Chapter 62 Pediatric Emergencies and Resuscitation
Injuries are the leading cause of death in American children and young adults and are responsible for more childhood deaths than all other causes combined (Chapter 5.1). Children are particularly vulnerable to injury for a number of reasons, including their small size, relative physical uncoordination, and limited ability to predict or understand danger. In addition, the immaturity of their developing bones, ligaments, and muscles; their thin body walls; and their relatively large heads, compared with total body surface area, make young children susceptible to serious or fatal injury from falls and collisions.
Serious injuries can become fatal when appropriate medical care is delayed.
Approach to the Emergency Evaluation of a Child
General Assessment
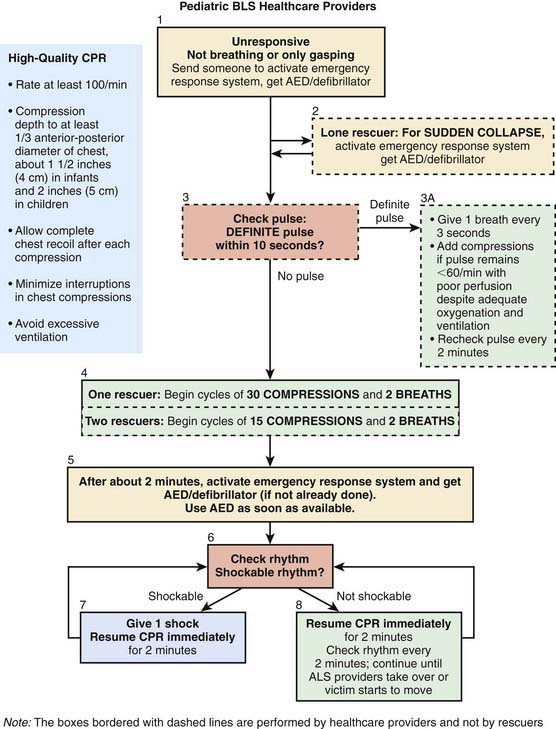
Once the caregiver and patient’s safety has been ensured, the caregiver performs a rapid visual survey of the child, assessing the child’s general appearance and cardiopulmonary function. This action should be very quick (only a few seconds) and should include assessment of (1) general appearance (determining color, tone, alertness, and responsiveness); (2) adequacy of breathing (distinguishing between normal, comfortable respirations and respiratory distress or apnea); and (3) adequacy of circulation (identifying cyanosis, pallor, or mottling). A child found unresponsive from an unwitnessed collapse should be approached with a gentle touch and the verbal question, “Are you OK?” If there is no response, the caregiver should immediately shout for help and send someone to both activate the emergency response system (EMS) and locate an automated external defibrillator (AED) (Fig. 62-1). The provider should then determine whether the child is breathing and, if not, provide 2 rescue breaths as described later under Recognition and Treatment of Respiratory Distress and Failure. If the child is adequately breathing, then the circulation is quickly assessed. Any child with a heart rate below 60 beats/min or without a pulse requires immediate CPR, as described under Cardiac Arrest. If the caregiver witnesses the sudden collapse of a child, the caregiver should have a higher suspicion for a sudden cardiac event. In this case, rapid deployment of an AED is of paramount importance. The provider should very briefly delay care of the child to activate EMS and locate the nearest AED.
Primary Assessment
The exam and vital sign data can be interpreted only if the caregiver has a thorough understanding of normal values. In pediatrics, normal respiratory rate, heart rate, and blood pressure have age-specific norms (Table 62-1). These ranges can be difficult to remember, especially if used infrequently. However, several standard principals apply: (1) no child’s respiratory rate should be >60 breaths/min for a sustained period; (2) normal heart rate is roughly 2-3 times normal respiratory rate for age; and (3) a simple guide for pediatric blood pressure (BP) is that the lower limit of systolic BP should be <60 mm Hg for neonates; <70 mm Hg for 1 mo–1 yr olds; <70 mm Hg + (2 × age) for 1-10 yr olds; and <90 mm Hg for any child older than 10 yr.
Airway and Breathing
The most common precipitating event for cardiac instability in infants and children is respiratory insufficiency. Therefore, rapid assessment of respiratory failure and immediate restoration of adequate ventilation and oxygenation remain the first priority in the resuscitation of a child. Using a systematic approach, the caregiver should first assess whether the child’s airway is patent and maintainable. A healthy, patent airway is open and unobstructed, allowing normal respiration without noise or effort. A maintainable airway is one that is either already patent or can be made patent with a simple maneuver. To assess airway patency, the provider should look for breathing movements in the child’s chest and abdomen, listen for breath sounds, and feel the movement of air at the child’s mouth and nose. Abnormal breathing sounds (i.e., snoring or stridor), increased work of breathing, and apnea are all findings potentially consistent with airway obstruction. If there is evidence of airway obstruction, then maneuvers to relieve the obstruction should be instituted before the caregiver proceeds to evaluate the child’s breathing (see under Recognition and Treatment of Respiratory Distress and Failure, Initial Management).
Disability
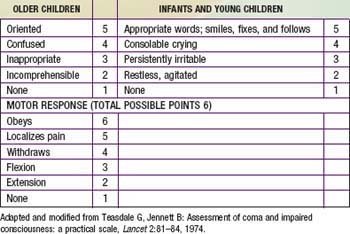
In the setting of a pediatric emergency, disability refers to a child’s neurologic function in terms of the level of consciousness and cortical function. Standard evaluation of a child’s neurologic condition can be done quickly with an assessment of pupillary response to light (if one is available) and use of either of the standard scores used in pediatrics: the Alert, Verbal, Pain, Unresponsive (AVPU) Pediatric Response Scale and the Glasgow Coma Scale (GCS) (Tables 62-2 and 62-3). The causes of decreased level of consciousness in children are numerous and include conditions as diverse as respiratory failure with hypoxia or hypercarbia, hypoglycemia, poisonings or drug overdose, trauma, seizures, infection, and shock. Most commonly, an ill or injured child has an altered level of consciousness because of respiratory compromise, circulatory compromise, or both. Any child with a depressed level of consciousness should be immediately assessed for abnormalities in cardiorespiratory status.
| A | The child is awake, alert, and interactive with parents and care providers |
| V | The child responds only if the care provider or parents call the child’s name or speak loudly |
| P | The child responds only to painful stimuli, such as pinching the nail bed of a toe or finger |
| U | The child is unresponsive to all stimuli |
From Ralston M, Hazinski MF, Zaritsky AL, et al, editors: Pediatric advanced life support course guide and PALS provider manual: provider manual, Dallas, 2007, American Heart Association.
The Alert, Verbal, Pain, Unresponsive Pediatric Response Scale
The AVPU scoring system is used to determine both a child’s level of consciousness and cerebral cortex function. Unlike the GCS (see later), the AVPU scale is not developmentally dependent—a child does not have to understand spoken language or follow commands, merely respond to a stimulus. The child is scored according to the amount of stimulus required to get a response, from alert (no stimulus, the child is already awake and interactive) to unresponsive (child does not respond to any stimulus) (see Table 62-2).
The Glasgow Coma Scale
Although the GCS has not been validated as a prognostic scoring system for infants and young children as it has been in adults, it is commonly used in the assessment of pediatric patients with an altered level of consciousness. The GCS is the most widely used method of evaluating a child’s neurologic function and has 3 components. Individual scores for eye opening, verbal response, and motor response are added together, with a maximum of 15 points (see Table 62-3). Patients with a GCS score ≤8 require aggressive management, including stabilization of the airway and breathing with endotracheal intubation and mechanical ventilation, respectively, and, if indicated, placement of an intracranial pressure monitoring device.
Tertiary Assessment
The tertiary assessment occurs in a hospital setting, where ancillary laboratory and radiographic assessments contribute to a thorough understanding of the child’s condition. A basic blood chemistry profile, complete blood count, liver function tests, coagulation studies, and arterial blood gas analyses give fairly broad (but somewhat nonspecific) estimates of renal function, acid-base balance, cardiorespiratory function, and presence or absence of shock. Chest radiographs can be useful to evaluate both the heart and lungs, although more detailed estimates of heart function and cardiac output can be made with echocardiography. Arterial and central venous catheters can be placed to monitor arterial and central venous pressure (see under Vascular Access).
Recognition and Treatment of Respiratory Distress and Failure
Airway Obstruction
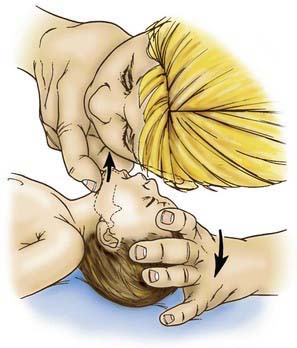
Airway obstruction is treated with a sequential approach, starting with the head-tilt/chin-lift maneuver to open and support the airway, followed by inspection for a foreign body, and finger-sweep clearance or suctioning if one is visualized (Fig. 62-2). Blind suctioning or finger sweeps of the mouth are not recommended. A nasopharyngeal airway (NPA) or oropharyngeal airway (OPA) can be inserted for airway support, if indicated. A conscious child suspected of having a partial foreign body obstruction should be permitted to cough spontaneously until coughing is no longer effective, respiratory distress and stridor increase, or the child becomes unconscious.
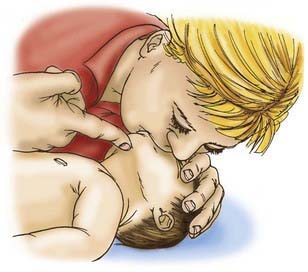
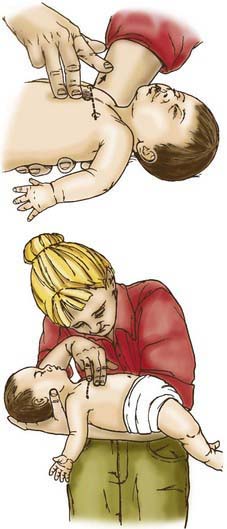
If the child becomes unconscious, the child should be gently placed on the ground, supine. The provider should then open the airway with the head-tilt/chin-lift maneuver and attempt mouth-to-mouth ventilation (Figs. 62-3 and 62-4). If ventilation is unsuccessful, the airway is repositioned, and ventilation attempted again. If there is still no chest rise, attempts to remove a foreign body are indicated. In an infant <1 yr old, a combination of 5 back blows and 5 chest thrusts is administered (Fig. 62-5). After each cycle of back blows and chest thrusts, the child’s mouth should be visually inspected for the presence of the foreign body. If identified within finger’s reach, it should be removed with a gentle finger sweep. If no foreign body is visualized, ventilation is again attempted. If this is unsuccessful, the head is repositioned, and ventilation attempted again. If there is no chest rise, the series of back blows and chest thrusts is repeated.

Figure 62-5 Back blows (top) and chest thrusts (bottom) to relieve foreign body airway obstruction in the infant.
(From Guidelines for cardiopulmonary resuscitation and emergency cardiac care. Emergency Cardiac Care Committee and Subcommittees, American Heart Association. Part V. Pediatric basic life support, JAMA 268:2251–2261, 1992.)
For a conscious child >1 yr old, providers should give a series of 5 abdominal thrusts (Heimlich maneuver) with the child standing or sitting (Fig. 62-6); this should occur with the child lying down if unconscious (Fig. 62-7). After the abdominal thrusts, the airway is examined for a foreign body, which should be removed if visualized. If no foreign body is seen, the head is repositioned, and ventilation attempted. If it is unsuccessful, the head is repositioned and ventilation is attempted again. If these efforts are unsuccessful, the Heimlich sequence is repeated.

Figure 62-6 Abdominal thrusts with the victim standing or sitting (conscious).
(From Guidelines for cardiopulmonary resuscitation and emergency cardiac care. Emergency Cardiac Care Committee and Subcommittees, American Heart Association. Part V. Pediatric basic life support, JAMA 268:2251–2261, 1992.)
Airway Narrowing
Airway support for these processes is dictated by both the underlying condition and the clinical severity of the problem. In cases of mild upper airway obstruction, the child has minimally elevated work of breathing (evidenced by tachypnea and few to mild retractions). Stridor, if present at all, should be audible with only coughing or activity. Children with these findings can be supported with nebulized cool mist and supplemental oxygen as needed. In cases with moderate obstruction, in which the child has a higher work of breathing and more pronounced stridor, nebulized racemic epinephrine and oral or intravenous (IV) dexamethasone can be added. Children with severe upper airway obstruction have marked retractions, prominent stridor, and decreased air entry on auscultation of the lung fields. Most children with significant airway obstruction are also hypoxic, and many appear dyspneic and agitated. A child in severe distress needs to be closely observed, as the signs of impending respiratory failure may be initially confused with improvement. Stridor becomes quieter and retractions less prominent when a child’s respiratory effort begins to diminish. The child in respiratory failure can be distinguished from one who is improving by evidence of poor air movement on auscultation and lethargy or decreased level of consciousness from hypercarbia, hypoxia, or both. When anaphylaxis is suspected as the cause for upper airway edema, providers should administer an intramuscular (IM) or IV dose of epinephrine as needed (Chapter 143). No matter the cause, any child in impending respiratory failure should be prepared for endotracheal intubation and respiratory support.
In cases of lower airway obstruction, therapies are targeted to both relieving the obstruction and reducing the child’s work of breathing. Inhaled bronchodilators, such as albuterol, augmented by oral or IV corticosteroids, remain the mainstay of therapy in settings of mild to moderate acute distress due to lower airway obstruction. Children with more significant obstruction appear dyspneic, with tachypnea, retractions, and easily audible wheezing. In these cases, the addition of an anticholinergic agent, such as nebulized ipratropium bromide, or a smooth muscle relaxant, such as magnesium sulfate, may provide further relief, although the evidence for these measures remains controversial (Chapter 138). Supplemental oxygen and IV fluid hydration can also be useful adjuncts. As in cases of upper airway obstruction, impending respiratory failure in children with lower airway obstruction can be insidious. When diagnosed early in a school-aged child who is cooperative, respiratory failure can be averted through judicious use of noninvasive support, with continuous positive airway pressure (CPAP), bilevel positive airway pressure (BiPAP), or heliox (combined helium-oxygen therapy). Endotracheal intubation should be performed only by skilled providers, preferably in a hospital setting, because there is a high risk of respiratory and circulatory compromise in patients with lower airway obstruction during the procedure.
Advanced Airway Management Techniques
Bag-Valve-Mask Positive Pressure Ventilation
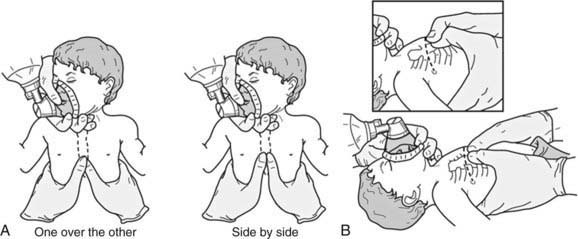
Rescue breathing with a bag-valve-mask apparatus can be as effective as endotracheal intubation and safer when the provider is inexperienced with intubation. Bag-valve-mask ventilation itself requires training to ensure that the provider is competent to select the correct mask size, open the child’s airway, form a tight seal between the mask and the child’s face, deliver effective ventilation, and assess the effectiveness of the ventilation. An appropriately sized mask is one that fits over the child’s mouth and nose but does not extend below the chin or over the eyes (Fig. 62-8). An adequate seal is best achieved via a combination “C–E” grip on the mask, in which the thumb and index finger form the letter “C” on top of the mask, pressing the mask downward onto the child’s face, and the remaining three fingers form an “E” grip under the child’s mandible, holding the jaw forward and extending the head up toward the mask. Using this method, the care provider can secure the mask to the child’s face with one hand and use the other hand to compress the ventilation bag (Fig. 62-9).
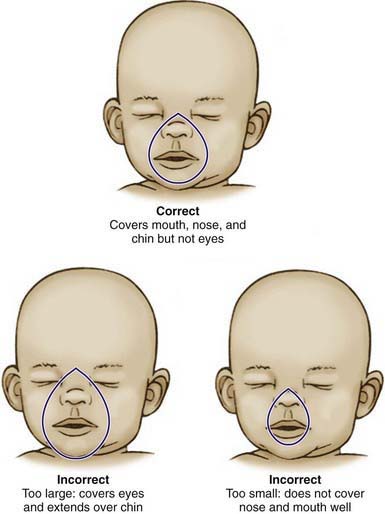
Figure 62-8 Appropriate sizing technique for pediatric bag-valve-mask apparatus.
(From American Academy of Pediatrics and the American Heart Association; Short J, editor: Textbook of neonatal resuscitation, ed 5, Elk Grove, IL, American Academy of Pediatrics, 2006, pp 3–16.)
The provider may have to move the head and neck through a range of positions to find the one that best maintains airway patency and allows maximal ventilation. In infants and young children, optimal ventilation is often provided when the child’s head is in the neutral “sniffing” position without hyperextension of the head (Fig. 62-10). Poor chest rise and persistently low oxygen saturation values indicate inadequate ventilation. In this setting, the care provider should recheck the mask’s seal on the child’s face, reposition the child’s head, and consider suctioning the airway if indicated. If these maneuvers do not restore ventilation, then the provider should consider endotracheal intubation.
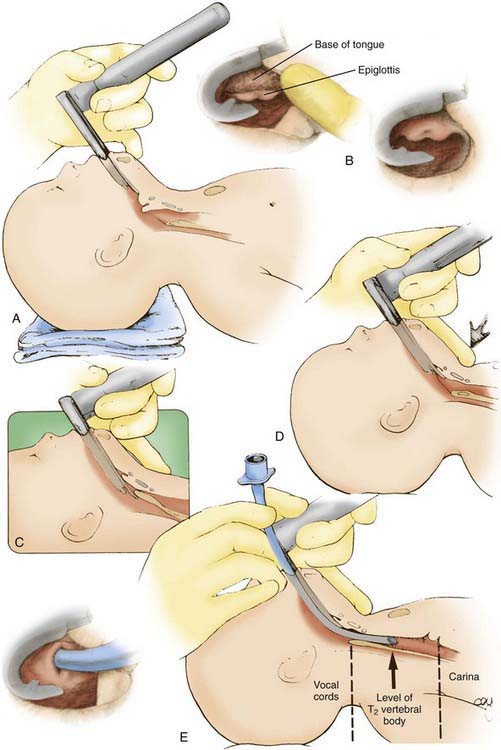
Endotracheal Intubation
Because many intubations in critically ill children are emergency procedures, caregivers should be prepared for rapid sequence intubation (RSI) (Fig. 62-11; Table 62-4). The goals of RSI are to induce anesthesia and paralysis and to complete intubation quickly. This approach minimizes elevations of intracranial pressure and blood pressure that may accompany intubation in awake or lightly sedated patients. Because the stomach generally cannot be emptied before RSI, the Sellick maneuver (downward pressure on the cricoid cartilage to compress the esophagus against the vertebral column) should be used to prevent aspiration of gastric contents.
| STEP | PROCEDURE | COMMENT/EXPLANATION |
|---|---|---|
| 1 | Obtain a brief history and perform an assessment | Rule out drug allergies; examine the airway anatomy (e.g., micrognathia, cleft palate) |
| 2 | Assemble equipment, medications, etc. | See lists below |
| 3 | Preoxygenate the patient | With bag/mask, nasal cannula, hood or blow-by |
| 4 | Premedicate the patient with lidocaine, atropine | Lidocaine minimizes the ICP rise with intubation and can be applied topically to the airway mucosa for local anesthesia |
| Atropine helps blunt the bradycardia associated with upper airway manipulation and reduces airway secretions | ||
| 5 | Induce sedation and analgesia | Sedatives: |
| Thiopental (2-5 mg/kg): Very rapid onset; can cause hypotension. | ||
| Diazepam (0.1 mg/kg): Onset 2-5 min; elimination in 30-60 min or more. | ||
| Ketamine (2 mg/kg): Onset 1-2 min; elimination in 30-40 min. May cause hallucinations if used alone; causes higher ICP, mucous secretions, increased vital signs, and bronchodilation. | ||
| Analgesics: | ||
| Fentanyl (3-10 µg/kg, may repeat 3-4×): Rapid administration risks “tight chest” response, with no effective ventilation. Effects wear off in 20-30 min. | ||
| Morphine (0.05-0.1 mg/kg dose): May last 30-60 min; may lead to hypotension in hypovolemic patients. | ||
| 6 | Pretreat with nondepolarizing paralytic agent | Small dose of a nondepolarizing paralytic agent (see below), with intent of diminishing the depolarizing effect of succinylcholine, which is administered next |
| 7 | Administer muscle relaxants | Succinylcholine dose is 1-2 mg/kg; causes initial contraction of muscles, then relaxation. This depolarization can, however, raise ICP and blood pressure. Onset of paralysis in 30-40 sec; duration is 5-10 min. |
| Increased use of pretreatment with a nondepolarizing muscle relaxant, especially rocuronium (1 mg/kg), which has a very rapid onset and short duration. Other nondepolarizing agents include vecuronium and pancuronium, both dosed at 0.1 mg/kg. | ||
| 8 | Perform a Sellick maneuver | Pressure on the cricoid cartilage, to occlude the esophagus and prevent regurgitation or aspiration |
| 9 | Perform endotracheal intubation | ET: Select the proper size for the age and weight of the child |
| Laryngoscope blades: A variety of Miller and the Macintosh blades | ||
| Patient supine; the neck is extended moderately to the “sniffing” position | ||
| 10 | Secure the tube and verify the position with a roentgenogram | ET secured with tape to the cheeks and upper lip or to an adhesive patch applied to the skin near the mouth. |
| 11 | Begin mechanical ventilation | Verify tube placement before ventilating with positive pressure; if an ET tube is in one bronchus, barotraumas may occur |
ET, endotracheal tube; ICP, intracranial pressure.
Recognition and Management of Shock
In simple terms, shock occurs when oxygen and nutrient delivery to the tissues is inadequate to meet metabolic demands (Chapter 64). The definition of shock does not include hypotension, and it is important for care providers to understand that shock does not begin when blood pressure drops but merely worsens and becomes more difficult to treat once blood pressure is abnormal.
Recognition of Bradyarrhythmias and Tachyarrhythmias
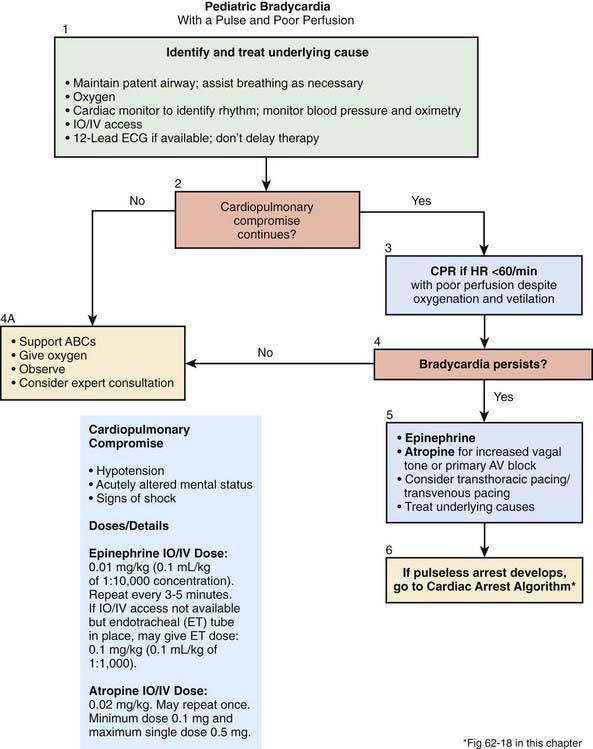
Bradyarrhythmias
By definition, a child is bradycardic when the heart rate is slower than the normal range for age (see Table 62-1). Sinus bradycardia can be a harmless incidental finding in an otherwise healthy person and is not commonly associated with cardiac compromise. A relative bradycardia occurs when the heart rate is too slow for a child’s activity level or metabolic needs. A clinically significant bradycardia occurs when the heart rate is slow and there are signs of systemic hypoperfusion (i.e., pallor, altered mental status, hypotension, acidosis). Symptomatic bradycardia occurs most often in the setting of hypoxia but can also be caused by hypoglycemia, hypocalcemia, other electrolyte abnormalities, and intracranial hypertension. Bradyarrhythmias are often the most common pre-arrest rhythms in young children.
Initial management of symptomatic bradycardia includes support or opening of the airway and confirming or establishing adequate oxygenation and ventilation (Fig. 62-12). After the child’s breathing has been secured, the child should be reassessed for continued bradycardia and poor perfusion—if cardiac compromise was solely the result of respiratory insufficiency, support of the child’s airway and breathing may have been sufficient to restore normal hemodynamics. If respiratory support does not correct the perfusion abnormalities, then further care is based on the quality of perfusion and the degree of bradycardia. A heart rate less than 60 beats/min with poor perfusion is an indication to begin chest compressions. If the child’s heart rate is above 60 beats/min, vascular access should be obtained; resuscitative epinephrine should be administered, and it should be repeated every 3-5 min for persistent symptomatic bradycardia. If increased vagal tone (e.g., in the setting of head injury with raised intracranial pressure) or primary atrioventricular block is suspected, atropine can also be given. For cases of refractory bradycardia, cardiac pacing should be considered. During the resuscitation of a child with bradycardia, providers should assess and treat factors known to cause bradycardia, referred to collectively as the 6 Hs (hypoxia, hypovolemia, hydrogen ions [acidosis], hypokalemia or hyperkalemia, hypoglycemia, hypothermia), and 4 Ts (toxins, tamponade, tension pneumothorax, and trauma [causing hypovolemia, intracranial hypertension, cardiac compromise or tamponade]) (Table 62-5).
Table 62-5 POTENTIALLY TREATABLE CONDITIONS ASSOCIATED WITH CARDIAC ARREST
| CONDITION | COMMON CLINICAL SETTINGS | CORRECTIVE ACTIONS |
|---|---|---|
| Acidosis | Pre-existing acidosis, diabetes, diarrhea, drugs and toxins, prolonged resuscitation, renal disease, and shock |
IV, intravenously.
* Adult dose. Adjust for size of child. See Table 62-6.
From Eisenbery MS, Mengert TJ: Cardiac resuscitation, N Engl J Med 344:1304–1313, 2001.
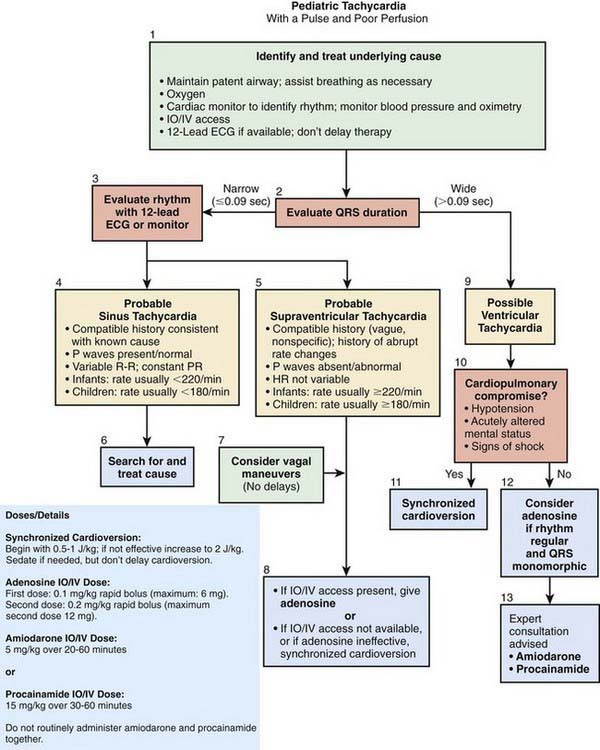
Tachyarrhythmias
As in the bradycardia algorithm, the initial management of tachycardia includes confirmation that the child has an adequate airway and life-sustaining breathing and circulation (Fig. 62-13). For children with persistent symptoms, further treatment is based on whether the QRS complex of the electrocardiogram (ECG) is narrow (≤0.08 sec) or wide (>0.08 sec). For narrow complex tachycardia, providers must distinguish between sinus tachycardia and SVT. In sinus tachycardia, (1) the history and onset are consistent with a known cause of tachycardia, such as fever or dehydration and (2) P waves are consistently present, are of normal morphology, and occur at a rate that varies somewhat. In SVT, (1) onset is often abrupt without prodrome and (2) P waves are absent or polymorphic, and when present, their rate is often fairly steady at or above 220 beats/min. For children with SVT and good perfusion, vagal maneuvers can be attempted. In cases in which SVT is associated with poor perfusion, providers should rapidly move to convert the child’s heart rhythm back to sinus rhythm. If the child already has IV access, then adenosine can be given via IV with rapid “push.” Adenosine has an extremely short half-life, so a proximal IV is best, and the adenosine should be set up with a three-way stopcock so it can be given and immediately flushed into the circulation. If the child does not have IV access, or adenosine does not successfully convert the heart rhythm back to sinus rhythm, then synchronized cardioversion, using 0.5-1 joule/kg, should be performed. In cases of wide complex tachycardia, providers should move immediately to cardioversion and increase the dose to 2 joules/kg if 1 joule/kg is not effective. As with cases of bradycardia, providers should review the 6 Hs and 4 Ts to identify factors that might be contributing to the tachycardia (see Table 62-5).
Recognition and Management of Cardiac Arrest
The initial step in CPR for a child of any age is to restore ventilation and oxygenation as quickly as possible. Upon confirmation of unresponsiveness, apnea, and pulselessness, the provider should open the airway with a head-tilt/chin-lift maneuver (or jaw-thrust if cervical spine trauma is suspected) and provide 2 initial rescue breaths (Fig. 62-14). These breaths are deep and slow, lasting approximately 1 sec per breath. The breaths are adequate if they cause the chest to rise and fall and improve the child’s color. If the breaths appear inadequate, the child should be repositioned, and the breaths delivered again. If the breaths remain ineffective, the provider should assess the child for foreign body aspiration. After 2 effective rescue breaths, the child’s pulse should be assessed. If the child has a pulse but remains apneic (or with ineffective breathing), then the rescuer should continue to provide assisted ventilation at an age-appropriate rate. Infants and children ≤8 yr old should receive rescue breathing at a rate of roughly 15-20 breaths/min, or roughly 1 breath every 3-5 sec. Children >8 yr old should receive 10-12 breaths/min, or 1 breath every 5-6 sec.

Figure 62-14 Combined jaw-thrust/spine stabilization maneuver for the pediatric trauma victim.
(From Guidelines for cardiopulmonary resuscitation and emergency cardiac care. Emergency Cardiac Care Committee and Subcommittees, American Heart Association. Part V. Pediatric basic life support, JAMA 268:2251–2261, 1992.)
If the child remains pulseless, chest compressions should be initiated. Chest compressions in infants <1 yr old may be performed by placing 2 thumbs on the midsternum with the hands encircling the thorax or by placing 2 fingers over the midsternum and compressing (Figs. 62-15 and 62-16). For children >1 yr old, the care provider should perform chest compressions over the lower half of the sternum with the heel of 1 hand, or with 2 hands as used for adult resuscitation (Fig. 62-17). In all cases, care should be taken to avoid compression of the xiphoid and the ribs. When feasible, a cardiac resuscitation board should be placed under the child’s back to maximize the efficiency of compressions. When a lone rescuer provides CPR, the universal ratio of 30 compressions to 2 ventilations is used. Pediatric patients in cardiac arrest are thought to have the best chance of survival if more frequent ventilation is offered. Therefore, the ratio should be lowered to 15 compressions to 2 ventilations for children ≤8 yr old as soon as a second care provider is available. In the outpatient setting, resuscitation effort should pause periodically to allow the provider to make an assessment of the possible return of spontaneous heart rate, pulse, and respirations. The goal of CPR is to re-establish spontaneous circulation at a level that is compatible with survival. If resuscitative efforts do not succeed in re-establishing life-sustaining breathing and circulation, the medical team must decide whether continued efforts are warranted or whether the resuscitation should be stopped. If EMS care is en route, bringing the potential for further escalation in care such as endotracheal intubation, vascular access, and medications, CPR should be continued as long as possible or deemed reasonable by the rescuers.
In the in-hospital setting, the ECG should dictate further resuscitative efforts. For children without a pulse and in asystole or electromechanical dissociation (pulseless electrical activity [PEA]), providers should continue rescue breathing and CPR, obtain vascular access, and give emergency IV epinephrine (Fig. 62-18). For continued asystole or PEA, epinephrine can be repeated every 3-5 min. Patient history, physical exam findings, and laboratory evaluation should be used to elicit correctable causes of arrest (such as the 6 Hs and 4 Ts) (see Table 62-5). CPR should be continued after epinephrine administration, to circulate the drug through the body. After 5 cycles of CPR, providers should reassess the child for the presence of a pulse or a change in the ECG rhythm that would necessitate a different response.
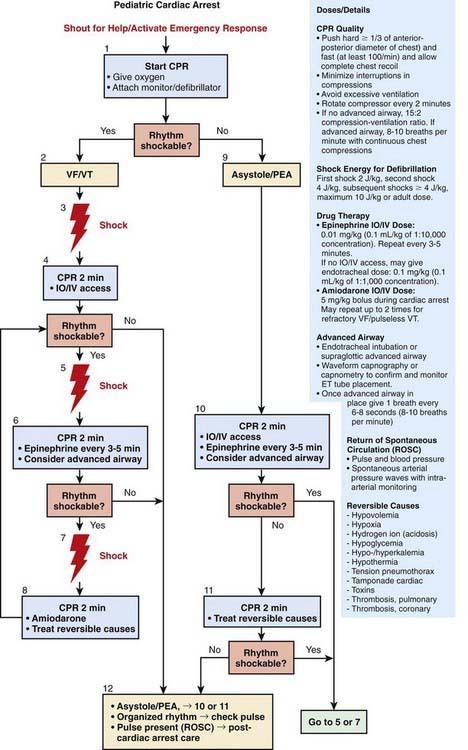
Figure 62-18 Pediatric advanced life support pulseless arrest algorithm.
(From Kleinman ME, Chameides L, Schexnayder SM, et al: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 14, Circulation 122 [suppl 3]:S876–S908, 2010, Fig 1, p S885.)
For those children with pulseless VT or VF, emergency defibrillation is indicated (see Fig. 62-18). Providers should apply the pads to the child’s bare chest and back and follow the verbal instructions given by the AED. For younger children, a defibrillator (if available) set to the dose of 2 joules/kg should be used. Ideally, the AED used in a child ≤8 yr should be equipped with an attenuated adult dose or should be designed for children; if neither device is available, a standard adult AED should be used. CPR should be immediately restarted after defibrillation. Emergency dose epinephrine can also be administered with another 5 cycles of CPR to ensure its circulation throughout the child’s body. If the ECG rhythm continues to show VF or VT, defibrillation can be alternated with epinephrine. For refractory VF or VT, an IV antiarrhythmic, such as amiodarone or lidocaine, can be given (Tables 62-6 and 62-7).
Table 62-6 MEDICATIONS FOR PEDIATRIC RESUSCITATION AND ARRHYTHMIAS
| MEDICATION | DOSE | REMARKS |
|---|---|---|
| Adenosine | 0.1 mg/kg (maximum 6 mg) | Monitor ECG |
| Repeat: 0.2 mg/kg (maximum 12 mg) | Rapid IV/IO bolus | |
| Amiodarone | 5 mg/kg IV/IO; repeat up to 15 mg/kg | Monitor ECG and blood pressure |
| Maximum: 300 mg | Adjust administration rate to urgency (give more slowly when perfusing rhythm is present) | |
| Use caution when administering with other drugs that prolong QT interval (consider expert consultation) | ||
| Atropine | 0.02 mg/kg IV/IO | Higher doses may be used with organophosphate poisoning |
| 0.03 mg/kg ET* | ||
| Repeat once if needed | ||
| Minimum dose: 0.1 mg | ||
| Minimum single dose: | ||
| Child, 0.5 mg | ||
| Adolescent, 1 mg | ||
| Calcium chloride (10%) | 20 mg/kg IV/IO (0.2 mL/kg) | Slowly |
| Adult dose: 5-10 mL | ||
| Epinephrine | 0.01 mg/kg (0.1 mL/kg 1 : 10,000) IV/IO | May repeat q3-5 min |
| 0.1 mg/kg (0.1 mL/kg 1 : 1,000) ET* | ||
| Maximum dose: 1 mg IV/IO; 10 mg ET | ||
| Glucose | 0.5-1 g/kg IV/IO | D10W: 5-10 mL/kg |
| D25W: 2-4 mL/kg | ||
| D50W: 1-2 mL/kg | ||
| Lidocaine | Bolus: 1 mg/kg IV/IO | |
| Maximum dose: 100 mg | ||
| Infusion: 20-50 µg/kg/min | ||
| ET*: 2-3 mg | ||
| Magnesium sulfate | 25-50 mg/kg IV/IO over 10-20 min; faster in Torsades de pointes | |
| Maximum dose: 2g | ||
| Naloxone | <5 yr or ≤20 kg: 0.1 mg/kg IV/IO/ET* | Use lower doses to reverse respiratory depression associated with therapeutic opioid use (1-15 µg/kg) |
| ≥5 yr or >20 kg: 2 mg IV/IO/ET* | ||
| Procainamide | 15 mg/kg IV/IO over 30-60 min | Monitor EGG and blood pressure |
| Adult dose: 20 mg/min IV infusion up to total maximum dose of 17 mg/kg | Use caution when administering with other drugs that prolong QT interval (consider expert consultation) | |
| Sodium bicarbonate | 1 mEq/kg/dose IV/IO slowly | After adequate ventilation |
ECG, electrocardiogram; ET, endotracheal tube; IO, intraosseous; IV, intravenous.
* Flush with 5 mL of normal saline and follow with 5 ventilations.
From ECC Committee, Subcommittees and Task Forces of the American Heart Association: 2005 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, Circulation 112:IV1–203, 2005.
Table 62-7 MEDICATIONS TO MAINTAIN CARDIAC OUTPUT AND FOR POST-RESUSCITATION STABILIZATION*
| MEDICATION | DOSE RANGE | COMMENT |
|---|---|---|
| Inamrinone | 0.75-1 mg/kg IV/IO over 5 min; may repeat 2×; then: 2-20 µg/kg/min | Inodilator |
| Dobutamine | 2-20 µg/kg/min IV/IO | Inotrope; vasodilator |
| Dopamine | 2-20 µg/kg/min IV/IO in low doses; pressor in higher doses | Inotrope; chronotrope; renal and splanchnic vasodilator |
| Epinephrine | 0.1-1 µg/kg/min IV/IO | Inotrope; chronotrope; vasodilator in low doses; vasopressor in higher doses |
| Milrinone | 50-75 µg/kg IV/IO over 10-60 min then 0.5-0.75 µg/kg/min | Inodilator |
| Norepinephrine | 0.1-2 µg/kg/min | Inotrope; vasopressor |
| Sodium nitroprusside | 1-8 µg/kg/min | Vasodilator; prepare only in D5W |
IO, intraosseous; IV, intravenous.
* Alternative formula for calculating an infusion: Infusion rate (mL/hr) = [weight (kg) × dose (µg/kg/min) × 60 (min/hr)]/concentration µg/mL).
From ECC Committee, Subcommittees and Task Forces of the American Heart Association: 2005 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, Circulation 112:IV1–203, 2005.
Vascular Access
Venous Access
Veins suitable for cannulation are numerous, but there is considerable anatomic variation from patient to patient. In the upper extremities, the median antecubital vein, located in the antecubital fossa, is often the largest and easiest to access (Fig. 62-19). Many veins on the dorsum of the hand are also suitable for cannulation because they are often large and easily located on the flat surface of the dorsum of the hand, and their cannulation is well tolerated. The cephalic vein is usually cannulated at the wrist, along the forearm, or at the elbow. The median vein of the forearm is also suitable because it lies along a flat surface of the forearm. In the lower extremity, the great saphenous vein, located just anterior to the medial malleolus, is accessible in most patients. The dorsum of the foot usually has a large vein in the midline, passing across the ankle joint, but catheters are difficult to maintain in this vein because dorsiflexion tends to dislodge them. A second large vein on the lateral side of the foot, running in the horizontal plane, usually 1-2 cm dorsal to the lower margin of the foot, is preferable (Fig. 62-20). The most notable scalp veins are the superficial temporal (just anterior to the ear) and posterior auricular (just behind the ear).
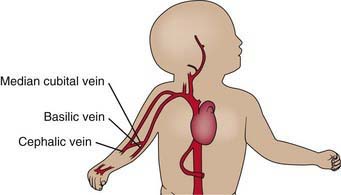
Figure 62-19 Veins of the upper extremity.
(From Roberts JR, Hedges JR, editors: Clinical procedures in emergency medicine, ed 4, Philadelphia, 2004, Saunders.)
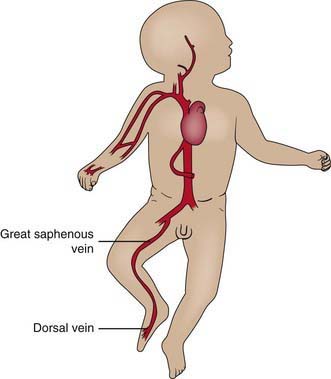
Figure 62-20 Veins of the lower extremity.
(From Roberts JR, Hedges JR, editors: Clinical procedures in emergency medicine, ed 4, Philadelphia, 2004, Saunders.)
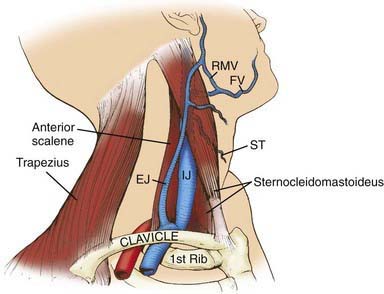
Deeper and larger central veins can provide more reliable, larger-bore access for medications, nutritive solutions, and blood sampling than peripheral venous lines. They may be reached by percutaneous cannulation or surgical exposure. In infants and young children, the femoral vein is often the easiest to access and cannulate, but the internal jugular and subclavian veins may also be used (Figs. 62-21 and 62-22). Because of its proximity to the median nerve, the brachial vein is not often recommended for cannulation.
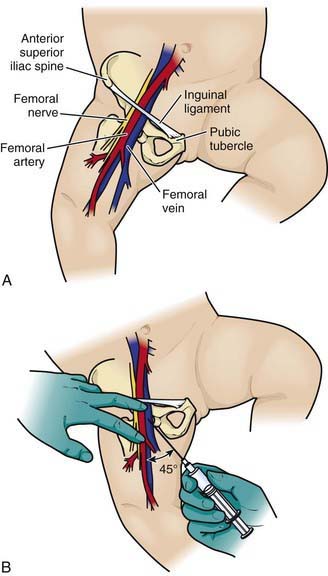
Figure 62-21 Femoral vein approach. Remember the mnemonic NAVEL for nerve, artery, vein, empty space, and lymphatics.
(From Putigna F, Solenberger R: Central venous access [website]. http://emedicine.medscape.com/article/940865-overview. Accessed February 7, 2011.)
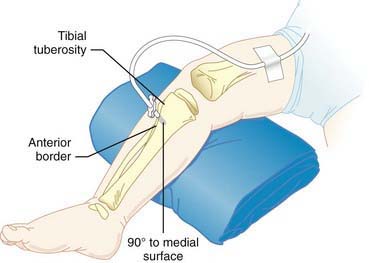
Intraosseous Access
Intraosseous (IO) needles are special rigid, large-bore needles that resemble those used for bone marrow aspiration. IO cannulation is recommended for patients for whom IV access proves difficult or unattainable, even in older children. If venous access is not available within 1 min in a child with cardiopulmonary arrest, an IO needle should be placed in the anterior tibia (with care taken to avoid traversing the epiphyseal plate). The needle should penetrate the anterior layer of compact bone, and its tip advanced into the spongy interior of the bone (Fig. 62-23). Any and all medications, blood products, and fluids may be administered through this route, including those involved in emergency resuscitations.
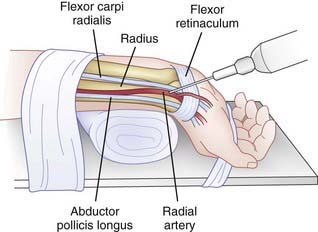
Arterial Access
Arterial access is indicated when care providers need frequent blood sampling, particularly to assess adequacy of oxygenation, ventilation, or acid-base balance, and/or continuous blood pressure monitoring. The radial artery, the most commonly cannulated artery, lies on the lateral side of the anterior wrist, just medial to the styloid process of the radius (Fig. 62-24). The ulnar artery, just lateral to the tendon of the flexor carpi ulnaris, is used less often because of its proximity to the ulnar nerve. Useful sites in the lower extremity, particularly in neonates and infants, are the dorsalis pedis artery, on the dorsum of the foot between the tendons of the tibialis anterior and the extensor hallucis longus, and the posterior tibial artery, posterior to the medial malleolus. Arterial catheters require special care for insertion and subsequent management because the blood flow to tissue can be compromised and considerable hemorrhage can occur if an arterial catheter is dislodged.
Post-Resuscitation Care
Induced hypothermia (32-33°C for ≈ 24 hr) has been used in adult and pediatric survivors of CPR in an attempt to reduce the high neurologic impairment seen in survivors of cardiac arrest (Chapter 63). Hypoxic-ischemic encephalopathy with subsequent development of seizures, intellectual impairment, and spasticity is a serious and common complication of cardiac arrest. In addition hyperglycemia and hypoglycemia should be avoided.
Post-resuscitation management generally has two phases, similar to earlier, emergency resuscitative care. First, the providers must assess the child’s airway and breathing and must support oxygenation and ventilation as indicated. If the child has ongoing respiratory failure and has been supported with bag-valve-mask ventilation until this time, the providers should now move forward with intubation. Once the child is intubated, mechanical ventilation must be established, and respiratory assessments performed, such as chest radiography and arterial blood gas sampling and analysis. The child’s circulatory system must also be assessed and supported as needed. Continuous arterial blood pressure monitoring can help the provider determine the need for, and response to, inotropic and chronotropic medications (see Table 62-7). Once the ABCs have been managed, providers can move on to full organ system assessments. A systematic approach that employs a full physical exam and laboratory evaluation to reveal the child’s respiratory, cardiovascular, neurologic, gastrointestinal, renal, and hematologic system function should be used.
American Academy of Pediatrics Committee on Pediatric Emergency MedicineAmerican Academy of Pediatrics Section on Cardiology and Cardiac SurgeryMarkenson D. Ventricular fibrillation and the use of automated external defibrillators on children. Pediatrics. 2007;120:1159-1161.
American Heart Association. American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: pediatric advanced life support. Pediatrics. 2006;117:e1005-e1028.
Berg MD, Schexnayder SM, Chameides L, et al. Pediatric basic life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics. 2010;126:e1345-e1360.
Bobrow BJ, Clark LL, Ewy GA, et al. Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. JAMA. 2008;299:1158-1165.
Bohn K, Rosenqvist M, Herlitz J, et al. Survival is similar after standard treatment and chest compression only in out-of-hospital bystander cardiopulmonary resuscitation. Circulation. 2007;116:2908-2912.
Boyd R. Witnessed resuscitation by relatives. Resuscitation. 2000;43:171-176.
Carcillo JA, Kuch BA, Han YY, et al. Mortality and functional morbidity after use of PALS/APLS by community physicians. Pediatrics. 2009;124:500-508.
Council on School Health. Medical emergencies occurring at school. Pediatrics. 2008;122:887-894.
Doherty DR, Parshuram CS, Gaboury I, et al. Hypothermia therapy after pediatric cardiac arrest. Circulation. 2009;119:1492-1500.
Durbin WJ, Stille C. Pneumonia. Pediatr Rev. 2008;29:147-158. quiz 159–160
ECC Committee, Subcommittees and Task Forces of the American Heart Association. 2005 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2005;112:IV1-IV203.
Ewy GA. Cardiac arrest—guideline changes urgently needed. Lancet. 2009;369:882-884.
Gattinoni L, Caironi P, Cressoni M, et al. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. 2006;354:1775-1786.
Hegenbarth MA. American Academy of Pediatrics Committee on Drugs: Preparing for pediatric emergencies: drugs to consider. Pediatrics. 2008;121:433-443.
Herlitz J, Engdahl J, Svensson L, et al. Characteristics and outcome among children suffering from out of hospital cardiac arrest in Sweden. Resuscitation. 2005;64:37-40.
Horton MA, Beamer C. Powered intraosseous insertion provides safe and effective vascular access for pediatric emergency patients. Pediatr Emerg Care. 2008;24:347-350.
Kleinman ME, Chameides L, Schexnayder SM, et al. Pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics. 2010;126:e1361-e1399.
Kleinman ME, de Caen AR, Chameides L, et al. Pediatric basic and advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Pediatrics. 2010;126:e1261-e1318.
Lopez-Herce J, Alvarez AC. Bystander CPR for paediatric out-of-hospital cardiac arrest. Lancet. 2010;375:1321-1322.
Lopez-Herce J, Garcia C, Rodriguez-Nunez A, et al. Long-term outcome of paediatric cardiorespiratory arrest in Spain. Resuscitation. 2005;64:79-85.
Maconochie I, Dawood M. Manchester triage system in paediatric emergency care. BMJ. 2008;337:767-768.
Markenson D, Pyles L, Neish S, et al. Ventricular fibrillation and use of automated external defibrillators on children. Pediatrics. 2007;120:e1368-e1379.
Mentzelopoulos SD, Zakynthinos SG, Tzoufi M, et al. Vasopressin, epinephrine, and corticosteroids for in-hospital cardiac arrest. Arch Intern Med. 2009;169:15-24.
Morley P. New international guidelines on resuscitation. BMJ. 2010;341:902.
Nagele P. Augmented CPR: rescue after the ResQ trial. Lancet. 2011;377:276-277.
Ogawa T, Akahane M, Koike S, et al. Outcomes of chest compression only CPR versus conventional CPR conducted by lay people in patients with out of hospital candiopulmonary arrest witnessed by bystanders: nationwide population based abservational study. BMJ. 2011;342:321.
Padman R, Lawless ST, Kettrick RG. Noninvasive ventilation via bilevel positive airway pressure support in pediatric practice. Crit Care Med. 1998;26:169-173.
Pell JP, Sirel M, Marsden AK, et al. Presentation, management, and outcome of out of hospital cardiopulmonary arrest: comparison by underlying etiology. Heart. 2003;89:839-842.
Ralston M, Hazinski MF, Zaritsky ALet al, editors. Pediatric advanced life support course guide and PALS provider manual: provider manual. Dallas: American Heart Association, 2007.
Rea TD, Fahrenbruch C, Calley L, et al. CPR with chest compression alone or with rescue breathing. N Engl J Med. 2010;363(5):423-432.
Robinson SM, Mackenzie-Ross S, Campbell Hewson GL, et al. Psychological effect of witnessed resuscitation on bereaved relatives. Lancet. 1998;352:614-617.
Sharek PJ, Parast LM, Leong K, et al. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a children’s hospital. JAMA. 2007;298:2267-2274.
Topjian AA, Berg RA, Nadkami VN. Pediatric cardiopulmonary resuscitation: advances in science, techniques, and outcomes. Pediatrics. 2008;122:1086-1098.
Vilke GM, Smith AM, Ray LU, et al. Airway obstruction in children aged less than 5 years: the prehospital experience. Prehosp Emerg Care. 2004;8:196-199.
Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med. 2000;342:1334-1349.
Wik L, Hansen TB, Fylling F, et al. Delaying defibrillation to give basic cardiopulmonary resuscitation to patients with out-of-hospital ventricular fibrillation: a randomized trial. JAMA. 2003;289:1389-1395.