W2 A Patient-Focused Wrist Outcome Instrument—the Adelaide Questionnaire
Measuring the outcome after distal radius fracture is an essential part of clinical practice.1,2 The primary purpose is to provide information regarding the response of the patient to fracture management and rehabilitation.3 This information is used for other purposes as well, such as to focus clinical practice by assisting with setting of treatment goals, developing management plans, aiding with patient motivation,4,5 justifying service provision, documenting continuous improvement strategies, and benchmarking.6,7
Outcome measurement after distal radius fracture is a challenging activity because the wrist is an anatomically compact and biomechanically complex region of the body.8 Little is known about the bony morphology and capsular, ligamentous, and muscular contributions to wrist function compared with other joints, such as the knee and the hip. Preliminary findings on wrist kinematics and proprioception have been reported more recently.9–12 Further work in these areas and in the musculotendinous contribution to wrist stability and motion is required, however, so that outcome instruments accurately reflect the structure and function of the wrist.
Many instruments have been developed to evaluate the outcome after distal radius fracture.13 Until the late 1990s, these instruments primarily assessed impairments, such as wrist range of motion, grip strength, and pain. In theory, however, a linear relationship does not exist between wrist impairments, such as range of wrist motion, and the ability to perform daily activities.14 An extreme clinical example is after total wrist fusion, when patients have no wrist movement. Most patients report, however, that they are able to perform most daily activities despite this impairment.15 Consequently, there has been a shift over the past decade to evaluate functional aspects of a wrist disorder, by specifically gathering information from patients regarding their ability to perform daily activities.16 This information is most frequently gained from administration of a standardized, clinimetrically sound questionnaire.1 This procedure also directly evaluates why patients present for treatment because their wrist typically interferes with their ability to perform daily activities.15,17
Four questionnaires are currently used in clinical practice to evaluate the outcome after distal radius fracture: the Disabilities of the Arm, Shoulder, and Hand (DASH),18 the patient-rated wrist evaluation (PRWE),19 the Michigan Outcomes Questionnaire (MHOQ),20 and the Modified Mayo Wrist Scoring System.21 The Modified Mayo Wrist Scoring System evaluates four variables—pain, satisfaction, range of motion, and grip strength—and does not evaluate the patient’s ability to perform daily activities. Scores for these variables are tallied and categorized as excellent, good, fair, and poor. This scoring system reports the end result of treatment, without a point of reference to baseline data. Baseline data are important so that magnitude of change that has occurred during the treatment period can be evaluated5,22 because not all individuals are symptom-free before distal radius fracture.23,24 For these reasons, the Modified Mayo Wrist Scoring System may be able to discriminate between individuals based on the final result of impairment variables, but cannot evaluate change in the ability to perform daily activities over time in individuals with distal radius fractures.
DASH, PRWE, and MHOQ are used in clinical and research settings to evaluate impairments (e.g., pain intensity) and the functional consequences (i.e., the ability to perform daily activities) after distal radius fracture.25–27 Anecdotal reports suggest that there are three major limitations of these questionnaires, all which center around the evaluation of daily activities:
Development of the Adelaide Questionnaire
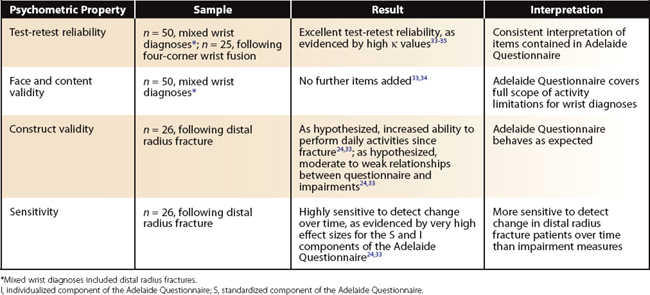
A new wrist outcome instrument, the Adelaide Questionnaire, was developed to address the limitations of existing instruments.33 Specifically, the Adelaide Questionnaire assesses from the patient’s perspective the actual ability to perform daily activities after distal radius fracture and other unilateral musculoskeletal wrist disorders. The questionnaire was developed based on the results of a large qualitative study of individuals with wrist injuries23,33 and has undergone subsequent psychometric evaluation with excellent results (Table W2-1).24,33–35
The Adelaide Questionnaire consists of three components (Fig. W2-1), as follows34:
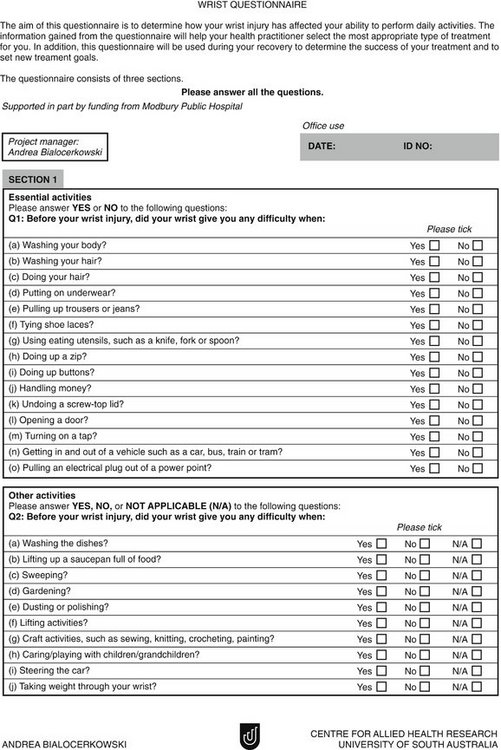
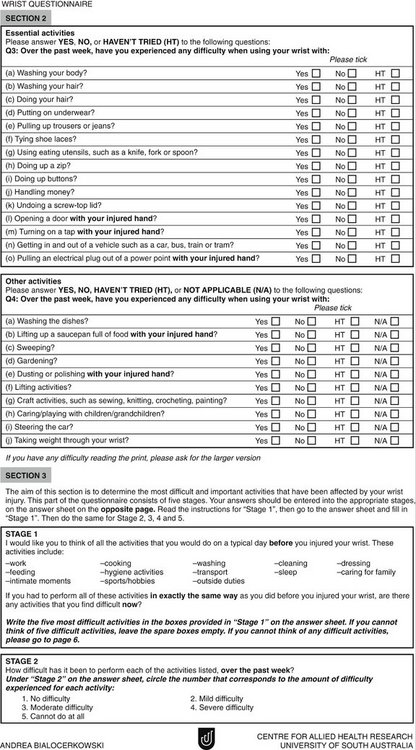
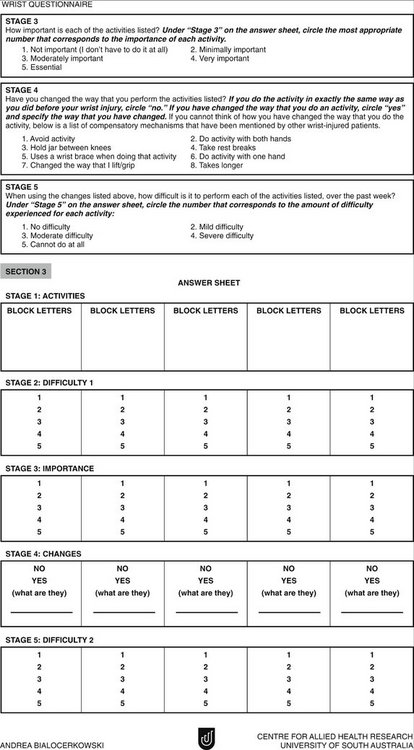
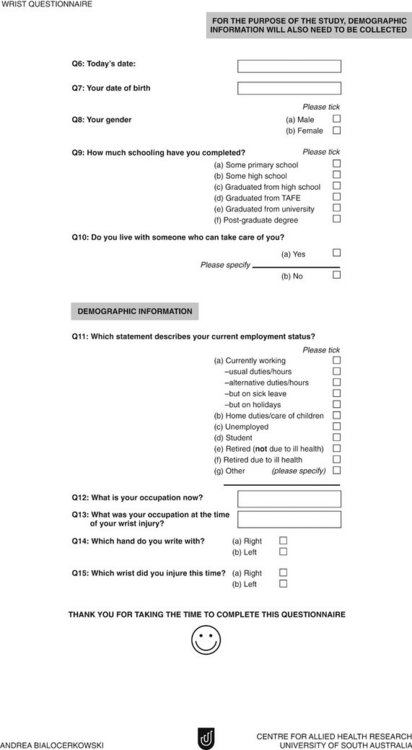
FIGURE W2-1 The Adelaide Questionnaire.
From Bialocerkowski,33 reproduced with permission from Andrea Bialocerkowski.
Detailed instructions regarding scoring of the Adelaide Questionnaire can be found in the article by Bialocerkowski and colleagues.34
Clinical Application of the Adelaide Questionnaire to Patients after Distal Radius Fracture
The Adelaide Questionnaire has been used in clinical practice to document the recovery trajectory after distal radius fracture in terms of specific activity limitations and compensatory mechanisms used.24,32,33 Adult patients with a unilateral distal radius fracture with or without ulna fracture from public and private health care providers throughout Adelaide, Australia, were evaluated in 2000, using the Adelaide Questionnaire and other measures (see later) during the first 6 months following distal radius fracture. Recovery trajectories of patients residing in nursing homes or patients with coexisting medical disorders (e.g., rheumatoid arthritis, cerebrovascular accident, bilateral wrist disorders, concomitant disorders of the hand or upper limb) were not documented because these factors would likely influence their ability to perform daily activities and their goals of treatment. Likewise, data from individuals with little comprehension of written English were not collated because they might experience difficulty completing the Adelaide Questionnaire.
TABLE W2-2 Clinical Tests Used to Evaluate Patients after Distal Radius Fracture
| Clinical Test | Equipment | Protocol |
|---|---|---|
| Active wrist/forearm range of motion; wrist flexion; wrist extension; radial deviation; ulnar deviation; pronation; supination | Plastic hand-held goniometer | ASHT Clinical Assessment Recommendations37 |
| Strength; grip; pinch | Jamar dynamometer; Preston Pinch Meter | ASHT Clinical Assessment Recommendations38; Macey and Burke39 |
| Light touch sensation | Semmes-Weinstein monofilaments (mini-kit) | ASHT Clinical Assessment Recommendations40 |
ASHT, American Society of Hand Therapists.
Patients
Fifty-three patients contributed data for the recovery trajectories, with 26 patients having four assessments at 8, 12, 18, and 24 weeks after fracture.33 The demographic characteristics of the patients are representative of a population who sustain distal radius fractures—mainly women 40 to 65 years old (Table W2-3).41,42
TABLE W2-3 Demographic Characteristics of Distal Radius Fracture Patients
| Demographic Characteristic | All Patients | Patients with Four Assessments |
|---|---|---|
| Total no. participants | 53 | 26 |
| Age (yr) | ||
| Mean (SD) | 61.7 (15.7) | 61.8 (15.2) |
| Range | 22-87 | 22-84 |
| Gender | ||
| Female | 46 (87%) | 22 (85%) |
| Male | 7 (13%) | 4 (15%) |
| Dominance of injury | ||
| Dominant wrist | 23 (43%) | 12 (46%) |
| Nondominant wrist | 30 (57%) | 14 (54%) |
| Education | ||
| Some primary school | 8 (15%) | 3 (12%) |
| Some high school | 20 (38%) | 10 (38%) |
| Graduated from high school | 18 (34%) | 10 (38%) |
| Graduated from TAFE | 3 (6%) | 1 (4%) |
| Graduated from university | 2 (3.5%) | 1 (4%) |
| Postgraduate degree | 2 (3.5%) | 1 (4%) |
| Employment status | ||
| Employed | 14 (26%) | 6 (23%) |
| Homemaker | 33 (62%) | 17 (65%) |
| Retired | 3 (6%) | 1 (4%) |
| Retired because of illness | 1 (2%) | 1 (4%) |
| Unemployed | 1 (2%) | 1 (4%) |
| Student | 1 (2%) | 0 (0%) |
| Occupational change owing to wrist disorder | ||
| No | 53 (100%) | 26 (100%) |
| Yes | 0 (0%) | 0 (0%) |
| Lives with caregiver | ||
| No | 21 (40%) | 8 (31%) |
| Yes | 32 (60%) | 18 (69%) |
| Previous wrist injury | ||
| No | 42 (81%) | 21 (81%) |
| Yes | 11 (19%) | 5 (19%) |
| Medical treatment received | ||
| Plaster only | 31 (58%) | 13 (50%) |
| Other treatment | 22 (42%) | 13 (50%) |
| Physiotherapy received | ||
| No | 24 (45%) | 10 (38%) |
| Yes | 29 (55%) | 16 (62%) |
TAFE, Australia’s technical and further education institutes.
Adapted from Bialocerkowski A, Grimmer K, Bain G: Validity of the patient-focused wrist outcome instrument: do impairments represent functional ability? Hand Clin. 2003;19:449-455.
Ability to Perform Daily Activities before Fracture
A common clinical observation is that some patients report difficulty performing daily activities before their distal radius fracture.24,33 This observation is supported by our data, where 13% of patients (n = 7) reported difficulty performing one or more daily activities before fracture. Undoing a screw-top lid of a jar and making weight through the wrist were the most frequently reported daily activities (Table W2-4). Not everyone is symptom-free before their current wrist disorder,23,31,33 and a baseline measure such as this should be established to guide treatment expectations. The goal of treatment after distal radius fracture is to restore function to preinjury level. It is realistic to expect that these patients would experience difficulty performing the same daily activities as before distal radius fracture. Clinically, this expectation is frequently communicated to patients. Currently used outcome measures, such as DASH, PRWE, and MHOQ, do not quantify outcome with respect to preinjury status, and assume that all patients should attain full recovery.
TABLE W2-4 Difficult Daily Activities before Current Distal Radius Fracture (n = 53)
| Daily Activity | Frequency of Report | Percentage Report |
|---|---|---|
| Undoing a screw-top lid | 3 | 6 |
| Taking weight through the wrist | 3 | 6 |
| Turning on a tap | 2 | 4 |
| Lifting up a saucepan full of food | 2 | 4 |
| Washing the dishes | 1 | 2 |
| Lifting activities | 1 | 2 |
From Bialocerkowski,33 reproduced with permission from Andrea Bialocerkowski.
Difficulty Performing Daily Activities 8 to 24 Weeks after Fracture
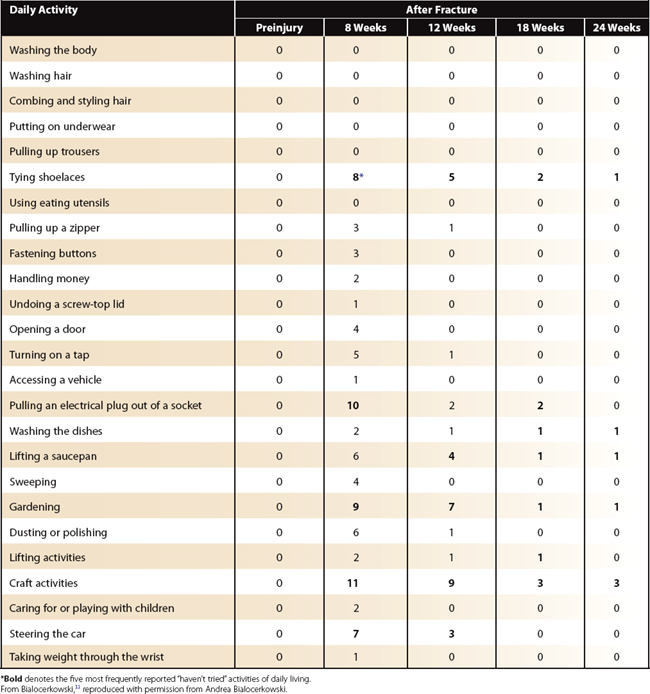
Clinicians observe that all patients report difficulty performing daily activities 8 weeks after distal radius fracture, and their functional ability increases with time since fracture.43 Little is known, however, about the specific daily activities that are problematic. We found that all patients (n = 53) reported difficulty performing daily activities initially following distal radius fracture. The most frequently reported difficult daily activities, in the standardized component of the Adelaide Questionnaire, initially were taking weight through the wrist (88%), using eating utensils (88%), lifting activities (85%), undoing a screw-top lid of a jar (85%), lifting a saucepan (77%), and turning on a tap (77%) (Table W2-5).33
TABLE W2-5 Frequency of Difficult Daily Activities in the Standardized Component of the Adelaide Questionnaire at 8, 12, 18, and 24 Weeks after Distal Radius Fracture (n = 26)
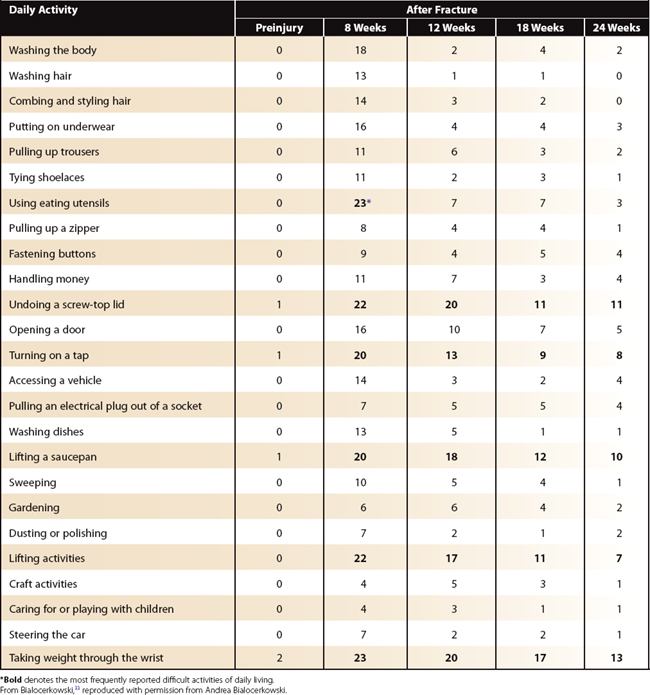
Recovery of the performance of these daily activities depended on the time since fracture and the daily activity.33 The number of patients reporting difficulty using eating utensils decreased rapidly (between 8 and 12 weeks after fracture), and very few patients reported difficulty with this activity at 24 weeks after fracture (n = 3 [11%]). In contrast, the ability to take weight through the wrist recovered more slowly over 6 months after fracture. At 24 weeks after fracture, 50% of patients still reported difficulty with this daily activity. Other frequently reported difficult activities at 24 weeks after fracture include undoing a screw-top lid of a jar (42%), lifting a saucepan (38%), and turning on a tap (31%) (see Table W2-5). At 6 months after distal radius fracture, patients generally have not reached their preinjury status.24,33
To illustrate the concept of different daily activities recovering at different rates after fracture, percentage change statistics were calculated for assessments at 12, 18, and 24 weeks after fracture compared with the assessment at 8 weeks after fracture.33 This comparison identified daily activities that were most likely to change over these assessment periods. To evaluate accurately the ability to perform daily activities at 24 weeks after fracture, the 11 sensitive activities listed in the last column of Table W2-6 should be evaluated. If a patient experiences difficulty with any of these activities, this indicates slower recovery. Only one of these daily activities is included, however, in currently used wrist outcome instruments (DASH and the PRWE include an item on using eating utensils) (Table W2-7). Currently used wrist outcome instruments do not contain an evaluation of daily activities that are sensitive to change in the first 6 months after distal radius fracture. Consequently, they may not provide an appropriate evaluation of outcome during this time.
TABLE W2-6 Most Sensitive Daily Activities to Detect Change in Function after Distal Radius Fracture (n = 26)
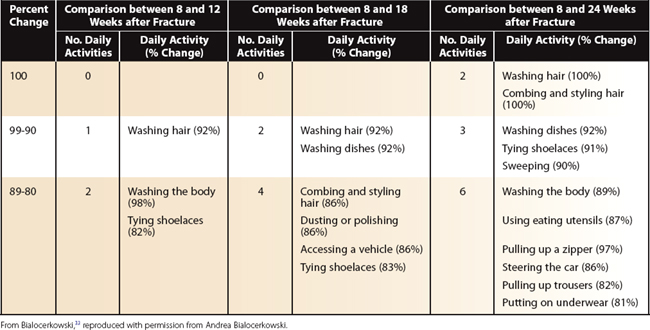
TABLE W2-7 Comparison of the Daily Activity Items Evaluated in the Adelaide Questionnaire, DASH, PRWE, and MHOQ
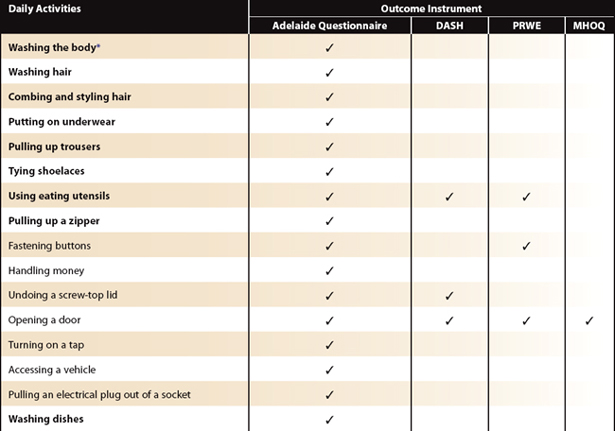
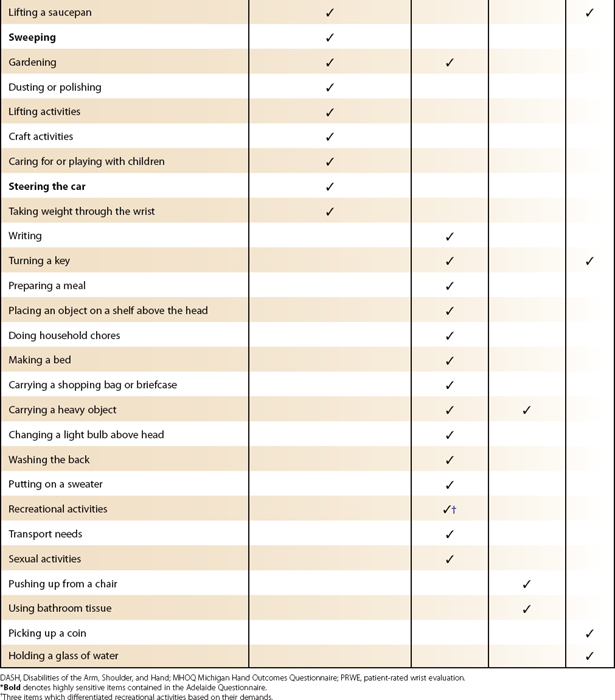
Clinically, patients also report difficulties with other daily activities that are not contained in standardized outcome measures, such as DASH, PRWE, the MHOQ, or the standardized component of the Adelaide Questionnaire. We found that the individualized component of the Adelaide Questionnaire provided additional information regarding activity limitations experienced by our patients. Ninety-one percent of our patients completed this component (n = 48), and reported that difficulty was frequently experienced with preparing vegetables (n = 26), carrying objects (n = 16), using a computer (n = 15), making a bed (n = 12), and mopping a floor (n = 12).33 Only one of these daily activities, carrying a heavy object, is contained in currently used wrist outcome instruments (DASH and PRWE) (see Table W2-7). Currently used wrist outcome instruments are unlikely to capture important, difficult daily activities that are specific to each patient. These activities are often brought to light during clinical examination of the patient. The Adelaide Questionnaire provides a standardized and structured means of evaluating and tracking change (improvement/no change/deterioration) in these daily activities.
Evaluation of Actual Ability
In clinical practice, we frequently ask patients what they have difficulty doing, not what they could have difficulty doing. Clinicians evaluate actual ability. In contrast, currently used wrist outcome instruments request patients to provide the best estimate if they have not performed the daily activity during the past week. This question evaluates performance, which is not equivalent to actual ability.28 Another frequent clinical observation is that not all patients attempt to perform the same daily activities at the same time during their rehabilitation. These measurement issues are overcome in the Adelaide Questionnaire because it evaluates actual ability by using the following two response options: “haven’t tried” and “not applicable.”
Patients at 8 weeks after distal radius fracture reported that they “haven’t tried” craft activities (42%), pulling an electrical plug out of a socket (38%), gardening (35%), and tying shoe laces (31%). The frequency of “haven’t tried” daily activities decreased throughout the rehabilitation period with most activities being attempted by 24 weeks after fracture. Craft activities were not attempted by three patients at 24 weeks after fracture (Table W2-8).33 This information indicates that these patients are recovering at a slower rate than expected, and they may lack confidence with daily activities. Gaining information on daily activities that have not been attempted substantiates clinical opinion regarding the speed of recovery and provides information for clinical decision making regarding management strategies. The Adelaide Questionnaire is the only standardized method of documenting use of the wrist and hand over time since distal radius fracture.
TABLE W2-8 Frequency of “Haven’t Tried” Responses on the Standardized Component of the Adelaide Questionnaire at 8, 12, 18, and 24 Weeks after Distal Radius Fracture (n = 26)
Clinically, we know that not all patients perform the same daily activities on a regular basis. This contention is supported from the results of the “not applicable” analyses, where six daily activities were not normally undertaken by at least one patient (Table W2-9).33 This phenomenon is likely to occur in other wrist outcome measures, but is not accounted for or evaluated. Because of this, the other outcome measures may provide an inaccurate measure of outcome.
TABLE W2-9 Daily Activities That Were “Not Applicable” in the Standardized Component of the Adelaide Questionnaire (n = 53)
| Daily Activity | Frequency of Report | Percent Report |
|---|---|---|
| Caring for or playing with children | 25 | 47 |
| Steering the car | 14 | 26 |
| Craft activities | 13 | 25 |
| Gardening | 11 | 21 |
| Sweeping | 3 | 6 |
| Dusting or polishing | 2 | 4 |
Use of Compensatory Mechanisms
Patients frequently report that they alter the way in which they perform daily activities by using compensatory mechanisms.23,31 We found that compensatory mechanisms were used for 94% of the daily activities specified in the individualized component of the Adelaide Questionnaire. Using the other hand, taking longer, and avoiding the daily activity were most frequently used compensatory mechanisms (Table W2-10).33 The types of compensatory mechanisms used to allow performance of daily activities changed over time (Table W2-11). At 8 and 12 weeks after distal radius fracture, a change in grip was the most frequently used compensatory mechanism. At 18 and 24 weeks after fracture, taking longer to perform the daily activity was most frequently reported.33,34 Patients may have been unable to use their affected wrist and hand in the early rehabilitation period. As time increased since fracture, patients began to use their affected wrist and hand at a slower rate compared with preinjury. The proportion of daily activities that are avoided remains constant, however, over the 6-month period since fracture. The ability to perform priority daily activities does not recover completely within 6 months after distal radius fracture.
TABLE W2-10 Eight Most Frequently Reported Compensatory Mechanisms Reported in the Individualized Component of the Adelaide Questionnaire
| Compensatory Mechanism | Frequency of Report | Percent Report |
|---|---|---|
| Uses one hand | 130 | 29 |
| Takes longer | 118 | 26 |
| Avoidance | 86 | 19 |
| Change in grasp | 49 | 11 |
| Assistance | 33 | 7 |
| Care required | 16 | 3 |
| Does less | 13 | 3 |
| Uses both hands | 12 | 2 |
From Bialocerkowski,33 reproduced with permission from Andrea Bialocerkowski.
TABLE W2-11 Frequency of Compensatory Mechanism Use over Time, Reported in the Individualized Component of the Adelaide Questionnaire (n = 26)
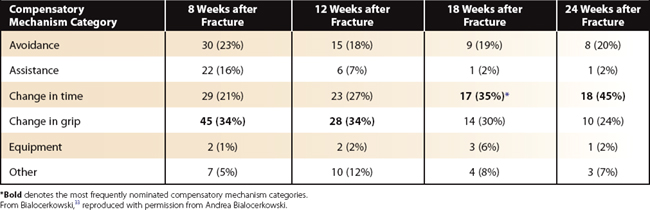
These findings have implications for clinical practice. First, as the type of compensatory mechanism changes over time since fracture, regular monitoring of compensatory mechanism use is required to ensure that increased stress is not placed on other parts of the body, and that daily activities are not avoided for extended periods. Unnecessary avoidance of daily activities may result in additional deconditioning of the wrist musculature. Performance of daily activities can be thought of as therapeutic exercise. Second, the use of compensatory mechanisms can have an impact on patients’ lifestyles and their satisfaction with their management. Three female patients reported that they changed their hairstyle after distal radius fracture because they were unable to style their hair satisfactorily (Table W2-12). They were unhappy with their more manageable hairstyle, however, which decreased their satisfaction with management of their wrist. Factors other than impairments have an impact on satisfaction. Third, MHOQ is the only currently used wrist outcome measure that evaluates compensatory mechanism use, but its evaluation is simplistic. The Adelaide Questionnaire is the only method to document in a standardized, detailed manner the compensatory mechanisms used for daily activities, and how they change over time.
TABLE W2-12 Other Compensatory Mechanisms Reported in the Individualized Component of the Adelaide Questionnaire (n = 53)
| Compensatory Mechanism | Frequency of Report |
|---|---|
| Fastening bra at the front instead of behind back | 6 |
| Change diet | 4 |
| Change hairstyle | 3 |
| Shower instead of taking a bath | 2 |
| Keep bra hooks fastened | 2 |
| Fill jug with small cups of water | 1 |
| Leave dishes on the drainer instead of drying them | 1 |
| Change sleeping position | 1 |
| Hang washing instead of on the line | 1 |
| Put on socks instead of stockings | 1 |
| Put money in pocket instead of using a purse | 1 |
From Bialocerkowski,33 reproduced with permission from Andrea Bialocerkowski.
Relationship between Ability to Perform Daily Activities and Impairments
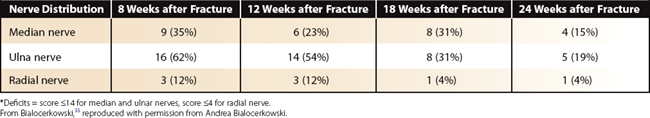
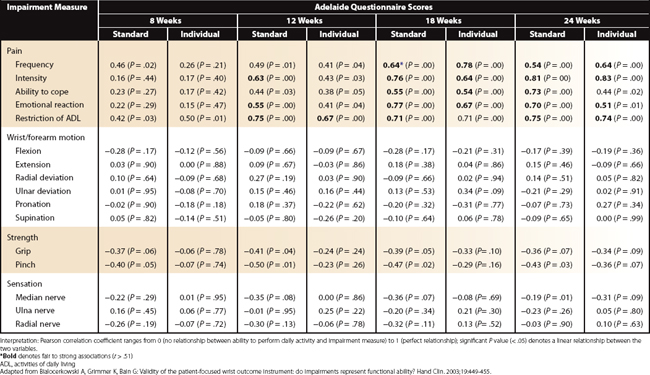
Impairments after distal radius fracture are routinely evaluated in clinical practice. Our patients, similar to others with distal radius fractures,33 had mild wrist pain and significant wrist motion and hand strength impairments at 8 weeks after distal radius fracture. These reduced over time since fracture (Tables W2-13, W2-14, and W2-15).33 Little is known, however, about the relationship between impairments and activity limitations. We found that there is only a moderate to weak relationship between the Adelaide Questionnaire scores and impairment measures, regardless of the time since assessment (Table W2-16).24,33 Pain constructs had the strongest association with the questionnaire scores, especially “restriction of activity of daily living due to pain.” At most, however, this pain construct predicts only 56% of the ability to perform daily activities. The relationship between other impairment measures and questionnaire scores was much weaker and predicts a much smaller percentage of the ability to perform daily activities. Impairments should not be used to predict performance, and the performance of daily activities should be evaluated directly, using standardized outcome instruments. In addition, outcome instruments such as the Modified Mayo Wrist Scoring System,21 which exclusively evaluates impairments, may provide an inappropriate measure of outcome for distal radius fracture patients.
TABLE W2-13 Mean (SD) for Each Pain Construct after Distal Radius Fracture Measured by the Glasgow Pain Questionnaire (n = 26)
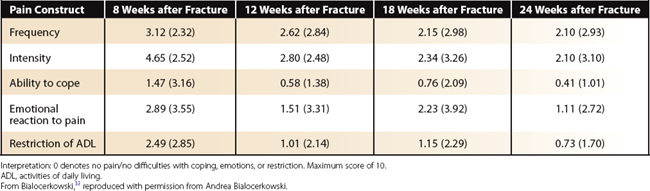
TABLE W2-14 Mean (SD) Active Wrist and Forearm Motion and Grip and Pinch Strength after Distal Radius Fracture
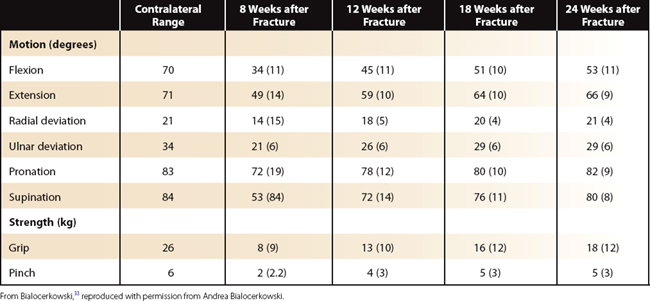
TABLE W2-16 Association between Standardized and Individualized Adelaide Questionnaire Scores and Impairment Measures, Measured by the Pearson Correlation Coefficient
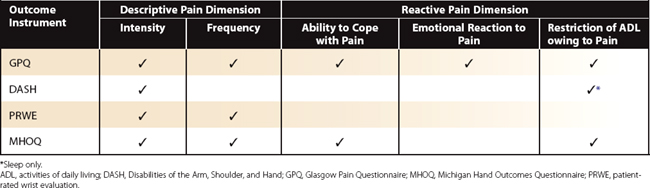
These findings have implications for the management of distal radius fracture patients. Treatment of these patients should be directed at increasing their ability to perform daily activities, rather than focusing solely on reducing impairments.44,45 Rehabilitation should consist of task-specific training, using closed chain exercises that focus on various types of grasp used during daily activities. This approach is in contrast to focusing on the reduction of impairments, by prescribing wrist movements and strengthening exercises in the cardinal planes that do not replicate the movements that are used during daily activities. Our results also suggest that even mild pain is an important contributor to poor performance of daily activities.46,47 Pain should be effectively managed during the rehabilitation period and appropriately evaluated. Pain items contained in DASH, PRWE, and MHOQ do not cover the full scope of pain, including descriptive and reactive dimensions (Table W2-17). Because pain is a complex phenomenon, we recommend a standardized pain questionnaire, such as the Glasgow Pain Questionnaire, should be used in conjunction with the Adelaide Questionnaire.36
Clinical Application of the Adelaide Questionnaire to Patients after Four-Corner Wrist Fusion
The Adelaide Questionnaire has been used in clinical practice to evaluate the functional outcome after a four-corner wrist fusion. This surgical procedure, which involves the resection of the scaphoid and fusion of the capitate, lunate, triquetrum, and hamate,48 is indicated when chronic wrist pain is associated with localized wrist disease, usually following nonunion of the scaphoid or in advanced scapholunate instability.49–51 The outcomes of four-corner wrist fusion have been systematically documented in terms of impairments.49–54 Activity limitations have been assessed in only three studies, using DASH, PRWE, or MHOQ.52–54 No information was provided regarding the specific daily activities these patients have difficulty performing or the compensatory mechanisms used to reduce activity limitations. These aspects of outcome are important for clinicians to understand because satisfaction with surgery and postoperative rehabilitation is often related to functional outcomes.
We documented these aspects of outcome in 25 adult patients with a unilateral four-corner wrist fusion using the Adelaide Questionnaire (Table W2-18).35 Patients completed the questionnaire at least 1 year postoperatively (mean 4.2 years, SD 2.7 years) when they were no longer receiving treatment. The surgery was performed by one orthopaedic surgeon, and all patients were provided with the same postoperative rehabilitation. Activity limitations and compensatory mechanism use were described using simple statistics.
TABLE W2-18 Demographic Characteristics of Patients with Four-Corner Wrist Fusion
| Characteristic | Participants |
|---|---|
| Number | 25 |
| Age, mean (SD) (yr) | 53.5 (18) |
| Gender | |
| Female | 4 (19%) |
| Male | 17 (81%) |
| Affected wrist | |
| Left | 8 (38%) |
| Right | 13 (62%) |
| Hand dominance | |
| Left | 1 (5%) |
| Right | 11 (52%) |
| Unknown | 9 (43%) |
| Time since operation (yr) | 4.2 (2.7) |
| Diagnosis | |
| Wrist instability | 12 (57%) |
| Osteoarthritis | 7 (33%) |
| Other | 2 (10%) |
Adapted from Bialocerkowski A, Bain G: Functional ability following limited wrist fusion. Proceedings of the International Federation of Societies of Hand Therapy, Sydney, March 11-15, 2007.
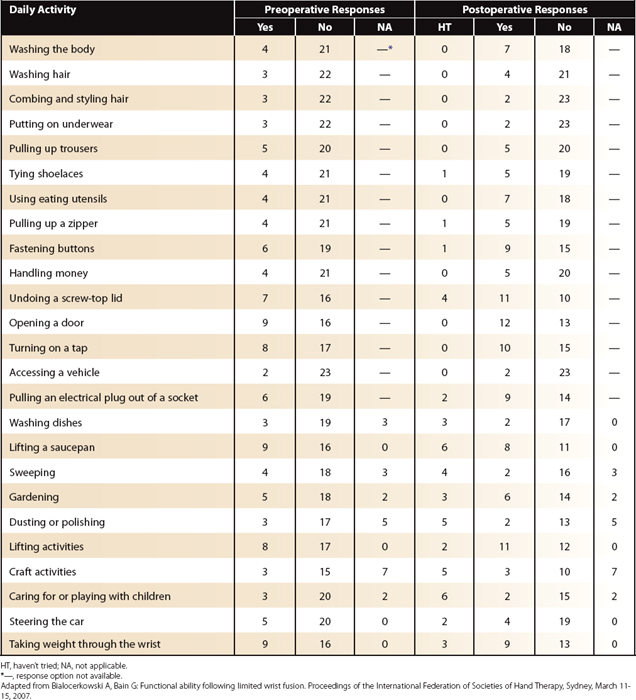
Ability to Perform Daily Activities Preoperatively
One indication for four-corner wrist fusion is chronic wrist pain that has an impact on the ability to perform daily activities. Ten of our patients reported difficulty performing daily activities contained in the standardized component of the Adelaide Questionnaire. The most frequently reported difficult daily activities were opening a door (n = 9), lifting a saucepan (n = 9), and taking weight through the wrist (n = 9) (Table W2-19).35 Given the extent of damage that necessitates the four-corner wrist fusion, these patients are likely to experience difficulty performing the same daily activities postoperatively. This likelihood is often communicated to the patient when discussing the treatment options. This information is not used to quantify outcome postoperatively, however. The Adelaide Questionnaire uses the ability to perform daily activities preoperatively as a baseline measure to quantify outcome in a more meaningful manner compared with currently used wrist outcome instruments.
Difficulty Performing Daily Activities Postoperatively
Patients often report that they experience difficulty performing daily activities after four-corner wrist fusion. This observation is supported by our data. All patients reported difficulty performing at least one daily activity in the standardized component of the Adelaide Questionnaire (average score = 6, SD = 7). The most frequently reported difficult daily activities were opening a door (n = 12), opening a screw-top lid of a jar (n = 11), and lifting activities (n = 11) (see Table W2-19).35 When postoperative status was compared with preoperative status, there was a deterioration in performing the following abilities with the operated limb: wash their body, use eating utensils, do up buttons, open a door, pull an electrical plug out of a socket, and lift.35 These results show that an appropriate baseline reference is required to determine the change in activity limitation that has occurred over the treatment period. The Adelaide Questionnaire is the only wrist outcome instrument that quantifies outcome in this manner.
Our patients also reported difficulty performing other daily activities that were not included in the standardized component of the Adelaide Questionnaire. The most frequently reported difficult daily activities were sports (n = 13), work (n = 10), and outside tasks other than gardening and sweeping (n = 9).35 These daily activities, which were important to our patients, are not addressed in currently used wrist outcome instruments. The individualized component of the Adelaide Questionnaire systematically collects activity limitation information that is unique to each patient.
Evaluation of Actual Ability
Clinicians often ask patients to list daily activities that they have not attempted to perform because of their wrist, to provide an indication of recovery. This clinical assessment often is not standardized. The Adelaide Questionnaire collects this information in a standardized manner, by the use of the “haven’t tried” response category, in the standardized component. In our patients, caring for or playing with children (n = 6) and lifting a saucepan (n = 6) were the most frequently reported activities that had not been attempted (see Table W2-19). Other activities, such as steering a car, tying shoelaces, pulling up a zipper, and fastening buttons, were not attempted by some of our patients.35 This finding is concerning, given the length of time postoperatively was on average more than 4 years. This issue would not be detected by currently used wrist outcome instruments. The Adelaide Questionnaire has the ability to identify patients at risk of poor outcome early during the rehabilitation period, by monitoring “haven’t tried” responses.
Compensatory Mechanism Use
Patients often report that they alter the way they perform daily activities to overcome any difficulties they may encounter. Of our patients, 84% reported using compensatory mechanisms to overcome specific activity limitations.35 Most commonly, patients used the other hand to perform the daily activity (42%), changed the type of grip used (42%), avoided the activity (37%), or took longer to perform the activity (37%). Patients frequently changed their grip or used a wrist brace for sporting activities, which was the most frequently specified difficult, important activity.35 Information regarding use of compensatory mechanisms is frequently gained during the patient examination, but infrequently elicited in a systematic manner. The Adelaide Questionnaire provides a standardized means of collecting this information, which is invaluable when ascertaining the extent to which the wrist is being used for daily activities.
Summary
1. Bidra R, Dias J, Heras-Palau C, et al. Assessing outcome after hand surgery: the current state. J Hand Surg [Br]. 2003;28:289-294.
2. Huijbregts M, Myers A, Kay T, et al. Systematic outcome measurement in clinical practice: challenges experienced by physiotherapists. Physiother Can. 2002;54:25-31.
3. Heras-Palou C, Burke F, Gias J, et al. Outcome measurement in hand surgery: report of a consensus conference. Br J Hand Therap. 2003;8:70-80.
4. Duckworth M. Outcome measurement selection and typology. Physiotherapy. 1999;85:21-27.
5. McCartney, Brown R. Managing by numbers: Using outcome measures in the NHS. Int J Health Care Qual Assur. 1999;12:6-12.
6. Melvin J. Outcomes research in rehabilitation: scope and challenges. Am J Phys Med Rehabil. 2001;80:78-82.
7. Marshall S, Haywood K, Fitzpatrick R. Impact of patient-reported outcome measures on routine practice: a structured review. J Eval Clin Pract. 2006;12:559-568.
8. Larson C, Lauritsen J. Epidemiology of acute wrist trauma. Int J Epidemiol. 1993;22:911-916.
9. Berger E, Berger R, Tomita K, et al: Morphology and classification of mechanoreceptors. Proceedings of the International Federation of Societies of Surgery of the Hand, Sydney, March 11-15, 2007.
10. Hagert E: Distribution of mechanoreceptors in the wrist ligaments. Proceedings of the International Federation of Societies of Surgery of the Hand, Sydney, March 11-15, 2007.
11. Berger R, Laskowski E: Changes of performance in proprioception in impaired patients. Proceedings of the International Federation of Societies of Surgery of the Hand, Sydney, March 11-15, 2007.
12. Garcia-Elias M: Proprioception in carpal instability. Proceedings of the International Federation of Societies of Surgery of the Hand, Sydney, March 11-15, 2007.
13. Bialocerkowski AE, Grimmer K, Bain G. A systematic review of the content and quality of wrist outcome instruments. Int J Qual Health Care. 2000;12:149-157.
14. Amadio P. Outcome assessment in hand surgery and hand therapy: an update. J Hand Therap. 2001;12:63-67.
15. Weiss A-P, Wiedeman G, Quenzer D, et al. Upper extremity function after wrist arthrodesis. J Hand Surg [Am]. 1995;20:813-817.
16. Wright J. Evaluating the outcome of treatment: shouldn’t we be asking patients if they are better? J Clin Epidemiol. 2000;53:549-553.
17. Chen Q, Kane R. Effects of using consumer and expert ratings of activities of daily living scale on predicted functional outcomes of post acute care. J Clin Epidemiol. 2001;54:334-342.
18. Hudak P, Amadio O, C Bombardier, Upper Extremity Collaborative Group. Development of an upper extremity outcome measures: the DASH (Disabilities of the Arm, Shoulder and Hand). Am J Ind Med. 1996;29:602-608.
19. MacDermid J. Development of a scale for patient rating of wrist pain and disability. J Hand Therap. 1996;9:178-183.
20. Chung K, Pillsbury M, Waters M, et al. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg [Am]. 1998;23:575-587.
21. Smith B, Cooney W. Revision of failed bone grafting for nonunion of the scaphoid: Treatment options and results. Clin Orthop. 1996;327:98-109.
22. Hammond R. Evaluating physiotherapy measuring outcome. Physiotherapy. 2000;86:170-172.
23. Bialocerkowski A. Difficulties associated with wrist disorders—a qualitative study. Clin Rehabil. 2002;16:429-440.
24. Bialocerkowski A, Grimmer K, Bain G. Validity of the patient-focused wrist outcome instrument: do impairments represent functional ability? Hand Clin. 2003;19:449-455.
25. Wright T, Horodyski M, Smith D. Functional outcome of unstable distal radius fractures: ORIF with a volar fixed-angle tine plate versus external fixation. J Hand Surg. 2005;30:289-299.
26. MacDermid J, Donner A, Richards R, et al. Patient versus injury factors as predictors of pain and disability six months after distal radius fracture. J Clin Epidemiol. 2002;55:849-854.
27. Kotsis S, Lau F, Chung K. Responsiveness of the Michigan Hand Outcomes Questionnaire and physical measurements in outcome studies of distal radius fracture treatment. J Hand Surg. 2007;32:84-90.
28. Young N, Williams J, Yoshida K, et al. The context of measuring disability: does it matter whether capacity or performance is measured? J Clin Epidemiol. 1996;49:1079-1101.
29. Hermann D. Reporting current past and changed health status: what we know about distortion. Med Care. 1995;33:AS89-AS94.
30. Wilson I. Clinical understanding and clinical implications of response shift. Soc Sci Med. 1999;48(11):1577-1588.
31. Beaton D, Tarasuk V, Katz J, et al. Are you better: A qualitative study of the meaning of recovery. Arthritis Care Res. 2001;45:270-279.
32. Bialocerkowski A, Grimmer K. Compensatory mechanism use during the first 6 months following distal radius fracture. Int J Therap Rehabil. 2004;11:467-474.
33. Bialocerkowski A: An instrument that assesses ADLs following a wrist disorder: development and preliminary testing. Doctoral thesis, University of South Australia, 2002.
34. Bialocerkowski A, Grimmer K, Bain G. Development of a patient-focused wrist outcome instrument. Hand Clin. 2003;19:437-448.
35. Bialocerkowski A: Activity limitations and compensatory mechanism use following limited wrist fusion. Arthritis Care Res., in press.
36. Thomas R, McEwen J, Asbury A. The Glasgow Pain Questionnaire: a new generic measure of pain: development and testing. Int J Epidemiol. 1996;25:1060-1067.
37. Adams L, Greene L, Topoozian E. Range of motion. American Society of Hand Therapists: Clinical Assessment Recommendations, 2nd ed; 1992; American Society of Hand Therapists: Chicago.
38. Fess E. Grip strength. American Society of Hand Therapists: Clinical Assessment Recommendations, 2nd ed; 1992; American Society of Hand Therapists: Chicago.
39. Macey A, Burke D. Outcomes of hand surgery. J Hand Surg [Br]. 1995;20:841-855.
40. Stone J. Sensibility. American Society of Hand Therapists: Clinical Assessment Recommendations, 2nd ed; 1992; American Society of Hand Therapists: Chicago.
41. Prince P, Kneiman M, Gulland L. Fracture prevalence in an Australian population. Aust J Public Health. 1993;17:124-128.
42. Barron J, Barrett J, Karagas M. The epidemiology of peripheral fractures. Bone. 1996;18:209S-213S.
43. MacDermid J, Richards R, Roth J. Distal radius fracture: a prospective outcome study of 275 patients. J Hand Therap. 2001;14:154-169.
44. Michlovitz S, LaStayo P, Alzner S, et al. Distal radius fractures: therapy practice patterns. J Hand Therap. 2001;14:249-257.
45. Hurov J. Fractures of the distal radius: what are the expectations of therapy? A two-year retrospective study. J Hand Therap. 1997;10:269-276.
46. Scudds R, Osbyte T. Pain and pain-related interference with function in older Canadians: the Canadian study of health and aging. Disabil Rehabil. 2001;23:654-664.
47. Williamson G, Schulz R. Pain activity restriction and symptoms of depression among community residing elderly adults. J Gerontol. 1992;47:367-372.
48. Watson H, Goodman M, Johnson T. Limited wrist arthrodesis, part 2: intercarpal and radiocarpal combinations. J Hand Surg [Am]. 1981;6:223-233.
49. Lyons R, Weiss A-P. Scaphoid excision and four-corner fusion in the SLAC/SNAG wrist. Op Tech Orthop. 2006;13:34-41.
50. Kendall C, Brown T, Millon S, et al. Results of four-corner arthrodesis using dorsal circular plate fixation. J Hand Surg [Am]. 2005;30:903-907.
51. Shin A. Four-corner arthrodesis. J Am Soc Surg Hand. 2006;1:93-111.
52. Cohen M, Kozin S. Degenerative arthritis of the wrist: proximal row carpectomy versus scaphoid excision and four corner arthrodesis. J Hand Surg [Am]. 2001;26:94-104.
53. Chung K, Watt A, Kotis S. A prospective outcomes study of four-corner wrist arthrodesis using a circular limited wrist fusion plate for stage II scapholunate advanced collapse wrist deformity. Plast Reconstr Surg. 2006;118:433-442.
54. Sauerbier M, Trankle M, Linsner G, et al. Midcarpal arthrodesis with complete scaphoid excision and interposition bone graft in the treatment of advanced carpal collapse (SNAC/SLAC wrist): operative technique and outcome assessment. J Hand Surg [Br]. 2002;25:341-345.
55. Jolles B, Buchbinder R, Beaton D. A study compared nine patient-specific indices for musculoskeletal disorders. J Clin Epidemiol. 2005;58:791-801.