Health, illness and disease3
Pathology is the study of the structural and functional changes which occur in cells and tissues as a result of injuries, abnormal stimuli or genetic abnormalities, and the consequences for the organism. It provides the link between basic biological sciences and the practice of medicine. In broad terms, the study of pathology encapsulates the way we think about diseases and about their causes, prevention and classification. Together with epidemiology (the study of disease at the level of populations), an understanding of pathology allows rational and practical classification of diseases.
• Pathology is the study of disease processes.
• Epidemiology is the study of diseases at the level of populations and provides a broad context for understanding pathology.
• Both provide a useful framework for classifying and understanding mechanisms of disease.
1.1. Health, illness and disease
Health and disease
Producing an accurate and complete definition of disease is not straightforward. Disease is often said to be a state of physiological or psychological dysfunction, or an abnormal variation in the structure or function of a part of the body. There is a wide range of normality and the human body can readily adapt to changes in the environment (e.g. by an increase in haemoglobin at an altitude where oxygen levels are low). Disease can be defined as a state in which these limits of normality are over-reached. Definitions like this one are ‘naturalistic’, and take the philosophical position that to have a disease is to fall outside the limits of normality, and that normality can be objectively defined. An alternative view is called ‘normativism’ and states that our ideas of what constitutes a disease are subjective and dependent on our personal and cultural values. For example, whether baldness is a disease depends on the cultural significance placed on hair loss. In some political contexts, political dissent has been considered a disease requiring psychiatric treatment. Whatever definition is used, the consequence of labelling someone as having a disease engages healthcare workers in a moral, ethical or professional obligation to intervene.
The World Health Organization defines health as a state of complete physical, mental and social wellbeing, and not merely the absence of disease or infirmity. Illness is the subjective state of not feeling well. Thus, it is possible to have a disease but not feel ill, because some diseases do not cause symptoms (a symptom is something noticed by the patient).
Classification of disease
Diagnosis uses concepts of disease classification to identify a disease in an individual patient (see Ch. 2). The aims of disease classification are to:
• determine the best treatment
• estimate the prognosis (expected future outcome)
• ascertain the cause, so the disease can be prevented in the future.
The most useful disease classifications are based on causes (aetiology) and underlying mechanisms (pathogenesis).
Aetiology
Diseases result from the interaction between individuals and their environment. The underlying cause is termed the aetiology. Some examples are:
• genetic: Down’s syndrome (extra chromosome 21)
• infective: bacteria, viruses, fungi
• chemical (drugs and toxins): cirrhosis of the liver caused by alcohol damage; respiratory failure as a result of paraquat poisoning affecting lungs; skin rash due to penicillin
• radiation: post-irradiation cancer (e.g. squamous cell carcinoma developing in the skin of a breast irradiated for mammary carcinoma)
• heat and cold: burns; frostbite
• metabolic: diabetes mellitus due to lack of insulin; gout due to deposition of uric acid crystals in joints
• nutritional: malnutrition; obesity; vitamin deficiency
• psychological: post-traumatic stress disorder due to witnessing a horrific event.
The causes of disease extend beyond pathological processes, however. Social and political factors may be of great importance, for example social stigmatisation of certain physical conditions, poverty, and government policy with respect to healthcare.
Idiopathic disease
In some instances, the underlying cause of a disease is obscure. Many euphemisms are used for this, including idiopathic, cryptogenic, essential and spontaneous. ‘Cause unknown’ is a simpler and more honest way of saying the same thing.
Pathogenesis (mechanisms of disease)
The pathogenesis of a disease is the mechanism by which the cause(s) interact with the target cells or tissues to produce pathological changes. There are a few fundamental processes that underlie most diseases:
• inflammation: response to injury in living vascularised tissue
• degeneration: deterioration of cell function resulting from metabolic disease or ageing
• neoplasia (oncogenesis): the process of transformation of cells from normal to the neoplastic, autonomous state in which the cells do not respond normally to factors controlling cell growth
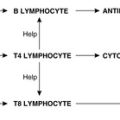
• immune reactions: specific responses to foreign organisms or material.
Genetic, acquired and congenital disease
Broadly speaking, diseases can be classified into two categories: ‘genetic’ and ‘acquired’. Genetic diseases are due to abnormalities in the genome. Most are inherited, i.e. passed from parent to offspring, but about 15–20% occur due to new mutations in the affected individual. Some, such as trisomy 21 (Down’s syndrome), are evident at birth, whereas others, such as Huntington’s disease and familial adenomatous polyposis, produce symptoms only in later life. Table 1 gives a classification of the main types of genetic disease. Acquired diseases are caused by environmental factors, such as a road traffic accident resulting in a bone fracture.
| Type | Basis | Transmission pattern | Examples |
|---|---|---|---|
| Mendelian | Expression of mutation in a single gene | Autosomal dominant | Huntington’s disease: due to an abnormality in a protein called huntingtin; affected individuals develop movement disorders and dementia in adulthood |
| Marfan’s syndrome: defective matrix protein fibrillin-1 causes abnormalities in the skeleton, cardiovascular system and eye Familial adenomatous polyposis: mutation of APC results in large numbers of neoplasms in the colon and elsewhere | |||
| Autosomal recessive | Cystic fibrosis: abnormal transmembrane ion transport resulting from a defective transmembrane conductance regulator causes thick, sticky mucous secretions | ||
| Sickle cell anaemia: a point mutation in the beta-haemoglobin chain causes deoxygenated haemoglobin molecules to undergo abnormal polymerisation | |||
| X-linked | Haemophilia A: a defect in blood clotting factor VIII causes abnormal bleeding | ||
| Duchenne’s muscular dystrophy: abnormalities in the sarcolemma-associated protein dystrophin cause progressive weakness | |||
| Multifactorial | The combined action of two or more genes with additive effects | The severity of the disease is proportional to the number of deleterious genes | Hypertension Congenital heart disease Diabetes mellitus |
| Cytogenetic | An abnormal number of chromosomes, or major structural changes in chromosomes affecting many genes | Generally arise de novo | Trisomy 21 (an extra chromosome 21) causes Down’s syndrome: characteristic facial appearances, single palmar crease, learning disabilities, increased risk of heart defects and other diseases |
| Deletion of part of the long arm of chromosome 22 causes DiGeorge syndrome: congenital heart defects, T cell immunodeficiency, parathyroid hypoplasia, facial abnormalities, psychiatric problems | |||
| Lack of an X chromosome (X0 phenotype) causes Turner’s syndrome: infertility, short stature, neck webbing, etc. |
Although the classification of disease into genetic and acquired is conceptually useful, the distinction is blurred because genetic and environmental factors interact in the pathogenesis of most diseases. For example, although carcinoma of the lung is acquired due to environmental exposure to cigarette smoke, there are genetic factors that make some individuals more prone to developing the condition than others. Likewise, there are genetic components to the development of diabetes mellitus, but the individual’s diet determines the severity of the disease. Only a few diseases can be considered entirely genetic or acquired in nature.
The term congenital is used for a disease present at birth, even though it may not be recognised or recognisable at that time. Such diseases include not only genetic abnormalities but also diseases acquired due to environmental factors acting on the developing embryo and fetus. Examples of acquired congenital diseases are:
• cerebral palsy due to fetal hypoxia during delivery
• congenital rubella due to intrauterine infection with rubella virus (German measles)
• fetal alcohol syndrome due to intrauterine exposure to large amounts of ethanol.
1.2. Ways of thinking about diseases
It is useful to have a logical framework for thinking about diseases. One way of organising the information is to use the following headings:
• definition: clinical or pathological
• epidemiology: e.g. incidence, age/gender, geography, race
• aetiology
• underlying pathology: mechanisms of disease (pathogenesis) with consequent structural changes in tissues (macroscopic – visible to the naked eye; microscopic – seen only by using the microscope) and functional changes in tissues (pathophysiology)
• clinical features: symptoms and signs; special investigations
• differential diagnosis: other diseases which may be similar
• treatment: e.g. drugs, surgery, counselling
• complications: other diseases that can follow
• prognosis: natural history of disease, disease outcome.
Epidemiology
Epidemiology provides a wider context for the study, classification and diagnosis of diseases. Data recorded about incidence, prevalence, death rate, etc. relate to populations, rather than to individuals.
Knowledge of epidemiology is important for:
• providing clues to what may cause disease
• identifying risk factors and risk markers
• planning and executing disease prevention and health promotion
• providing adequate healthcare facilities
• evaluating healthcare interventions.
Diseases are often discussed in terms of their morbidity (degree of ‘illness’ involved) and mortality (risk of death as a result of the disease). Five-year and 10-year survival rates are often used as an expression of mortality. For example, in some types of lung cancer the poor prognosis is reflected in a 5-year survival rate of 0%.
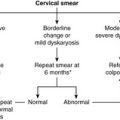
Screening is the process whereby apparently healthy people are investigated in order to detect unrecognised disease. Although ‘mass screening’ is carried out (e.g. all babies are screened for phenylketonuria at birth), most screening programmes target certain ‘at risk’ groups. Thus, the screening programmes for female breast and cervical cancer target subgroups of the population who are most at risk, namely females of certain age groups. Screening involves a relatively inexpensive diagnostic test, such as a cervical smear or mammogram, which picks up those with early, treatable forms or precursors of the disease. The test must be sensitive so it picks up as many cases as possible, but not over-sensitive so that ‘false-positive’ results occur. In a perfect test, the sensitivity (true positives) and specificity (true negatives) will each be 100%.
Incidence and prevalence
Incidence of a disease is the number of new cases occurring in a defined population over a defined time period. In contrast, prevalence is the number of cases found in a defined population at a particular time. Factors affecting incidence and prevalence include:
• time: how the disease varies over the course of time, e.g. historically or with the changing seasons
• person: the personal characteristics of those who have the disease and how they differ from those who do not, e.g. in age, sex, occupation, race, social class, behaviour.
Changes in the incidence of disease with time may result from preventive measures, such as immunisation programmes, or may reflect changes in social conditions. For example, increased smoking has led to an increase in heart disease and lung cancer, better housing conditions in the early twentieth century led to a decrease in tuberculosis. The biggest drop in the number of cases of tuberculosis antedated BCG immunisation and antibiotics, and was mainly a result of better housing and social conditions.
Many diseases show significant geographical variations: in industrialised countries heart disease and cancer are common, whereas in developing countries malnutrition and infection are often the principal health problems. Different infectious agents are common in different geographical areas.
There are many well-documented associations between occupations and disease:
• coal miners – pneumoconiosis (coal-dust disease of the lungs)
• boilermakers and dockyard workers – asbestosis (asbestos-related scarring in the lungs); mesothelioma (asbestos-related malignant tumour of the pleura)
• rubber and dye workers – bladder cancer through the effect of chemicals
• those working in hardwood manufacturing – nasal cancer as a result of inhalation of wood dust.
Relative risk is a way of describing the degree of risk for developing a disease associated with a particular occupation, behaviour or other factor. It is the proportion of individuals exposed to the risk factor who develop the disease divided by the proportion that develops it in the rest of the population. Thus, if exposure to a certain chemical has a relative risk of 2 for developing a particular cancer, it means that exposed individuals are twice as likely to develop the cancer as unexposed individuals.
Self-assessment: questions
One best answer questions
2. Which of the following is not a genetic disease?
a. Down’s syndrome
b. congenital rubella
c. familial adenomatous polyposis
d. haemophilia A
e. Huntington’s disease
3. Which of the following is not considered when classifying a disease?
a. aetiology
b. pathogenesis
c. response to treatment
d. social context
e. star sign
4. A researcher is studying a disease and finds that the relative risk of developing the disease for people who drink coffee is 0.5. Which of the following conclusions is most appropriate?
a. coffee drinkers are four times as likely to develop the disease as those who do not drink coffee
b. coffee drinkers are twice as likely to develop the disease as those who do not drink coffee
c. those who do not drink coffee are twice as likely to develop the disease as coffee drinkers
d. those who do not drink coffee are four times as likely to develop the disease as coffee drinkers
e. coffee is the most likely cause of the disease
True-false questions
1. The following are correctly paired:
a. idiopathic – cause unknown
b. pathogenesis – direct cause of disease
c. congenital – present at birth
d. prognosis – likely disease outcome
e. aetiology – mechanism of disease production
2. The following are examples of cytogenetic diseases:
a. haemophilia (factor VIII deficiency)
b. Down’s syndrome
c. sickle cell anaemia
d. Münchhausen’s syndrome
e. Turner’s syndrome
3. The following are correctly paired:
a. incidence – number of cases in a population at a given time
b. symptoms – features of an illness that the patient notices
c. prevalence – number of new cases in a population over a given time
d. morbidity – number of deaths in a population
e. sensitivity of a screening test – number of patients with the disease who have a positive screening test
Case history
A 9-year-old boy with cystic fibrosis presents to his local hospital with a chest infection. He has chest pain and is coughing up foul smelling, green sputum.
1. What is cystic fibrosis?
2. What is the pathogenesis of the child’s chest infection?
He is treated with antibiotics and makes a swift recovery.
3. What other therapy is likely to be of value in treating the chest infection?
4. What other problems might this patient develop?
5. What is the prognosis of the disease?
Short note questions
1. What factors may affect the incidence and prevalence of a disease?
2. What is meant by the term ‘screening’? What factors influence the success of a screening programme?
3. What factors influence the prognosis of a disease?
Viva questions
1. What does ‘congenital’ mean? How does this differ from the term genetic?
2. How do aetiology and pathogenesis differ?
3. What type of disease may have a high incidence but a low prevalence (and vice versa)?
Self-assessment: answers
One best answer
2. b. Congenital rubella is present at birth, but it is an infectious disease, not a genetic one. Despite the principle that virtually all diseases have genetic and environmental components to some extent, it is still useful to distinguish those in which one or the other is predominant.
3. e. This question is not as trite as it looks, because astrology is an important part of many non-Western medical traditions. However, it is not supported by scientific evidence and so the patient’s star sign is not considered in pathology or epidemiology.
4. c. Coffee seems to have a protective effect for this disease; coffee drinkers develop it only half as often as other individuals.
True-false answers
1. a. True. Idiopathic, essential and primary are all terms used to mean cause unknown.
b. False. Pathogenesis is the mechanism by which the causal agent(s) act upon the body systems to produce the disease.
c. True. The term congenital means that the pathological process has affected the embryo or fetus. It is important to remember that the congenital disease/defect may not cause illness until months or years after birth (e.g. various forms of congenital heart disease).
d. True. The prognosis of a disease is an estimate of its outcome.
e. False. The aetiology of a disease is the causal agent.
2. a. False. Haemophilia is an inherited disorder of blood clotting but it is caused by a single gene mutation. The genetic defect is linked to the X chromosome and is carried by females and mainly expressed in disease form in males. The abnormality in the gene causes a defect in factor VIII production and thus the clotting cascade is interrupted and affected individuals have a bleeding tendency.
b. True. Down’s syndrome is a common chromosomal disorder. Most affected individuals (95%) have trisomy 21, i.e. an extra chromosome 21. Their total chromosome count is therefore 47. The remaining 5% have an extra copy of the long arm of chromosome 21 translocated to another chromosome. Two other common trisomies are trisomy 18 (Edward’s syndrome) and trisomy 13 (Patau’s syndrome).
c. False. Sickle cell anaemia is caused by a point mutation in the haemoglobin gene that substitutes a valine for a glutamate in the beta-haemoglobin molecule. It is not associated with cytogenetic abnormalities.
d. False. Patients with Münchhausen’s syndrome have fictitious illnesses with frequent admissions to hospital, repeated investigations and sometimes surgery.
e. True. Girls with Turner’s syndrome typically have only one X chromosome, so the total number of chromosomes is 45. They are phenotypically female but are infertile and show some classic features such as a webbed neck and short stature.
3. a. False. Incidence is the number of new cases in a population over a given time.
b. True. Symptoms are reported by the patient. Signs are the clinical manifestations of a disease which the clinician elicits.
c. False. Prevalence is the number of cases in a population at any one time.
d. False. The term morbidity relates to illness, not death (mortality).
e. True. The sensitivity of a test is the number of individuals with the condition who test positive. In other words, it is the power of the test to correctly identify individuals who have the disease. In contrast, specificity is the ability of the test to correctly identify people who are well: it is the number of individuals free of the disease who have a negative result.
Case history answer
1. Cystic fibrosis is characterised by the production of abnormally sticky mucous secretions by exocrine glands. This causes blockage of the ducts in organs such as the pancreas, lung and reproductive tissues, leading to failure of function. Susceptibility to lung infections is a particular problem. The diagnosis can be made by the finding of raised concentrations of chloride and sodium in sweat. Cystic fibrosis is an autosomal recessive disease. The CF gene is located on the long arm of chromosome 7 and codes for a chloride ion-linked transmembrane regulator protein. Many different mutations of the CF gene have been described. The prevalence of carriage of the abnormal gene is very high (of the order of 1:25 Caucasians).
2. This case illustrates the relationship between pathogenesis and aetiology. The sputum is characteristic of bacterial infection; common organisms isolated from patients with cystic fibrosis include Staphylococcus aureus, Haemophilus influenzae and Pseudomonas aeruginosa. The pathogenesis involves the following processes:
b. these sticky secretions can then be colonised by bacteria, some of which will be pathogenic (disease causing)
c. multiplication of the pathogenic bacteria incites an inflammatory reaction
d. the large numbers of neutrophils that form part of the inflammatory reaction produce pus, hence the characteristics of the sputum.
3. In addition to antibiotic treatment, physiotherapy is indicated to help drain the secretions.
4. Patients with cystic fibrosis have numerous systemic problems. Recurrent lung infections could be associated with the development of bronchiectasis. Cor pulmonale can complicate the lung disease in cystic fibrosis. Failure of pancreatic function is common, and this patient is likely to require enzyme supplements. A few patients also require replacement insulin treatment. Liver failure may occur due to inspissated secretions obstructing the biliary tree. Most males exhibit congenital absence of the vas deferens bilaterally and are infertile.
5. Although the prognosis of cystic fibrosis is improving with better therapeutic regimens, and it may ultimately be cured by gene therapy, the disease still causes premature death; very few patients with cystic fibrosis survive beyond the age of 40.
Short note answers
Comment: For all the three questions, start with a definition of the term. Use bulleted lists as appropriate.
1. The main points to be covered in this answer are:
a. definitions of incidence and prevalence
b. general factors affecting them: time, place, person
c. examples of each factor.
2. The main points to be covered in this answer are:
a. definition of screening (this answers the first part of the question)
b. the relationship between the natural history of a disease and the target population
c. the acceptability of the screening method
d. sensitivity and specificity in relation to false-negative and false-positive results
e. cost.
Illustrate your answer with examples, e.g. the cervical and breast screening programmes.
3. The prognosis of a disease will vary for each patient and depends on:
a. the nature of the disease
b. how long the patient has had the disease
c. the general state of health of the patient: the presence of other diseases, and the nutritional status of the patient
d. the age of the patient
e. availability of diagnostic and treatment facilities
f. the response of the patient to the treatment available.
There are many examples of changing prognosis related to factors of an individual patient’s status, e.g. Candida infection in a healthy individual is a minor illness, whereas in a person with human immunodeficiency virus (HIV) infection it may be fatal; influenza in a healthy 20-year-old is usually a self-limiting illness, whereas in an elderly bedridden patient it may be complicated by pneumonia and lead to death.
Viva answers
Comment: It is a good idea to start off with a definition of the subject or topic and then give examples in the same way as for a short answer question. However, the examiners may ask questions which may deflect you from a logical sequence, because they will be looking for depth and breadth of knowledge. You will have to keep prioritising and reorganising your knowledge as you go along.
1. Congenital disease is present at birth, but not necessarily inherited. Genetic disease is present in the genome of the individual from conception but will not necessarily manifest at birth. For example, fetal alcohol syndrome and haemophilia are both congenital, but only haemophilia is a genetic disorder.
2. Aetiology is the cause of a disease whereas pathogenesis is the underlying abnormal process that gives rise to the disorder. For example, in the disease tuberculosis:
• The organism Mycobacterium tuberculosis is the aetiology.
• The pathogenesis is delayed hypersensitivity response of T cells and macrophages to the organism, giving rise to the destructive granulomas that characterise tuberculosis (see Ch. 9).
3. Incidence is the number of cases occurring in a defined population over a stated period of time whereas prevalence is the number of cases in a defined population at a given time. The common cold has a high incidence, because many new cases occur during the course of, say, a year. However, it is a short-lived condition and so the prevalence at any particular time is relatively low compared with the incidence. On the other hand, the incidence of new cases of cystic fibrosis in any particular year is relatively low, but because patients usually live for many years the prevalence in the population will be higher.