Chapter 11 Paediatric Proximal Radial Fractures
Introduction
Since radial head fractures are very rare in children1 this chapter will concentrate on paediatric fractures of the radial neck and their management.
Radial neck fractures account for 1% of all fractures and 5–14% of elbow fractures. They involve all age groups from childhood to prepuberty, with a peak incidence at around 9–10 years of age. They occur at a younger age in girls than in boys (approximately 2 years earlier).2
Most often the injury is a Salter–Harris type II, or complete fracture of the neck itself. Some of these fractures are very difficult to treat, with many possible complications, all of which have a significant, deleterious effect on joint function. The degree of initial anatomical disruption, especially if associated with a vascular lesion, has a major effect on outcome. However, the inadequacies of difficult primary treatment are equally responsible. Open reduction with a condyloradial Steinmann pin is usually associated with a high incidence of complications and, whenever possible, closed treatments are preferred by most paediatric orthopaedic surgeons. To avoid open reduction, two closed methods are helpful and will be described: intramedullary pinning as proposed by JP Métaizeau et al,3–8 and percutaneous pinning.9–11 In our experience, open reduction only becomes necessary when the above methods cannot obtain reduction. Even in these circumstances, osteosynthesis may require intramedullary pinning.
Aetiology
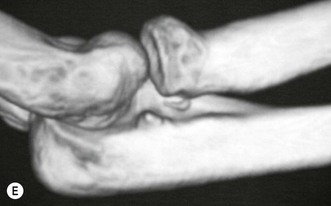
The mechanism of injury is usually an indirect force. It results from a fall onto the outstretched hand in which the elbow is extended or slightly flexed and a valgus force is applied to the elbow joint. According to the Jeffery classification, which is based on the mechanism of injury, it is a type I injury.12 The head of the radius is driven against the capitulum. As the radial head is essentially cartilaginous, it is more resistant to trauma, which is why isolated radial head fractures and epiphyseal separations are so rare. Typically, the proximal radial metaphysis cannot withstand the sudden axial compression forces to which it is subjected, and breaks. Radial neck fractures may also occur in association with dislocation of the elbow: Jeffery type II injury.13 If this occurs during a posterior dislocation of the elbow the radial head remains in an anterior position.14 If, however, it occurs during reduction of the dislocation the radial head will remain posteriorly dislocated (posterior to the capitulum). This form of fracture adversely affects the prognosis because there is an associated vascular risk and because reduction of the fracture is significantly more challenging.
Associated injuries are frequent, from fracture of the olecranon that occurs in an extended elbow, to dislocation of the elbow joint with or without avulsion of the medial epicondyle in an elbow that is slightly flexed on impact.15,16 Skin lesions and neurovascular injuries are, however, rare.
Presentation, investigation and treatment options
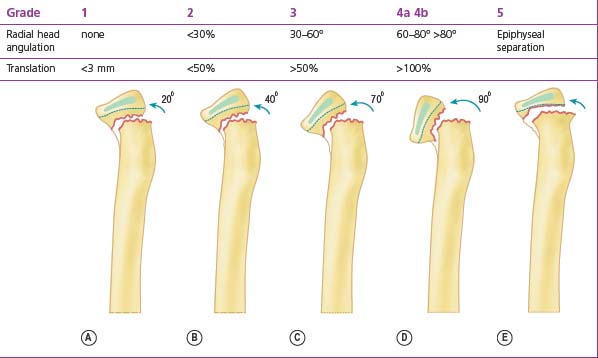
The child usually presents having fallen onto the outstretched hand. The injury most frequently occurs during sport, play or after a simple fall. Clinical examination reveals a swollen elbow that must be carefully evaluated. In addition to assessing the bony anatomy of the joint it is also essential to examine the neurovascular status of the forearm and hand. Anteroposterior (AP) and lateral radiographs of the elbow should routinely be undertaken, the fracture configuration studied and displacement of the radial head measured. Accurate classification of the injury enables appropriate treatment to be instituted. Although many radial neck fracture classifications have been developed,1,12,17 that described by Métaizeau et al4 is perhaps the most useful. This classifies radial neck fractures based on translation and is useful because of its influence on prognosis (Table 11.1):4
In 30–50% of severe displaced radial neck fractures another fracture of the elbow joint will have occurred. Most often there is a fracture of the olecranon, lateral condyle, medial epicondyle or ulna, all of which may require an additional procedure with appropriate osteosynthesis.16
Surgical techniques and rehabilitation
Conservative treatment
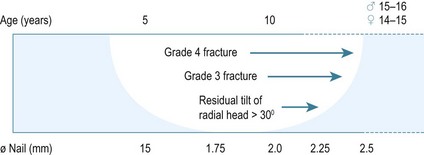
A question that is frequently asked is: allowing for the remodelling capacity of the proximal radial epiphysis, what amount of residual tilting can be accepted in order to permit good results? According to the literature, a residual displacement of 30°, and sometimes 50°,18 is well tolerated and can correct itself spontaneously. This value must be correlated to the age of the child, since a minimum of 3–4 years of growth is required to achieve adequate remodelling. A tilt of 30° is therefore often acceptable in children.
Surgical treatment
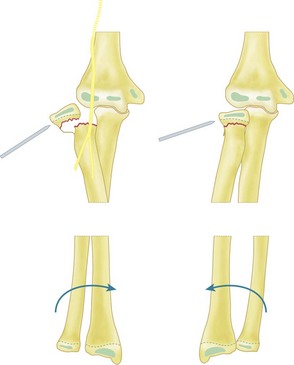
Percutaneous pinning
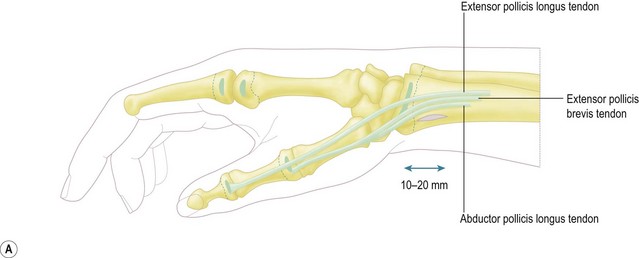
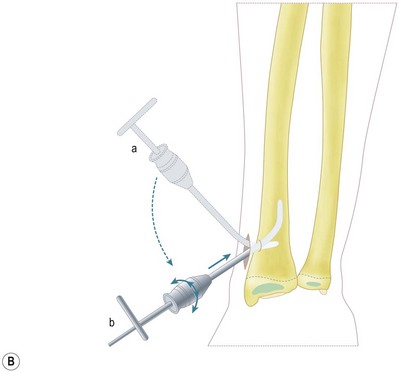
A small stab wound is made on the lateral side of the elbow, 2–5 cm below the level of the radial fracture, depending on the amount of displacement. The more displaced the fracture, the lower the entrance of the wire. This approach must be posterior to the extensor radial muscles and with the forearm in pronation so that the deep branch of the radial nerve is protected by being displaced anteriorly. A smooth 2 or 2.5 mm K-wire is inserted through the wound, the subcutaneous tissues and the muscles to reach the radial head and neck (Fig. 11.1).
Although Lenggenhager originally left the pin in place in the cast, it is nowadays considered unnecessary as sufficient stability can be obtained with a long-arm cast with the elbow flexed at 90° and the forearm in neutral rotation for 3–6 weeks.19 The period of immobilization is determined by the age of the child and is shorter for younger children, whose fractures heal more rapidly.9
Elastic stable intramedullary nailing (ESIN) technique
Published by Métaizeau et al in 1980,3 this method is very simple but requires perfect knowledge of the elastic stable intramedullary nailing technique, which is used in fractures of the forearm.20
Closed reduction
An alternative reduction manoeuvre involves replacing the thumb with a punch as described above.
Surgical procedure: retrograde radial intramedullary nailing
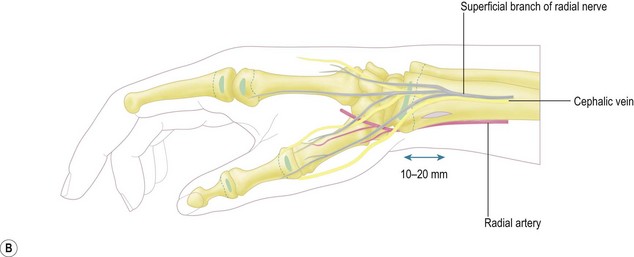
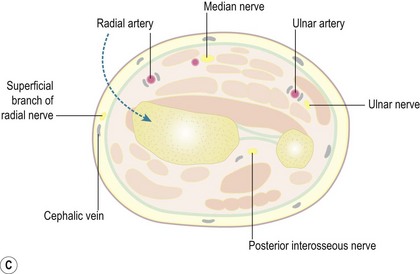
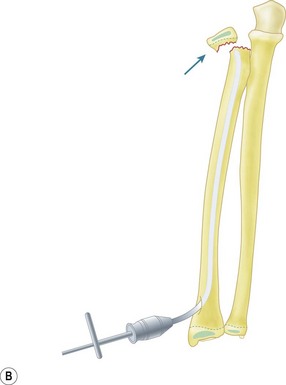
Identification of the distal physis with fluoroscopy assists in accurately positioning the 1.5–2 cm longitudinal incision. Blunt dissection using scissors is then performed. The radial vein and the sensory branch of the radial nerve are successively retracted posteriorly and protected with a mini retractor. Dissection continues anterior to the insertion of the brachioradialis tendon to avoid potential damage to the extensor pollicis brevis and abductor pollicis longus tendons, and is carried down to the bone (Fig. 11.2).
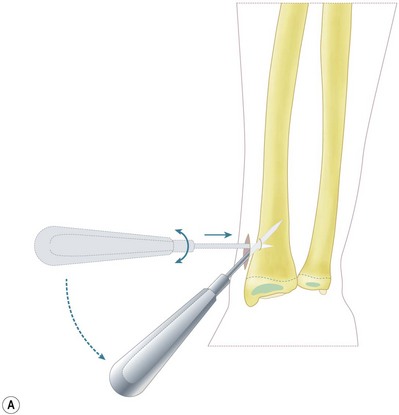
The entry hole is made with an awl in the same anterior–posterior oblique direction, 10–15 mm above the distal physis. Care should be taken not to slip anteriorly to avoid injury to the radial artery. The chief advantage of this anterolateral approach to the distal radius is safety, since there are no critical superficial neurovascular structures in the vicinity. Furthermore, if the metaphysis is firmly held in mid pronation with the thumb and index finger, the awl can be safely directed posteriorly away from the radial artery (Fig. 11.3).
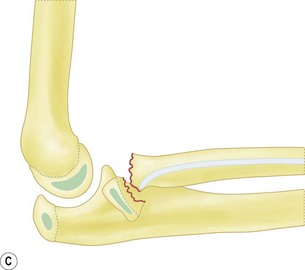
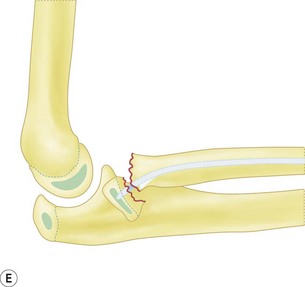
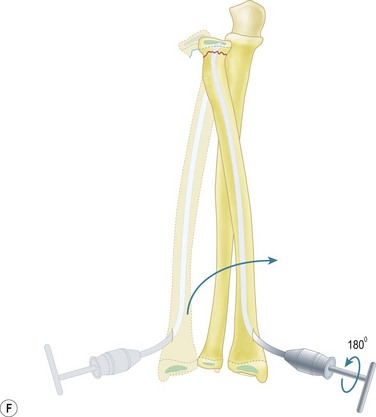
Once the nail has reached the fracture site, it must be rotated so that its tip is positioned in the plane of maximal displacement of the radial head. The nail is firmly impacted into the radial head under fluoroscopic guidance using heavy mallet blows. Reduction of translation and tilt is then obtained by rotating the nail 180° anteriorly. The direction of rotation clearly depends on the position of the radial head but, as the radial head is most often translated posterolaterally, rotation is performed in an anteromedial direction. Therefore, with the surgeon facing the distal end of the radius, rotational movement will be clockwise in a right elbow and counterclockwise in a left elbow. Gentle rotation is mandatory, otherwise the tip of the nail may cut out into the epiphysis. It is also recommended to combine rotation of the nail and pronation of the forearm. In fractures with grade 4 displacement, it may be necessary to use a punch as previously described to gently move the radial head towards the nail until it is positioned right in front of the nail tip (Fig. 11.4).
Owing to the remodelling capacity of the radial neck and depending on the child’s age at the time of surgery, under-reduction (lateral tilt) of up to 20° and even 30° is acceptable.18 For this reason one should not try at all costs to achieve a perfect reduction at the risk of damaging the lateral periosteum or making multiple perforations in the radial head.
Difficult injuries
Grade 4 radial neck fractures
These fractures cannot initially be managed with ESIN as the severe radial head tilt precludes impaction of the nail. The first technical option is to use a punch to partially reduce the radial head and allow insertion of the nail.10
A third option consists of inserting a provisional nail to both partially reduce and stabilize the fracture. Then, a second nail is inserted in the same way, which anchors in the partially reduced epiphysis. The provisional nail can then be removed and reduction is completed using the second nail. The main drawback of this method is the creation of two distal holes, and its major limitation is the small diameter of the intramedullary canal, which may not accommodate both nails.3
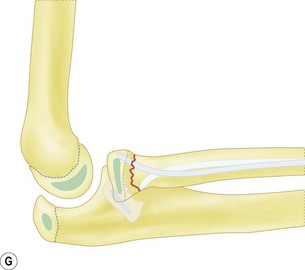
Radial head dislocation
Dislocation of the radial head posterior to the capitulum may be a contraindication to percutaneous reduction because of the risk of 180° rotation of the radial head, which would result in avulsion of the periosteal flap (if present) and, as a consequence, to necrosis of the epiphysis. Nevertheless, a subluxation manoeuvre of the joint may help the reduction with a K-wire.21 When an open approach is required, a posterolateral approach is used between the extensor carpi radialis anteriorly, and the extensor digitorum posteriorly. A technical trick from JD Métaizeau’s personal experience involves using a lateral approach through a superolateral arthrotomy that will afford access to the radial head from above and will reduce the potential risk of injury to an already compromised periosteal flap. Caution must be exercised when mobilizing the radial head, in order to preserve integrity of the few blood vessels that remain. Once reduction has been achieved, stabilization is provided by intramedullary pinning as previously described, or sometimes sutures are placed through capsuloperiosteal tissue.
Postoperative care
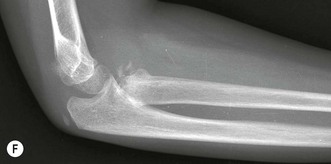
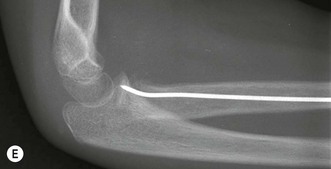
Postoperative X-rays (AP and lateral) are taken with the cast in situ.
Analgesics and nonsteroidal anti-inflammatory drugs are prescribed for a few days.
Return to sports is allowed as soon as skin healing is complete.
However, if after 2–3 years follow-up the morphology of the child’s elbow is normal, with full range of motion, longer follow-up is unnecessary (Table 11.2).
Table 11.2 ESIN and radial neck fracture: postoperative management in the absence of complications
| Day 0 |
Outcome
With the percutaneous technique, Kohler et al10 used a Rocher punch in a ‘tyre lever manoeuvre’ in 19 patients and had 18 satisfactory reductions. His results in 15 patients were nine excellent, three good and three poor with, among these, one case of partial necrosis of the radial head.
Bernstein et al9 used percutaneous pinning for fracture reduction and had success in 15 out of 18 patients. The three patients in whom this method failed comprised two who had comminuted radial head and neck fractures and one with a completely rotated and displaced radial head.
Rodriguez-Merchan11 obtained successful reduction in 20 patients with 70% good, 15% fair and 15% poor results.
Métaizeau et al published their experience of the ESIN method in 47 patients.4 Twenty patients’ radial neck fractures were grade 3, 11 grade 4a and 16 grade 4b. The reduction quality was excellent in 16 grade 3, eight grade 4a and nine grade 4b. In this latter group, three patients underwent reduction with percutaneous pinning. All these cases had excellent results with no loss of motion and no radiological change of the radial head. Residual tilt of the radial head after reduction was measured at less than 20° in three grade 3, two grade 4a and one grade 4b. Their functional results were also excellent. One grade 3 had an overcorrection of 25° with progressive remodelling and excellent function. One grade 4a had residual displacement of more then 20° and a loss of motion of more than 20°. Six grade 4b had loss of motion with five poor results. Four of these had open reduction and suffered complications of non-union of the neck (one case), necroses of the radial head (two cases) and articular calcifications (two cases). Other authors have had similar results. Gonzalez-Herranz et al5 reported 16 excellent results in 17 cases. In three cases, an overgrowth of the radial head was observed without any functional impairment. Tollet et al22 reported 15 cases with a mean age of 9 years, all of whom had full functional recovery at 6 weeks without any complications. Marchiodi et al23 described 12 cases with excellent results. Keller et al24 reported this method in the treatment of six adult patients with displaced fractures of the radial neck. All patients had good results 9 months after intramedullary reduction and stabilization. They had little or no pain, complete healing and no significant periarticular calcifications. Ursei et al8 and Nawabi et al6 reported comparable favourable results.
Complications
Complications associated with radial neck fractures
Malunion
The potential for bone remodelling depends on the child’s age. It is generally held that where residual tilt is greater than 30° there is incomplete bone remodelling.14 Treatment will vary according to the degree of discomfort.
Nonunion of the radial neck
Nonunion of the radial neck is a rarely reported complication.25 Its mechanism is very similar to that of necrosis. A major factor is the precarious vascularization that is compromised in severely displaced fractures, posterior dislocation and if open reduction of the fracture is required. At issue is the question of whether this condition should be treated or not, since it is generally well tolerated and potential complications are not insignificant.
Conclusion
Fractures of the radial neck in children must be treated conservatively whenever possible. Allowing for remodelling with growth, conservative treatment is the method of choice in grade l and 2 cases, and some grade 3 fractures with a residual tilt of <30°.18
In other cases with a displaced radial head, a perfect reduction may be obtained with percutaneous pinning or intramedullary nailing.26 An analysis of the literature indicates that the best long-term results are achieved with intramedullary nailing, in comparison to percutaneous pinning. The main difference in the two techniques is the quality of stability, which is excellent with intramedullary nailing, when compared to the cast used in the percutaneous pinning method. For these reasons, treatment of displaced fractures will give better results with intramedullary nailing, combined in some difficult reductions with percutaneous pinning.
1 Malmvik J, Herbertsson P, Josefsson PO, et al. Fracture of the radial head and neck of Mason types II and III during growth: a 14–25 year follow-up. J Pediatr Orthop B. 2003;12:63-68.
2 Chambers HG, Wilkins KE. Fractures of the proximal radius and ulna. 4th ed. Rockwood CA, Wilkins KE, King RE, editors. Fractures in children. vol. 3. Philadelphia PA: Lippincott Raven; 1996:586-613.
3 Métaizeau JP, Prévot J, Schmitt M. Reduction et fixation des fractures et décollements épiphysaires de la tête radiale par broche centromedullaire. Rev Chir Orthop. 1980;66:47-49.
4 Métaizeau JP, Lascombes P, Lemelle JL, et al. Reduction and fixation of displaced neck fractures by closed intramedullary pinning. J Pediatr Orthop. 1993;13:355-360.
5 Gonzalez-Herranz A, Alvarez-Romera A, Burgos J, et al. Displaced radial neck fractures in children treated by closed intramedullary pinning (Métaizeau technique). J Pediatr Orthop. 1997;17:325-331.
6 Nawabi DH, Kang N, Amin A, et al. Centromedullary pinning of radial neck fractures: length matters!. J Pediatr Orthop. 2006;26:278-279.
7 Schmittenbecher P, Haevernick B, Herold A, et al. Treatment decision, method of osteosynthesis, and outcome in radial neck fractures in children: a multicenter study. J Pediatr Orthop. 2005;25:45-50.
8 Ursei M, Sales de Gauzy J, Knorr J, et al. Surgical treatment of radial neck fractures in children by intramedullary pinning. Acta Orthop Belg. 2006;72:131-137.
9 Bernstein SM, McKeever P, Bernstein L. Percutaneous reduction of displaced radial neck fractures in children. J Pediatr Orthop. 1993;13:85-88.
10 Kohler R, James J, Brigound T, et al. Traitement des fractures du radius chez l’enfant par poinçonnage percutané (19 cas). Rev Chir Orthop. 1991;77:140.
11 Rodriguez-Merchan EC. Percutaneous reduction of displaced radial neck fractures in children. J Trauma. 1994;37:812-844.
12 Jeffery CC. Fractures of the head of the radius in children. J Bone Joint Surg. 1950;32B:314-324.
13 Chotel F, Vallese P, Parot R, et al. Complete dislocation of the radial head following fracture of the radial neck in children: the Jeffery type II lesion. J Pediatr Orthop B. 2004;13:268-274.
14 Newman JH. Displaced radial neck fractures in children. Injury. 1977;9:114-121.
15 Dormans JP, Rang M. Fractures of the olecranon and radial neck in children. Orthop Clin North Am. 1990;21:257-268.
16 Sessa S, Lascombes P, Prévot J, et al. Fractures of the radial head and associated elbow injuries in children. J Pediatr Orthop B. 1996;5:200-209.
17 Judet J, Judet R, Lefranc J. Fractures du col radial chez l’enfant. Ann Chir. 1962;16:1377-1385.
18 Vocke AK, VonLaer L. Displaced fractures of the radial neck in children: long-term results and prognosis of conservative treatment. J Pediatr Orthop. 1998;7:217-222.
19 Lenggenhager K. Beitrag zur behandlung der Radius-Kopfchen-Stauchungsfraktur. Schweiz Med Wochenschr. 1948;78:195-196.
20 Lascombes P, Prévot J, Ligier N, et al. Elastic stable intramedullary nailing in forearm shaft fractures in children: 85 cases. J Pediatr Orthop. 1990;10:167-171.
21 Chotel F, Sailhan F, Martin JN, et al. A specific closed percutaneous technique for reduction of Jeffery type II lesion. J Pediatr Orthop B. 2006;15:376-378.
22 Tollet P, Toussaint D, Djemal C, et al. Traitement chirurgical des fractures du col radial chez l’enfant parla technique de Métaizeau. Acta Orthop Belg. 1997;63:245-250.
23 Marchiodi L, Mignani G, Stilli S, et al. Retrograde intramedullary osteosynthesis in the surgical treatment of fractures of the radial capitellum during childhood. Chir Organ Mov. 1997;82:327-334.
24 Keller HW, Rehm KE, Helling J. Intramedullary reduction and stabilisation of adult radial neck fractures. J Bone joint Surg. 1994;76B:406-408.
25 Waters PM, Stewart SL. Radial neck fracture nonunion in children. J Pediatr Orthop. 2001;21:570-576.
26 Lascombes P. Flexible intramedullary nailing. Berlin: Nancy School University. Springer; 2010.