Chapter 18 Pacemakers and Defibrillators
1 What are the general principles of cardiovascular implantable electronic device (CIED) management according to the Heart Rhythm Society (HRS)–American Society of Anesthesiologists Consensus Statement published in 2011?
2 How can one differentiate a pacemaker from an ICD?
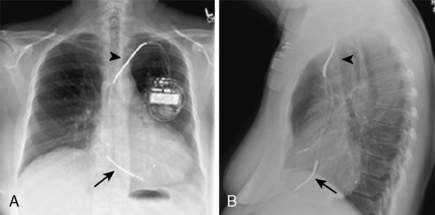
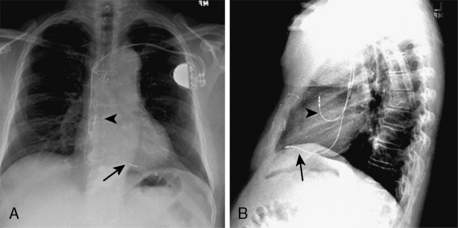
Occasionally a patient is seen initially without information about his or her CIED. A critical step is to determine whether the device is a pacemaker or an ICD. The patient may be able to tell you why the device was inserted, and this might provide a clue. However, if the patient’s history cannot help, the patient’s chest radiograph can. The ICD leads, unlike pacer leads, have one or two radiodense shocking coils. Because of the shocking coils, the ICD leads (Fig. 18-1) are much larger than the pacer leads (Fig. 18-2), and this can be appreciated radiographically.
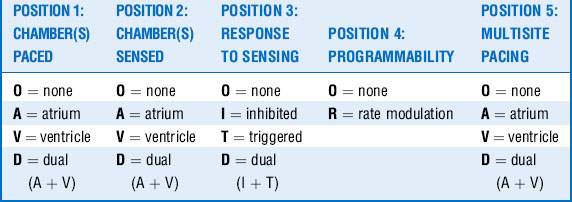
3 Describe the five-letter pacemaker code
• First position of the code reflects the chamber(s) in which stimulation occurs.
5 Explain the following pacemaker codes: DOO, VVI, DDD, and DDDRV
 DOO = asynchronous atrial-ventricular pacing with a constant A-V interval. Atrial and ventricular pacing pulses are emitted regardless of the underlying cardiac rhythm.
DOO = asynchronous atrial-ventricular pacing with a constant A-V interval. Atrial and ventricular pacing pulses are emitted regardless of the underlying cardiac rhythm.
 VVI = ventricular-only antibradycardia pacing. Failure of the ventricle to produce an intrinsic event within the appropriate time window results in ventricular pacing. With no atrial sensing, there can be no atrioventricular (AV) synchrony in a patient with any intrinsic atrial activity.
VVI = ventricular-only antibradycardia pacing. Failure of the ventricle to produce an intrinsic event within the appropriate time window results in ventricular pacing. With no atrial sensing, there can be no atrioventricular (AV) synchrony in a patient with any intrinsic atrial activity.
 DDD = dual-chamber antibradycardia pacing. In the absence of intrinsic activity in the atrium, it will be paced. After any sensed or paced atrial event, an intrinsic ventricular event must occur before the expiration of the AV timer or the ventricle will be paced.
DDD = dual-chamber antibradycardia pacing. In the absence of intrinsic activity in the atrium, it will be paced. After any sensed or paced atrial event, an intrinsic ventricular event must occur before the expiration of the AV timer or the ventricle will be paced.
 DDDRV = dual-chamber antibradycardia pacing with rate response mode circuitry (to increase the paced rate in setting of increased metabolic demand) and biventricular pacing capability.
DDDRV = dual-chamber antibradycardia pacing with rate response mode circuitry (to increase the paced rate in setting of increased metabolic demand) and biventricular pacing capability.
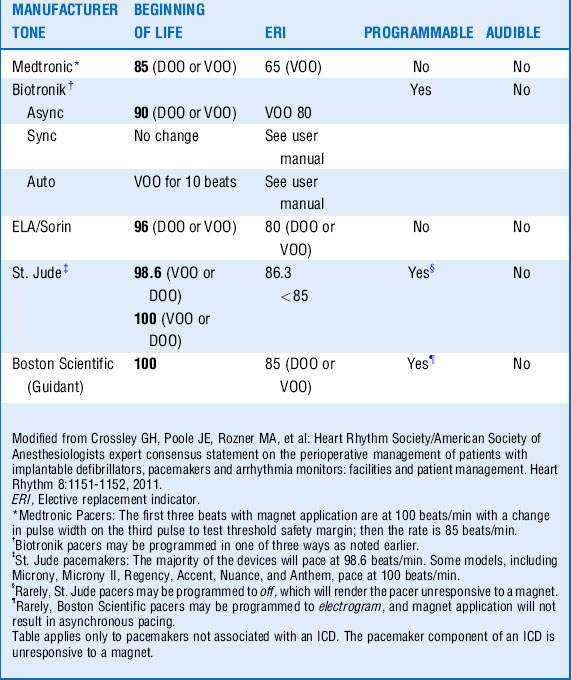
15 How will a magnet affect an ICD?
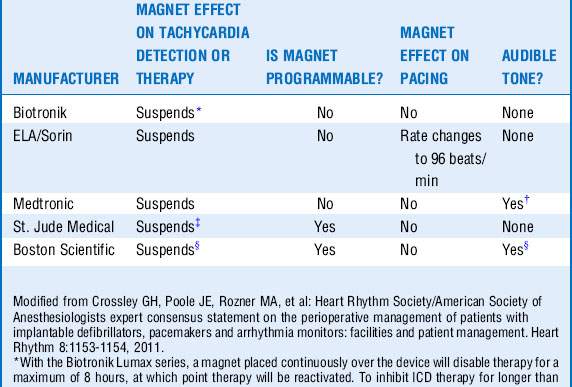
Magnets usually inhibit the antitachycardic functions (defibrillation, cardioversion, antitachy pacing) of an ICD. Because each manufacturer’s device has some idiosyncrasies, the clinician must be sure to understand how the magnet will affect the ICD before magnet application. Removal of the magnet usually returns the ICD to the active mode. The rare exception may be the Boston Scientific Prizm series. Boston Scientific devices emit a tone for as long as the magnet is on the ICD. Medtronic devices emit a tone for approximately 30 seconds. The other devices do not emit a tone. A few devices in a specific scenario might not respond to a magnet. See Table 18-3.
16 Why is it important to know when pacemaker or ICD leads were inserted when considering placement of a central line?
20 How can electrocautery affect an ICD?
Key Points Pacemakers and Defibrillators
1 American Society of Anesthesiologists. practice advisory for the perioperative management of patients with cardiac implantable electronic devices: pacemakers and implantable cardioverter-defibrillators. Anesthesiology. 2011;114:247–261.
2 Crossley G.H., Poole J.E., Rozner M.A., et al. Heart Rhythm Society/American Society of Anesthesiologists expert consensus statement on the perioperative management of patients with implantable defibrillators, pacemakers and arrhythmia monitors: facilities and patient management. Heart Rhythm. 2011;8:1114–1152.
3 Lau W., Corcoran S., Mond H. Pacemaker tachycardia in a minute ventilation rate-adaptive pacemaker induced by electrocardiographic monitoring. Pacing Clin Electrophysiol. 2006;29:438–440.
4 Manegold J.C., Israel C.W., Erlich J.R., et al. External cardioversion of atrial fibrillation in patients with implanted pacemaker or cardioverter-defibrillator systems: a randomized comparison of monophasic and biphasic shock energy application. Eur Heart J. 2007;28:1731–1738.
5 Maron B.J., Estes M. Medical progress: commotio cordis. N Engl J Med. 2010;362:917–927.
6 Smirk F.H. R waves interrupting T waves. Br Heart J. 1949;11:23–36.