Chapter 343 Pancreatitis
343.1 Acute Pancreatitis
Acute pancreatitis, the most common pancreatic disorder in children, is increasing in incidence. At least 30-50 cases are now seen in major pediatric centers per year. In children, blunt abdominal injuries, multisystem disease, biliary stones or microlithiasis (sludging), and drug toxicity are the most common etiologies. Although many drugs and toxins can induce acute pancreatitis in susceptible persons, in children, valproic acid, L-asparaginase, 6-mercaptopurine, and azathioprine are the most common causes of drug-induced pancreatitis. Other cases follow organ transplantation or are due to infections, metabolic disorders, and mutations in susceptibility genes (Chapter 343.2). Less than 5% of cases are idiopathic (Table 343-1).
Table 343-1 ETIOLOGY OF ACUTE PANCREATITIS IN CHILDREN
DRUGS AND TOXINS
GENETIC
INFECTIOUS
OBSTRUCTIVE
SYSTEMIC DISEASE
TRAUMATIC
Diagnosis
Acute pancreatitis is usually diagnosed by measurement of serum lipase and amylase activities. Serum lipase is now considered the test of choice for acute pancreatitis as it is more specific than amylase for acute inflammatory pancreatic disease and should be determined when pancreatitis is suspected. The serum lipase rises by 4-8 hr, peaks at 24-48 hr, and remains elevated 8-14 days longer than serum amylase. Serum lipase can be elevated in nonpancreatic diseases. The serum amylase level is typically elevated for up to 4 days. A variety of other conditions can also cause hyperamylasemia without pancreatitis (Table 343-2). Elevation of salivary amylase can mislead the clinician to diagnose pancreatitis in a child with abdominal pain. The laboratory can separate amylase isoenzymes into pancreatic and salivary fractions. Initially, serum amylase levels are normal in 10-15% of patients.
Table 343-2 DIFFERENTIAL DIAGNOSIS OF HYPERAMYLASEMIA
PANCREATIC PATHOLOGY
SALIVARY GLAND PATHOLOGY
INTRA-ABDOMINAL PATHOLOGY
SYSTEMIC DISEASES
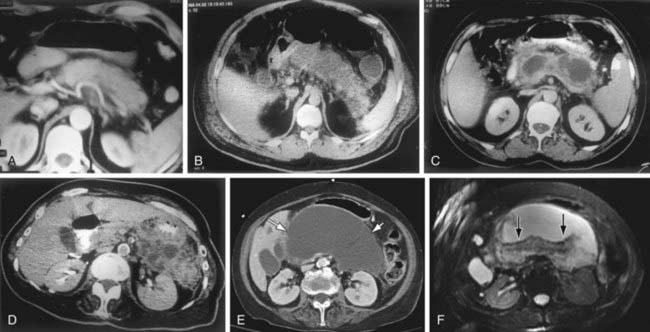
CT scanning has a major role in the diagnosis and follow-up of children with pancreatitis. Findings can include pancreatic enlargement, a hypoechoic, sonolucent edematous pancreas, pancreatic masses, fluid collections, and abscesses (Fig. 343-1); ≥20% of children with acute pancreatitis initially have normal imaging studies. In adults, CT findings are the basis of a widely accepted prognostic system. Ultrasonography is more sensitive than CT scanning for the diagnosis of biliary stones. Magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiopancreatography (ERCP) are essential in the investgation of recurrent pancreatitis, nonresolving pancreatitis, and disease associated with gallbladder pathology. Endoscopic ultrasonography also helps visualize the pancreaticobiliary system.
Frossard JL, Steer ML, Pastor CM. Acute pancreatitis. Lancet. 2008;371:143-152.
Jacobson B, Vander Vliet M, Hughes M, et al. A prospective, randomized trial of clear liquids versus low-fat solid diet as the initial meal in mild acute pancreatitis. Clin Gastroenterol Hepatol. 2007;5:946-951.
Kandula L, Lowe ME. Etiology and outcome of acute pancreatitis in infants and toddlers. J Pediatr. 2008;152:106-110.
Makola D, Krenitsky J, Parrish C, et al. Efficacy of enteral nutrition for the treatment of pancreatitis using standard enteral formula. Am J Gastroenterol. 2006;101:2347-2355.
Nydegger A, Heine R, Ranuh R. Changing incidence of acute pancreatitis: 10-year experience at the Royal Children’s Hospital, Melbourne. J Gastroenterol Hepatol. 2007;22:1313-1316.
Petrov MS, van Santvoort HC, Besselink MGH, et al. Enteral nutrition and the risk of mortality and infectious complications in patients with severe acute pancreatitis. Arch Surg. 2008;143:1111-1117.
Werlin SL, Kugathasan S, Frautschy B. Pancreatitis in children. J Pediatr Gastroenterol Nutr. 2003;37:591-595.
Whitcomb DC. Acute pancreatitis. N Engl J Med. 2006;354:2142-2150.
343.2 Chronic Pancreatitis
Chronic pancreatitis in children is often due to genetic mutations or due to congenital anomalies of the pancreatic or biliary ductal system. Mutations in the PRSS1 gene (cationic trypsinogen) located on the long arm of chromosome 7, SPINK 1 gene (pancreatic trypsin inhibitor) located on chromosome 5, in the cystic fibrosis gene (CFTR), and chymotrypsin C all lead to chronic pancreatitis (see Table 343-1).
Cationic trypsinogen has a trypsin-sensitive cleavage site. Loss of this cleavage site in the abnormal protein permits uncontrolled activation of trypsinogen to trypsin, which leads to autodigestion of the pancreas. Mutations in PRSS1 act in an autosomal dominant fashion with incomplete penetrance and variable expressivity. Symptoms often begin in the 1st decade but are usually mild at the onset. Although spontaneous recovery from each attack occurs in 4-7 days, episodes become progressively severe. Clinically, hereditary pancreatitis may be diagnosed by the presence of the disease in successive generations of a family. An evaluation during symptom-free intervals may be unrewarding until calcifications, pseudocysts, or pancreatic exocrine and endocrine insufficiency develops (Fig. 343-2). Chronic pancreatitis is a risk factor for future development of pancreatic cancer. Multiple mutations of the PRSS1 gene associated with hereditary pancreatitis have been described.
De Boeck K, Weren M, Poresmans M, et al. Pancreatitis among patients with cystic fibrosis: correlation with pancreatic status and genotype. Pediatrics. 2005;115:463-469.
Dua K, Miranda A, Santharam R, et al. ERCP in the evaluation of abdominal pain in children. Gastrointest Endosc. 2008;68:1081-1085.
Kingsnorth A, O’Reilly D. Acute pancreatitis. BMJ. 2006;332:1072-1076.
Tipnis N, Dua K, Werlin S. A retrospective assessment of magnetic resonance cholangiopancreatography in children. J Pediatr Gastroenterol. 2008;46:59-64.
Werlin SL, Taylor A. ERCP. In: Howard ER, Stringer MD, Colombani PM, editors. Surgery of the liver, bile ducts and pancreas in children. ed 2. London: STM Publishing; 2002:509-520.
Witt H, Apte M, Keim V, et al. Chronic pancreatitis: challenges and advances in pathogenesis, genetics, diagnosis, and therapy. Gastroenterology. 2007;132:1557-1573.