CHAPTER 76 PEDIATRIC TRAUMA
Pediatric trauma is the number one killer of children. It is also the number one cause of permanent disability in this population. It has often been said that children are not merely small adults, and this is never more accurate than in pediatric trauma. Although the principles of trauma care are the same for children as for adults, the differences in care required to optimally treat the injured child do require special knowledge, careful management, and attention to the unique physiology and psychology of the growing child or adolescent.
MECHANISMS OF PEDIATRIC TRAUMA
The mechanism of injury and mortality in children has remained remarkably consistent. In children over 1 year and under 14 years, motor vehicle–related mortality remains the greatest killer of children, at 46.5% of all causes (2002).1 Drowning is the second cause, followed by burns. A detailed view of mortality statistics reveals the home as an area of continuing concern. Other areas of concern include falls and bicycle-related injuries; a growing area of death and disability now includes all-terrain vehicle (ATV) crashes.2
INITIAL ASSESSMENT, STABILIZATION, AND MANAGEMENT OF INJURED CHILD
Airway Management
Most children do not have pre-existing pulmonary disease; therefore, an oxygen saturation of greater than 90% on room air is often proof of adequate pulmonary function. If oxygenation is difficult, then a lung injury, pneumothorax, or aspiration should be considered. Hypoventilation is common in the presence of a head injury or shock. If any of these conditions exist, intubation is appropriate. Respiratory compromise requiring intubation commonly indicates a very severe injury. While no criteria have been validated to determine what constitutes a “major resuscitation” in children, intubation and airway compromise have been shown to suggest a population that has a higher incidence of mortality compared with injured children who do not have airway issues.3 As with all patients, care should be taken to avoid cervical spine motion during intubation. It should be noted that nasotracheal intubation is generally not used in small children in the emergency setting.
The need for emergency airway access for acute pediatric airway obstruction is a very uncommon event. If needed, a 14- or 16-gauge angiocatheter may be placed through the cricothyroid membrane, or even the tracheal wall. Care should be taken to avoid penetrating the posterior tracheal membrane. Oxygen can then be administered through the catheter, allowing time for attempts at intubation. This technique, although rarely required, may be followed by tracheotomy or cricothyroidotomy. It should be noted that a cricothyroidotomy in a child may lead to subglottic stenosis and should be avoided.
Vascular Access
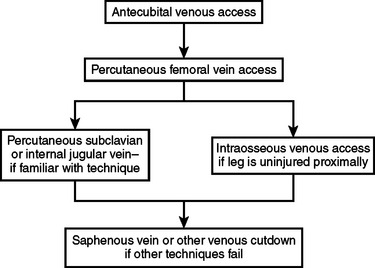
The ideal initial sites for vascular access in children are the peripheral veins in the upper extremities, especially the antecubital fossa. If access cannot be achieved in these vessels, central venous access may be employed (Figure 1). A percutaneous femoral venous catheter is the next best choice and the most commonly used route for emergency venous access in the child. This should be done without attempting a cut-down, preferably using the Seldinger technique. Surgeons familiar with subclavian catheterization in the child may utilize this route as the next choice.4 For surgeons comfortable with this technique in children, complications are rare. Intraosseous access is acceptable in injured children. Contraindications include proximal fractures and sites of infection nearby. The anteromedial surface of the proximal tibia is used, 2–4 cm distal to the tibial tuberosity. For insertion in the proximal tibia, the needle is directed inferiorly at a 45-degree angle from the perpendicular. If the insertion site is the distal tibia, the needle should be angled 45 degrees superiorly. In both instances, the goal is to angle away from the region of the growth plate and/or joint. There are specialized needles readily available to use with this technique, but if these are not available, a spinal needle with a trochar may be employed. Multiple entries into the medullary cavity should be avoided, as the leakage that occurs with multiple attempts may cause a compartment syndrome. For surgeons not familiar with peripheral, central, or intraosseous access in children, a cut-down of the saphenous vein may be employed,5 although intravenous (IV) access by cut-down is no easier or faster than any of the abovementioned methods.
Circulatory Management
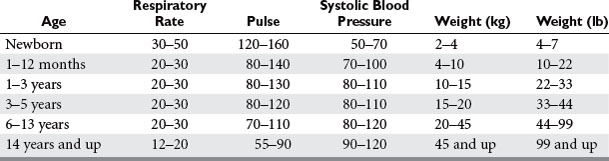
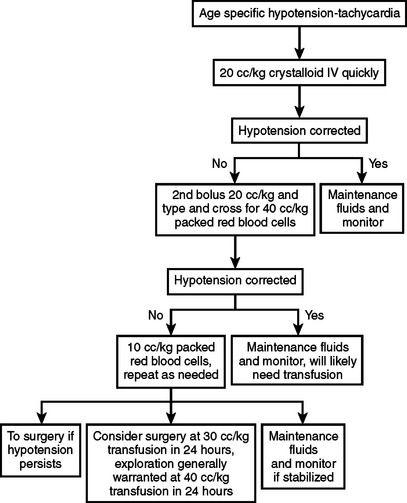
Age-specific hypotension is an indication for designating the necessity for major resuscitation in an injured child. In an analysis of the National Pediatric Trauma Registry, 38% of recorded deaths occurred in children whose systolic blood pressure was less than 90 mm Hg. This group represented 2.4% of the study population. To determine if a child has “age-specific hypotension” requires knowledge of normal blood pressures in children.6 New national guidelines for the ranges of normal childhood blood pressures based on age were published in 2004 (Table 1). A child with an injury that produces significant blood loss may present with a normal blood pressure. The otherwise healthy child can readily compensate for blood loss by mounting a significant tachycardia coupled with peripheral vasoconstriction. Therefore, a normal blood pressure in a child does not mean that circulating blood volume is at normal levels. A more accurate determination includes a blood pressure evaluation along with monitoring heart rate and assessing peripheral perfusion. Clinical signs of poor perfusion in conjunction with altered mentation are classic findings in pediatric hypovolemic shock. If these are present, then an immediate bolus of 20 cc/kg of isotonic crystalloid is in order. If a second bolus of this amount is needed, and there is little improvement, blood should be started immediately (Figure 2). Caution must be taken, as over-resuscitation may be as problematic as under-resuscitation, especially in the presence of a head injury. Enthusiastic administration of crystalloid solutions may exacerbate cerebral edema in certain circumstances. Overtreatment with crystalloid infusions may result in poor clot formation, worsening the compromised hemorrhagic state, and may have no impact on survival. Supranormal trauma resuscitation increases the likelihood of the abdominal compartment syndrome in adult trauma victims, and there are reports of the same problem in children.7 Typically, a bolus of 20 cc/kg of isotonic crystalloid in the presence of hypotension is the first treatment. If there is evidence of continuing instability, a second bolus of this amount may be given. If after two boluses of crystalloid the child does not have stable vital signs, blood should be started immediately. Type-specific packed red blood cells should be given, or O negative blood if necessary, in certain circumstances. Fresh frozen plasma and platelets should be considered early in the resuscitation period if large amounts of blood are needed for resuscitation. If there is a decreased level of consciousness without signs of hypovolemia, then modest fluid resuscitation is in order. Hypothermia is an extremely common occurrence in injured children. Hypothermia in the injured child may occur at any time of the year, even during the extremes of summer. The response to hypothermia includes catecholamine release and shivering, with an increase in oxygen consumption and metabolic acidosis. Hypothermia as well as acidosis contribute to a post-traumatic coagulopathy. Prevention and treatment of hypothermia require attention to this serious complication during the initial evaluation of the injured child. A warm room, warmed fluids, heated air-warming blankets, or externally warmed blankets should be utilized during the initial resuscitation. An aggressive approach to rewarming should begin in the emergency department and should be continued in the radiology suite during evaluation. There is some evidence to suggest that early, carefully controlled hypothermia in the severely head-injured child who has no other injuries may be beneficial, but this treatment option is still experimental.
Diagnostic Assessment
Several recent studies by adult and pediatric trauma surgeons have attempted to determine the role of focused acute sonography for trauma (FAST) in the evaluation of the injured child.8,9 The most common FAST evaluation examines the heart, right and left upper quadrants, and the pelvis for fluid (Figure 3). Some surgeons include an evaluation of the thorax for fluid in the pleural space and for pneumothorax.
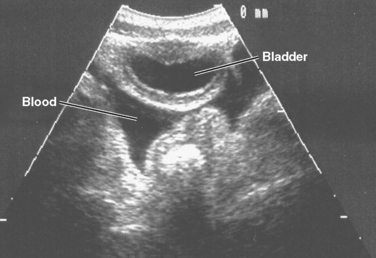
Figure 3 A positive focused acute sonography for trauma (FAST) in a 4-year-old. Blood in the pelvis.
Computerized tomography (CT) is the accepted diagnostic radiologic tool of choice for the vast majority of injured children suspected of having a potentially life-threatening injury.10 CT scans of the head, abdomen, and chest are considered the standard of care for the evaluation of an internal injury in a stable, traumatized child. The majority of children with suspected intra-abdominal injuries, providing they are stable, should have a CT scan performed prior to instituting operative or nonoperative management, unless an absolute indication for surgery is present. Physiologically unstable children in the emergency department are evaluated by other modalities, such as diagnostic peritoneal lavage or ultrasound. While CT scanning is the imaging modality of choice for evaluating a stable injured child, it is generally accepted that a high percentage of those scans will reveal no injuries. Abnormal abdominal CT scans are seen in only one-fourth of patients (Figure 4). A CT scan affects the decision to operate on children with a solid organ injury in a very small number of cases. Despite the liberal use of head CT scans, it is possible for the child with a severe neurologic injury to have a normal initial scan, or for a child to develop late manifestation of a neurologic injury or cerebral edema despite an initial normal study.
MANAGEMENT OF SPECIFIC INJURIES
Head and Central Nervous System Injury
Acute traumatic brain injury is the most common cause of death and disability in the pediatric population. In those who survive, minor injuries can be associated with reversible defects, while major injuries can result in severe disabilities. The mechanisms of head injury in children are related to age. Infants typically suffer more from falls, such as from a table or the arms of a care giver. Intentional injury is a common cause of death in children under 2 years. Injury with intention, independent of severity, raises the mortality in brain-injured children. In older children, the usual cause of head injuries is from vehicle-related accidents or recreational activities.11 While children have a better survival rate with head injury than adults do, this does not mean they have less morbidity with similar injuries. Children have a plasticity of the neuron related to the myelination and establishment of neuron interconnections. This allows a given focal injury to produce a less severe deficit as compared with a mature brain. But this same lack of maturity may also make the child more susceptible to a diffuse injury and subject to greater cognitive impairment.
During the initial evaluation and resuscitation of the braininjured child, care should be taken to avoid secondary brain injury due to causes such as hypotension and hypoxia.12 Control of the cervical spine is also mandatory during this period. Clinical and radiologic evaluation of the c-spine is important to rule out injury. The Glasgow Coma Scale (GCS) can be used for children over the age of 5, while some modification of the GCS is often used for children under 5. If a score of less than 9 is determined, that patient typically requires airway management, and intracranial pressure (ICP) measurement and treatment options should be considered. A score of less than 8 indicates the patient is comatose. Maintaining good oxygenation and perfusion is crucial during the entire resuscitation period, and this often mandates endotracheal intubation, taking care to protect the cervical spine, as injury may not be known.
Once the patient is initially evaluated and causes of secondary brain injury are managed, a head CT should be obtained. If there is evidence of brain swelling, monitoring of ICP is indicated. This is best done with a system that allows drainage of cerebrospinal fluid, such as a ventriculostomy. Avoiding hyperthermia is important, as this may cause secondary brain injury.13 Other management techniques include hyperosmolar therapy with mannitol or hypertonic saline. Sedation is used as needed to maintain a low ICP. Hyperventilation as prophylaxis should generally be avoided. High-dose barbiturate therapy to create a coma has been suggested to be of some benefit. Decompressive craniectomy is now considered an alternative for the surgical management of head-injured children in specific circumstances. It should be considered in head-injured children with cerebral edema and medically uncontrolled intracranial hypertension. It may be of some benefit in children with a potentially recoverable head injury. It is not likely to be useful in children who have suffered an extensive secondary brain injury, or those who have a GCS of 3, with no improvement. Nutritional support, avoidance of steroid use, and treatment of postinjury seizures when indicated are also important aspects of the care of the head-injured patient.
Thoracic Injuries
Thoracic trauma is an important cause of morbidity and mortality in children. It accounts for 4%–25% of pediatric trauma injuries, but these chest injuries are associated with a greater mortality rate when compared with other system injuries. Thoracic trauma can be anticipated in children who present with a low systolic blood pressure, an elevated respiratory rate, abnormalities on thoracic physical examination including abnormal chest auscultation, and femur fractures.14
Pneumothorax and hemothorax are not uncommon injuries in children. A pneumothorax is typically treated with a chest tube appropriately sized for the patient. A hemothorax is also treated with a tube thoracostomy, typically with the largest tube that can be inserted. Intrathoracic blood loss of 15 ml/kg immediately or ongoing losses of 2–3 ml/kg/hour for 3 or more hours suggest the need for thoracic exploration to control bleeding in children. Cardiac injuries are extremely rare, as are tracheobronchial injuries and esophageal injuries. Injuries to the great vessels occur in children with rapid deceleration injuries, and these types of injuries should be considered, with the appropriate mechanism, in any injured child.15
Abdominal Injuries
During the course of routine nonoperative management of abdominal injuries, injuries requiring operative management may be overlooked for quite some time. It has been noted that a delay in diagnosis, although not uncommon, is not associated with increased mortality.16 However, an increase in septic complications has been seen when operative intervention occurred more than 24 hours after injury. Therefore, in-hospital observation with serial examinations should be employed in all children with abdominal examinations that are not perfectly normal. When abdominal injuries occur under suspicious circumstances, the diagnosis of child abuse should be entertained.
The child with a duodenal injury that requires surgery more often presents with abdominal distention, bilious vomiting, pneumoperitoneum, and peritonitis.17 A duodenal hematoma is usually treated nonoperatively with nasogastric decompression and total parenteral nutrition. This management is associated with a high rate of success, but may take as long as 3 weeks for the obstruction to resolve. A late diagnosis of duodenal perforation can occur with this injury and is usually associated with an increase in complications, but not mortality.
The small bowel, both jejunum and ileum, is the most common part of the intestinal tract to be injured in a child. The mechanism of injury to the small bowel is the result of its being trapped between the delivered force and the vertebral column. Adult-sized seatbelts are often used to secure children in a car, and as a result the risk of small bowel injury rises. If a seatbelt bruise is present, the risk of an intra-abdominal injury is much more likely, and therefore a higher index of suspicion should be employed. Children with small bowel injury due to blunt trauma invariably have an abnormal physical examination. Free fluid seen on an ultrasound or CT scan, coupled with a tender abdomen, and no solid organ injury, almost mandates an abdominal exploration for bowel injury. Even if no perforation is identified in surgery, care should be taken to evaluate for mesenteric rents, hematomas, and possibly retroperitoneal injuries. In this same setting, compression injury of the lumbar vertebrae (chance fracture) is also common; and when present, the patient usually requires a longer hospital stay due to pain management.
Injuries to the colon and rectum are not common in children.18 Accidental causes of colon and rectal injuries include motor vehicle collisions involving pelvic fractures and rectal wall penetration by bone shards. Nonaccidental injuries caused by child abuse, typically from blunt instrumentation, are also seen. If the mucosa is injured or the injury is superficial, observation is appropriate. Full thickness injuries of the distal rectum can be managed with primary repair in many cases. Devastating colon injuries above the peritoneal reflection often need a temporary colostomy. Penetrating injuries often can be managed by primary repair, but in the face of complicating features may also need diversion at the time of repair.
The injured spleen in a child will almost always stop bleeding without any intervention. Nonoperative management is the standard of care, and the incidence of any potential operative intervention is very small.19 The rate of operative intervention is likely cut in half when a trained pediatric surgeon is managing the patient. Children who require surgery are those who have received or are likely to receive half their blood volume in transfusions within 24 hours of injury (40 cc/kg). The physiologic response to splenic injury correlates with the grade of splenic injury. Most often children who need operative intervention will need splenectomy. If splenectomy must be performed, post-splenectomy immunization is appropriate. Many children are given penicillin on a daily basis if the splenectomy is performed before age 5 years of age. If immunosuppression is suspected, hepatitis B vaccine should also be administered.
Pediatric pancreatic injuries are uncommon and are most often due to blunt trauma. Bicycle-related injuries should be included in this category. The majority of pancreatic injuries in children may be treated successfully with nonoperative management, including gut rest, intravenous nutrition, and occasionally pancreatic antisecretory medication. Conservative management of children with a pancreatic transection may be more controversial. The beneficial effects of a spleen-sparing distal pancreatectomy, even in the face of a delayed diagnosis, have been noted.20 When the capabilities for pediatric endoscopic retrograde cholangiopancreatography (ERCP) are available, ductal stenting may be of significant benefit. Other surgeons, as well as our group, have been able to employ laparoscopic distal pancreatectomy with splenic salvage for pancreatic transection when stenting could not be accomplished.
1 Kissoon N, Dreyer J, Walia M. Pediatric trauma: differences in pathophysiology, injury patterns and treatment compared with adult trauma. CMAJ. 1990;142:27.
2 Killingsworth JB, Tilford JM, Parker JG, Graham JJ, Dick RM, Aitken ME. National hospitalization impact of pediatric all-terrain vehicle injuries. Pediatrics. 2005;115(3):e316-e321.
3 Edil BH, Tuggle DW, Jones S, Albrecht R, Kuhn A, Mantor PC, Puffinbarger NK. Pediatric major resuscitation—respiratory compromise as a criterion for mandatory surgeon presence. J Pediatr Surg. 2005;40(6):926-928.
4 Chiang VW, Baskin MN. Uses and complications of central venous catheters inserted in a pediatric emergency department. Pediatr Emerg Care. 2000;16(4):230-232.
5 Rogers FB. Technical note: a quick and simple method of obtaining venous access in traumatic exsanguination. J Trauma. 1993;34(1):142-143.
6 National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. the fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl):555-576.
7 Balogh Z, McKinley BA, Cocanour CS, Kozar RA, Valdivia A, Sailors RM, Moore FA. Supranormal trauma resuscitation causes more cases of abdominal compartment syndrome. Arch Surg. 2003;138(6):637-642.
8 Mutabagani KH, Coley BD, Zumberge N, McCarthy DW, Besner GE, Caniano DA, Cooney DR. Preliminary experience with focused abdominal sonography for trauma (FAST) in children: is it useful? J Pediatr Surg. 1999;34(1):48-52.
9 Suthers SE, Albrecht R, Foley D, Mantor PC, Puffinbarger NK, Jones SK, Tuggle DW. Surgeon-directed ultrasound for trauma is a predictor of intra-abdominal injury in children. Am Surg. 2004;70(2):164-167.
10 Ruess L, Sivit CJ, Eichelberger MR, Gotschall CS, Taylor GA. Blunt abdominal trauma in children: impact of CT on operative and nonop-erative management. AJR. 1997;169:1011-1014.
11 Kriel RL, Krach LE, Panser LA. Closed head injury: comparison of children younger and older than 6 years of age. Pediatr Neurol. 1989;5(5):296-300.
12 Selden PD, Bratton SL, Carney NA, et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents following severe pediatric traumatic brain injury. Pediatr Crit Care Med. 2003;4(3 Suppl):S53-S55.
13 Adelson PD, Ragheb J, Kanev P, Brockmeyer D, Beers SR, Brown SD, Cassidy LD, Chang Y, Levin H. Phase II clinical trial of moderate hypothermia after severe traumatic brain injury in children. Neurosurgery. 2005;56(4):740-754.
14 Holmes JF, Sokolove PE, Brant WE, et al. A clinical decision rule for identifying children with thoracic injuries after blunt torso trauma. Ann Emerg Med. 2002;39:492-499.
15 Tiao GM, Griffith PM, Szmuszkovicz JR, et al. Cardiac and great vessel injuries in children after blunt trauma. An institutional review. J Pediatr Surg. 2002;35:1656-1660.
16 Canty TGSr, Canty TGJr, Brown C. Injuries of the gastrointestinal tract from blunt trauma in children: a 12-year experience at a designated pediatric trauma center. J Trauma. 1999;46:234-240.
17 Clendenon JN, Meyers RL, Nance ML, Scaife ER. Management of duodenal injuries in children. J Pediatr Surg. 2004;39(6):964-968.
18 Haut ER, Nance ML, Keller MS, Groner JI, Ford HR, Kuhn A, Tuchfarber B, Garcia V, Schwab CW, Stafford PW. Management of penetrating colon and rectal injuries in the pediatric patient. Dis Colon Rectum. 2004;47(9):1526-1532.
19 Mooney DP, Forbes PW. Variation in the management of pediatric splenic injuries in New England. J Trauma. 2004;56(2):328-333.
20 Meier DE, Coln CD, Hicks BA, Guzzetta PC. Early operation in children with pancreas transection. J Pediatr Surg. 2001;36(2):341-344.