CHAPTER 37 Pediatric Pelvic Osteotomies and Shelf Procedures
Indications
Surgical techniques
Rotational Osteotomies
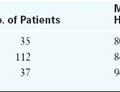
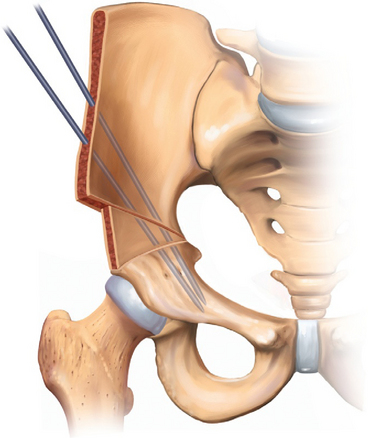
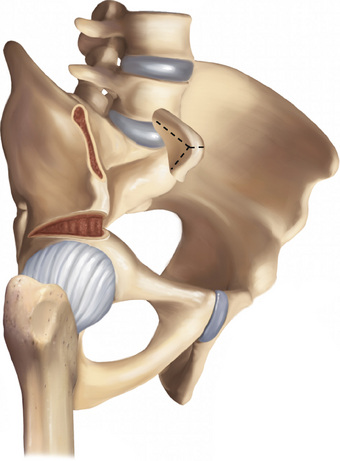
The patient is placed in the supine position with a sandbag under the ipsilateral thorax, and the affected limb is draped free. Adductor contracture is released with a subcutaneous or open tenotomy. Incision and exposure are provided via a Smith-Peterson approach to the hip. A so-called bikini incision starts 2 cm distal to the center of the iliac crest, extends 1 cm distal to the anterosuperior iliac spine, and ends below the middle of the inguinal ligament. The interval between the tensor fascia latae and the sartorius is developed to expose the rectus femoris and the anteroinferior iliac spine. The iliac apophysis is incised down to bone along the iliac crest from the posterior end of the skin incision to the anteroinferior iliac spine. The lateral portion of the apophysis and the periosteum of the outer table are carefully stripped in a continuous sheet to the lateral edge of the acetabulum and posteriorly to the greater sciatic notch; this space is then packed. Adhesions of the joint capsule to the lateral aspect of the ilium can be freed with a periosteal elevator. The medial half of the apophysis and the periosteum of the inner wall are carefully stripped in a continuous sheet to expose the sciatic notch. Care is taken to remain subperiosteal to avoid injury to the sciatic nerve and the superior gluteal artery. The tendinous portion of the iliopsoas is exposed on its deep surface at the level of the pelvic brim and rolled over to visualize the musculotendinous junction. A scissors is passed between the tendon and the musculotendinous junction, and the tendon is cut sharply with a scalpel. The tip of a curved forceps is passed subperiosteally from the medial side and through the sciatic notch to grasp the end of the Gigli saw. The index finger of the opposite hand is used to guide the forceps. The skin and the soft tissues are retracted widely. The osteotomy extends in a straight line from the sciatic notch to the anteroinferior iliac spine, with care taken to remain at right angles to the vertical axis of the ilium. The hands are kept far apart, and continuous tension is placed on each end of the saw to keep it from binding (Figure 37-1). A triangular-shaped bone graft is then taken from the iliac crest with large bone cutters. (A saw may be used in older children.) The base of the graft extends from the anterosuperior iliac spine to the anteroinferior iliac spine. A towel clip is placed on each fragment. The proximal fragment should only be steadied. The towel clip on the distal fragment should be placed well posterior to avoid fracture. The distal fragment is then rotated downward and forward in line with the ilium, which opens the osteotomy anterolaterally. Avoid the posterior or medial displacement of the distal fragment. If the hip capsule has not been opened, the leg can be used to attain the desired correction by placing it in a figure-four position. Downward pressure on the knee as the heel is moved toward the child’s chin produces the desired rotation. The wedge-shaped bone graft is then inserted into the osteotomy site, and the traction is released from the distal fragment. The posterior aspect of the osteotomy should remain closed. Two heavy, threaded K-wires are inserted across the osteotomy site, through the graft, and into the distal segment that lies medial and posterior to the acetabulum (Figure 37-2). Care is taken to avoid penetrating the hip joint. The hip is carefully moved so that crepitus can be heard and felt for; this may indicate that a pin has penetrated the joint. The two halves of the iliac apophysis are sutured together. The K-wires are cut so that their ends lie in subcutaneous fat. A drain is usually not necessary if only an innominate osteotomy has been performed. The wound is then closed. A 1½ hip spica cast is applied with the hip in slight abduction, flexion, and internal rotation and with the knee in flexion. In older, reliable children, three-point partial weight bearing with crutches may be permitted with no immobilization.
Osteotomies in which all three pelvic bones (e.g., Steel, Tönnis, Carlioz) are cut offer greater rotational advantages. The Ganz periacetabular osteotomy may be performed for patients with a closed triradiate cartilage. This procedure is discussed in detail in Chapter 26, and it will not be discussed here. Variations of the triple osteotomy exist for patients with open triradiate cartilage.
Volume-Reducing Osteotomies
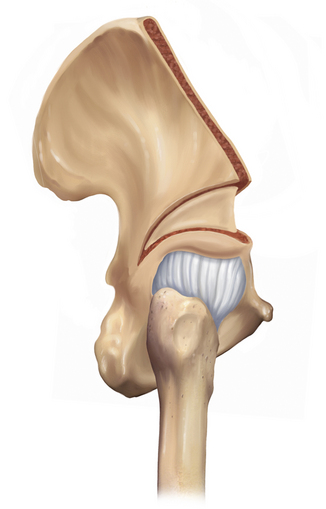
The patient is positioned supine, with a bump placed under the involved hip. Exposure is via a Smith-Peterson approach to the hip. Just as with the Salter osteotomy, the iliac apophysis is split, and both the inner and outer tables of the ilium are exposed subperiosteally. Exposure is carried out to the sciatic notch, and the rectus insertion is left alone. Although it was not recommended by Pemberton in his original article, the division of the psoas tendon (as in the Salter osteotomy) may facilitate correction. Two flat-blade retractors are inserted into the sciatic notch on either side of the ilium. The osteotomy is performed with a narrow curved osteotome through the outer table, starting 1 cm above the anteroinferior iliac spine and extending posteriorly, keeping 1 cm to 1.5 cm from the attachment of the hip capsule. Because the osteotomy is carried posteriorly and then inferiorly through the outer table, it will disappear into the soft-tissue attachments behind the capsule. Visualization can be facilitated by the rotation of the retractor in the sciatic notch. Care must be taken to avoid cutting into the sciatic notch. Direct the osteotomy to the ilioischial limb of the triradiate cartilage. With the use of the same osteotome, a corresponding cut is made on the inner table. As with the outer table, avoid cutting into the sciatic notch. The plane of the osteotomy may be adjusted on the basis of the type of coverage that is necessary. A more transverse cut will provide more anterior coverage, whereas a laterally inclined osteotomy will provide more lateral coverage. After both cortices of the ilium have been cut, a wide curved osteotomy is used to connect the two cuts. As the osteotome proceeds posteriorly, it will become apparent that it cannot make the sharp turn inferiorly into the posterior column. A special Pemberton right-angled curved osteotome is used to complete this cut into the triradiate cartilage (Figure 37-3). A small lamina spreader can hold the osteotomy apart and facilitate this cut. The acetabulum can now be directed into the desired position. A groove is cut into each surface of the osteotomy with a narrow gouge or curette. A triangular wedge of bone is removed from the anterior iliac crest and placed in the osteotomy site (Figure 37-4). Because the graft will be recessed in the osteotomy site, the graft should be larger than the gap created by the osteotomy. This osteotomy is quite secure, and it does not require additional fixation. The iliac apophysis is reapproximated, and the wound is closed. The patient is placed in a 1½ hip spica cast.
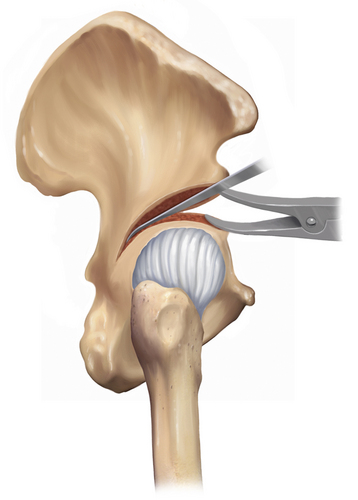
The patient is positioned supine, with a bump placed under the involved hip. Exposure is via a Smith-Peterson approach to the hip. Unlike the previously described procedures, only the outer table of the ilium is exposed subperiosteally. Exposure is carried out to the sciatic notch. The iliac apophysis is not split but instead elevated as a unit. A 1.5-cm-wide straight osteotome is used to make an osteotomy 0.5 cm to 1 cm above the edge of the acetabulum on a line drawn from the anteroinferior iliac spine to the sciatic notch. A preliminary notch is made at the extreme ends of the intended osteotomy, at the sciatic notch and the anteroinferior iliac spine, to prevent inadvertent fracture. The lateral cortex is cut, but the medial wall is kept intact; this will allow the fragment to bend freely. A 2-cm-wide curved osteotome is used to deepen the osteotomy in a medial and caudal direction behind the acetabulum to the horizontal limb of the triradiate cartilage (Figure 37-5). The osteotome should be directed halfway between the medial wall of the ilium and the medial wall of the acetabulum; this can be monitored with image intensification. Bicortical bone graft is obtained from the anterosuperior iliac spine and shaped into three or four small triangles with a base of 1 cm. The osteotomy site is opened with an osteotome or a lamina spreader. The grafts are placed into the osteotomy site, with the largest graft placed in the area in which maximum coverage is needed (Figure 37-6). This osteotomy is stable and does not require further fixation. The wound is closed. A 1½ hip spica cast is placed on the patient, with the hip in 45 degrees of flexion and 30 degrees of abduction.
Salvage Procedures
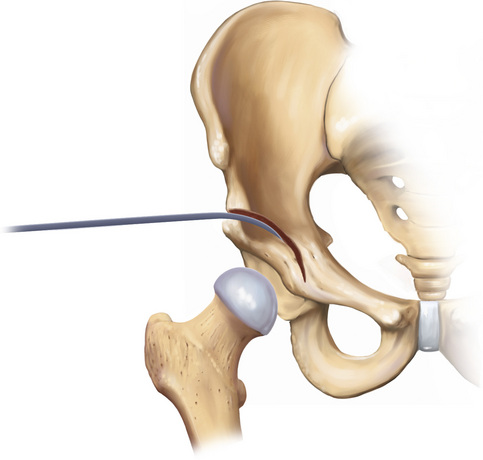
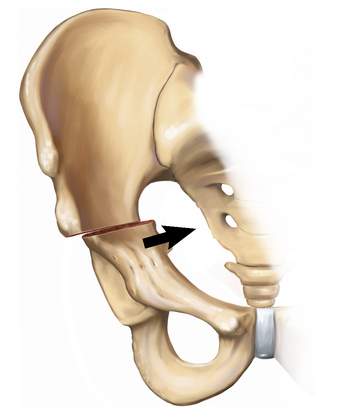
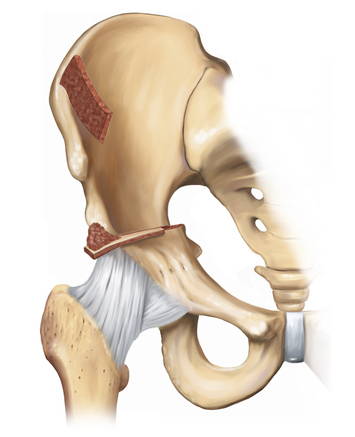
Position the patient supine, with a bump placed under the involved hip. Exposure is via a Smith-Peterson approach. As with the Salter osteotomy, the inner and outer tables of the ilium are exposed. The superior aspect of the hip capsule needs to be well exposed anteroposteriorly to facilitate the correct placement of the osteotomy. A guidewire should be drilled lateral to medial, with a 10-degree to 15-degree cephalad incline just above the acetabular roof. The osteotomy should be between the capsular insertion and the reflected rectus head, it should head in a curvilinear fashion along the capsular insertion, and it should end anteriorly under the anteroinferior iliac spine and posteriorly in the sciatic notch (Figure 37-7). Pass a Gigli saw through the sciatic notch (i.e., like the initiation of the Salter osteotomy) to score the anterior cortex of the sciatic notch to ensure that the osteotomy fractures through that point in the notch. The lateral cortex is cut first, and this is followed by the medial cortex. Ensure that there are no posterior tethers. The distal fragment is displaced medially by abducting the leg. Further displacement can be achieved by placing direct pressure over the greater trochanter. After the desired displacement is achieved, fixation is obtained with two or three screws or large threaded Steinmann pins. Coverage can be augmented anteriorly by obtaining corticocancellous bone from the inner table of the ilium and placing it in the osteotomy site before fixation (Figure 37-8). Additional cancellous bone graft is added and held in place by the periosteum when the wound is closed.
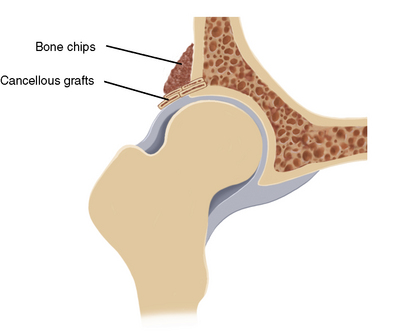
The patient is positioned supine, with a bump placed under the involved hip. Exposure is via a Smith-Peterson approach. Only the outer table of the ilium is exposed subperiosteally. The reflected head of the rectus femoris is sectioned at the junction of the conjoint tendon; it is reflected to expose the entire hip capsule, and it will be used to secure the bone graft. The location of the slot should be at the edge of the acetabulum; the correct location can be verified with image intensification. When the correct location is identified, a  -inch drill or a burr is used to make a series of 1-cm-deep holes that incline 20 degrees cephalad at the edge of the acetabulum (Figure 37-9). A narrow rongeur or burr is used to connect the holes and to produce a slot; the floor of the slot should be the subchondral bone of the acetabulum. Corticocancellous and cancellous strips of bone graft are obtained from the outer table of the ilium. The cancellous grafts are cut into 1-cm-wide strips that are long enough to provide adequate lateral femoral head coverage. They are placed in the slot so that they extend out over the capsule. A second layer of cancellous strips is placed perpendicular to the first layer (Figure 37-10). Extending the graft too anterior or lateral may result in impingement, so this should be avoided. The reflected head of the rectus is sutured back to the conjoint tendon, which holds the grafts in place. The remaining bone is cut into small pieces and placed over the graft. The wound is closed, and the patient’s hip is placed in a 1½ hip spica cast in 20 degrees of flexion and 15 degrees of abduction.
-inch drill or a burr is used to make a series of 1-cm-deep holes that incline 20 degrees cephalad at the edge of the acetabulum (Figure 37-9). A narrow rongeur or burr is used to connect the holes and to produce a slot; the floor of the slot should be the subchondral bone of the acetabulum. Corticocancellous and cancellous strips of bone graft are obtained from the outer table of the ilium. The cancellous grafts are cut into 1-cm-wide strips that are long enough to provide adequate lateral femoral head coverage. They are placed in the slot so that they extend out over the capsule. A second layer of cancellous strips is placed perpendicular to the first layer (Figure 37-10). Extending the graft too anterior or lateral may result in impingement, so this should be avoided. The reflected head of the rectus is sutured back to the conjoint tendon, which holds the grafts in place. The remaining bone is cut into small pieces and placed over the graft. The wound is closed, and the patient’s hip is placed in a 1½ hip spica cast in 20 degrees of flexion and 15 degrees of abduction.
Technical Pearls
Salter Osteotomy
Pemberton Osteotomy
San Diego Acetabuloplasty
Chiari Osteotomy
Annotated references and suggested readings
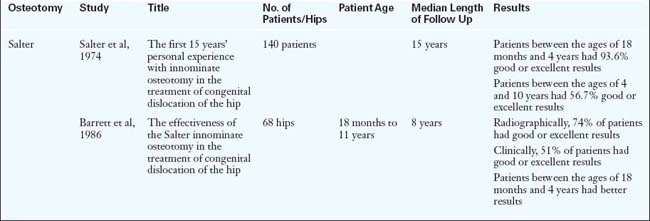
Barrett W.P., Staheli L.T., Chew D.E. The effectiveness of the Salter innominate osteotomy in the treatment of congenital dislocation of the hip. J Bone Joint Surg. 1986;68:79-87.
Bohm P., Brzuske A. Salter innominate osteotomy for the treatment of developmental dysplasia of the hip in children: results of seventy-three consecutive osteotomies after twenty-six to thirty-five years of follow-up. J Bone Joint Surg. 2002;84-A:178-186.
Calvert P.T., August A.C., Albert J.S., et al. The Chiari pelvic osteotomy. A review of the long-term results. J Bone Joint Surg Br. 1987;69:551-555.
Chiari K. Medial displacement osteotomy of the pelvis. Clin Orthop. 1974;98:55-71.
Faciszewski T., Kiefer G.N., Coleman S.S. Pemberton osteotomy for residual acetabular dysplasia in children who have congenital dislocation of the hip. J Bone Joint Surg. 1993;75:643-649.
Gillingham B.L., Sanchez A.A., Wenger D.R. Pelvic osteotomies for the treatment of hip dysplasia in children and young adults. J Am Acad Orthop Surg. 1999;7:325-337.
Hadley N.A. The effects of contact pressure elevations and aseptic necrosis on the long-term outcome of congenital hip dislocation. J Orthop Res. 1990;8:504-513.
Harris N.G. Acetabular growth potential in congenital dislocation of the hip and some factors upon which it may depend. Clin Orthop. 1976;119:99-106.
Ito H., Ooura H., Kobayashi M., et al. Middle-term results of Salter innominate osteotomy. Clin Orthop. 2001;387:156-164.
Love B.R., Stevens P.M., Williams P.F. A long-term review of shelf arthroplasty. J Bone Joint Surg Br. 1980;62:321-325.
McNerney N.P., Mubarak S.J., Wenger D.R. One-stage correction of the dysplastic hip in cerebral palsy with the San Diego acetabuloplasty: results and complications in 104 hips. J Pediatr Orthop. 2000;20:93-103.
Morrissy R.T., Weinstein S.L. Atlas of pediatric orthopaedic surgery, 4th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.
Mubarak S.J., Valencia F.G., Wenger D.R. One-stage correction of the spastic dislocated hip. Use of pericapsular acetabuloplasty to improve coverage. J Bone Joint Surg. 1992;74:1347-1357.
Nishimatsu H., Iida H., Kawanabe K. et al. The modified Spitzy shelf operation for patients with dysplasia of the hip. A 24-year follow-up study. J Bone Joint Surg Br. 2002;84:647-652.
Pemberton P.A. Pericapsular osteotomy of the ilium for treatment of congenital subluxation and dislocation of the hip. J Bone Joint Surg. 1965;47:65-86.
Ponsetti I.V. Growth and development of the acetabulum in the normal child. J Bone Joint Surg. 1978;60:575-585.
Rozkydal Z., Kovanda M. Chiari pelvic osteotomy in the management of developmental hip dysplasia: a long term follow-up. Bratisl Lek Listy. 2003;104:7-13.
Salter R.B. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg Br. 1961;43B:518-539.
Salter R.B., Dubos J.P. The first fifteen year’s personal experience with innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. Clin Orthop. 1974;98:72-103.
Staheli L.T. Chew DE. Slotted acetabular augmentation in childhood and adolescence. J Pediatr Orthop. 1992;12:569-580.
Summers B.N., Turner A., Wynn-Jones C.H. The shelf operation in the management of late presentation of congenital hip dysplasia. J Bone Joint Surg Br. 1988;70B:63-68.
Thomas S.R., Wedge J.H., Salter R.B. Outcome at forty-five years after open reduction and innominate osteotomy for late- presenting developmental dislocation of the hip. J Bone Joint Surg. 2007;89:2341-2350.
Wada A., Fujii T., Takamura K., et al. Pemberton osteotomy for developmental dysplasia of the hip in older children. J Pediatr Orthop. 2003;23:508-513.
Weinstein S.L. Natural history of congenital hip dislocation (CDH) and hip dysplasia. Clin Orthop. 1987;225:62-76.
Weinstein S.L., Mubarak S.J., Wenger D.R. Developmental hip dysplasia and dislocation: part I. Instr Course Lect. 2004;53:523-530.
Windhager R., Pongracz N., Schonecker W., et al. Chiari osteotomy for congenital dislocation and subluxation of the hip: results after 20 to 34 years follow-up. J Bone Joint Surg Br. 1991;73B:890-895.

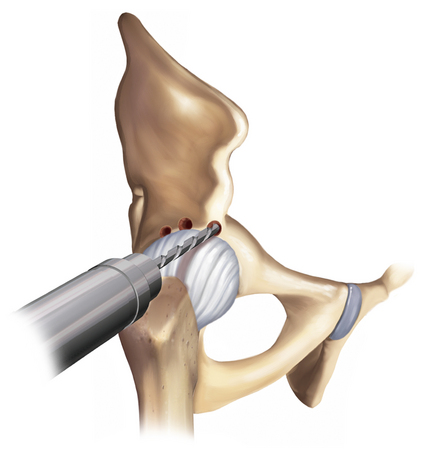
 -inch drill bit is used to make a series of holes at the edge of the acetabulum. These holes should be drilled to a depth of about 1 cm, and they should incline about 20 degrees, as illustrated. They should extend far enough anteriorly and posteriorly to provide the necessary coverage.
-inch drill bit is used to make a series of holes at the edge of the acetabulum. These holes should be drilled to a depth of about 1 cm, and they should incline about 20 degrees, as illustrated. They should extend far enough anteriorly and posteriorly to provide the necessary coverage.