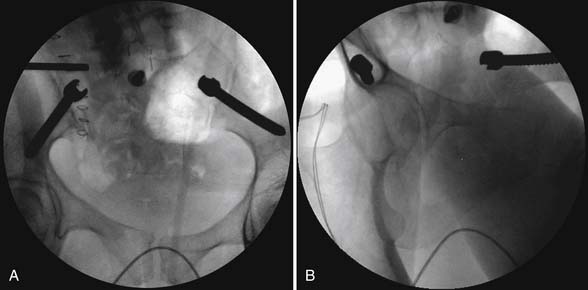
In placing pelvic screws, it may be useful to remove a portion of the posterior superior iliac spine with a Leksell rongeur or burr so that the heads may be adequately countersunk in an attempt to minimize their prominence. The probe is introduced into the window of cancellous bone and aimed between the inner and outer tables of the ileum, toward the sciatic notch (Figure 62-7). After the tract is probed for any cortical breaches, the cavity is tapped in preparation for the instrumentation; in most instances the dimensions of the iliac wing should be able to accommodate relatively large implants (i.e., 7.5 mm in diameter and up to 80 mm in length or greater). The final position of the pelvic screws should be assessed with intraoperative radiographs or fluoroscopy in AP, lateral, and oblique views to ensure that it is entirely contained within the ileum and is not encroaching upon other critical structures, such as the hip joint (Figure 62-8).
Conclusion
Pelvic fixation represents an effective method for enhancing the rigidity of posterior spinal fusion constructs. By obtaining secure purchase within the iliac crests, these implants confer greater stability to the axial skeleton and may therefore be indispensable for the treatment of patients with osteoporosis who are at greater risk for nonunion and other postoperative complications following complex spinal reconstructions.
1. Moshirfar A., Rand F.F., Sponseller P.D., Parazin S.J., Khanna A.J., Kebaish K.M., Stinson J.T., Riley L.H. Pelvic fixation in spine surgery. Historical overview, indications, biomechanical relevance, and current techniques. J. Bone Joint Surg. Am.. 2005;87:89-106.
2. Schwend R.M., Sluyters R., Najdzionek J. The pylon concept of pelvic anchorage for spinal instrumentation in the human cadaver. Spine. 2003;28:542-547.
3. Schildhauer T.A., McCulloch P., Chapman J.R., Mann F.A. Anatomic and radiographic considerations for placement of transiliac screws in lumbopelvic fixation. J. Spinal Disord. Tech.. 2002;15:199-205.
4. Acharya N.K., Bijukachhe B., Kumar R.J., Menon V.K. Ilio-lumbar fixation—the Amrita technique. J. Spinal Disord. Tech.. 2008;21:493-499.
5. McCord D.H., Cunningham B.W., Shono Y., Myers J.J., McAfee P.C. Biomechanical analysis of lumbosacral fixation. Spine. 1992;17(Suppl. 8):S235-S243.
6. Santos E.R., Rosner M.K., Perra J.H., Polly D.W. Spinopelvic fixation in deformity: a review. Neurosurg. Clin. N. Am.. 2007;18:373-384.
7. O’Brien M.F. Sacropelvic fixation in spinal deformity. In: DeWald R.L., editor. Spinal deformities: the comprehensive text. New York: Thieme; 2003:601-614.
8. Wood K.B., Schendel M.J., Ogilvie J.W., Braun J., Major M.C., Malcom J.R. Effect of sacral and iliac instrumentation on strains in the pelvis: a biomechanical study. Spine. 1996;21:1185-1191.