Chapter 173 Overview of Imaging Procedures Available for Spinal Diagnosis
Plain-Film Radiography
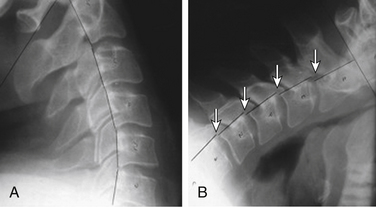
For basic anatomic depiction of the entire spinal column, plain films are optimal (Fig. 173-1). The images are relatively easy to obtain, the machines and film are readily available, and the images are mostly straightforward to interpret with a basic knowledge of spinal anatomy. Although actual hard-copy x-ray film is now replaced in many practices by direct digital images, there are still some older clinicians who insist on preserving the tactile experience of holding an x-ray film in their hands to aid in diagnosis. This will fade eventually, mostly because of cost factors (film is still fairly expensive, whereas digital images are not), but also because the benefits of going digital include the ability to change window widths, enlarge an area of interest, and store images on a central server and transmit them.1
One drawback is that proper radiographic technique must be used at all times and someone must ensure the dosages are correct and the images are diagnostic and satisfactory, or have them repeated. One must be cautious about the total ionizing radiation exposure to the patient, taking into account the number of repeated exposures endured, the part of the body being exposed, and the age of the patient.2 For instance, the total exposure of a newborn with hip dysplasia undergoing a plain radiographic examination every few weeks to determine if the therapeutic harness is working must be weighed against the fact that a superior method that does not involve ionizing radiation, ultrasonography, is available to accomplish the same end.
For evaluating the spine, plain radiographs have one distinct advantage over other imaging techniques: they observe the spine in a position of function, specifically, with the patient upright and bearing weight.3 This is not true of any other modality, with the exception of upright MRI (which has its own drawbacks). In addition, the spine can be imaged from a lateral viewpoint, with the patient engaging in flexion and extension, or with ventral views of the patient bending from side to side (Fig. 173-2; see Fig. 173-1). This can be performed using fluoroscopy as well, but plain radiographs are less expensive to produce and result in lower doses of radiation to the patient. Either technique is acceptable, provided the images are properly obtained and interpreted.
Plain radiographs can show excellent bony detail, assuming they are done correctly, and any fracture or misalignment is usually obvious. Instability is even more obvious if flexion and extension views are obtained.3 Congenital osseous abnormalities can be diagnosed and the normal curvatures of the spine assessed. Bearing in mind that not every individual naturally has the expected amounts of cervical and lumbar lordosis and thoracic kyphosis, observers should refrain from stating that loss of any of the spinal curvatures automatically means that the patient has muscle spasms in that region because that diagnosis can be made only by physical examination. Assessment of postural curves can be done only on upright images; otherwise, scoliosis, kyphosis, and lordosis are modified by the shape of the backboard or bed.
Myelography
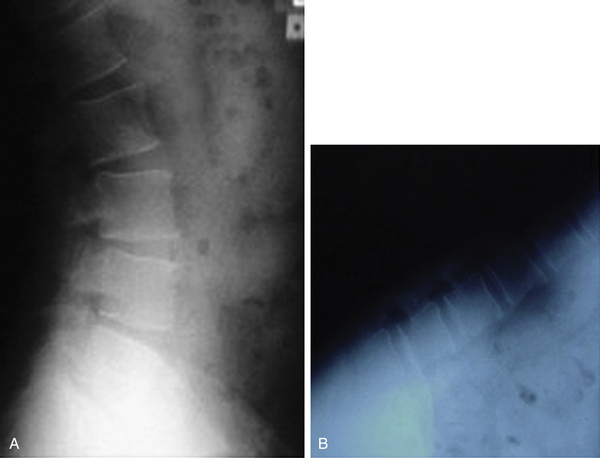
The most useful modern role of myelography is to reveal the details of the subarachnoid spaces in conjunction with anatomic detail provided by CT (Fig. 173-3). The myelogram/CT combination is the current gold standard of spinal imaging, but is used only as a last resort because it is, after all, an invasive procedure that requires a lumbar puncture and intrathecal injection.4
Fluoroscopy
This technique is essentially continuous, real-time radiography. Consequently, the dosages of radiation to the patient and to the operator can be very large if the physician is not aware of the fact that the longer the activation pedal is depressed, the more radiation is delivered.5 Although fluoroscopy can effectively evaluate motion of the spine in real time, with or without intrathecal contrast, flexion and extension plain films serve the same purpose, depict exactly the same anatomy, involve less radiation, and are less expensive to produce. The most frequent use of fluoroscopy today is in the form of the ubiquitous operating room C-arm used with every spinal surgical procedure for direction, localization, and documentation during and after surgery. It is very important that the operating physician be cognizant of the dose delivery curves for the specific machine that is being used, because they do vary according to manufacturer. Also, common sense dictates that the operator should not “keep their foot on the pedal” continually during usage, but instead develop the habit of taking “snapshots” of the target organ/structure as needed during the surgical procedure.
Computed Tomography
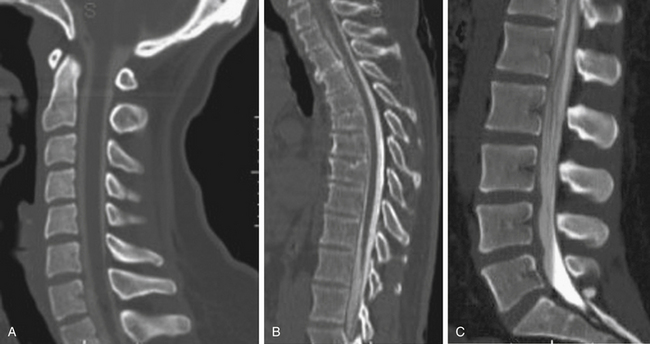
Computed tomography is an x-ray technique capable of producing images of the inside of the body using ionizing radiation (Fig. 173-4). As a result, CT carries the same risks and benefits as plain-film radiography. The x-ray source in the CT scanner is housed in a doughnut-shaped device that is capable of rotating circumferentially around the patient. Early-generation devices consisted of a single x-ray source and a single 180-degree detection device. In these devices, the x-ray beam passes through the body part of interest and exposes the detector on the opposite side in exactly the same manner as the plain radiograph is generated. Unlike plain radiographs, however, the CT x-ray source and detection device are capable of moving in tandem. After an image is created, the source and the detector move in parallel inside the cowling and another exposure is made, followed by another and then another. After the acquisition of multiple consecutive images, a computer compiles the image data and displays it according to complex algorithms as an axial image of the inside of the body part being imaged. This was a revolution—clearly as large a step forward as was Roentgen’s original hand x-ray image.
The early, single-row technique for CT scanning is a slow and cumbersome process. Since then, the CT scanner has evolved through at least eight additional generations to become the ultrafast, ultra-detailed diagnostic machine that it is today. Up to 256 x-ray sources and 256 corresponding detectors now image the body part at incredible speeds, producing excellent images in time frames that rarely exceed a few minutes. Although image resolution is significantly better and scan times markedly shorter, the dosage of ionizing radiation increases with every additional source/detector added and the radiation dosage to the patient can be massive. The 64-slice option is generally used only when imaging the beating heart. Most, if not all, of the fine imaging produced today, particularly when imaging the spine, is performed with the 16- or 32-slice options, which produce excellent images with much less radiation dosage.
There is no question that the anatomic detail of osseous structures such as the vertebral bodies and motion segments is best depicted with the CT scanner.6 Even though a CT scanner is capable of acquiring images only in the axial plane, powerful computer algorithms routinely allow extremely detailed sagittal and coronal images to be reconstructed during postprocessing, with very little effort. Surface algorithms are also available to build a three-dimensional representation of the surface of the spine that can then be rotated on the computer screen into any orientation the clinician requires. CT myelography provides an excellent in vivo demonstration of spinal anatomy and, as noted previously, is the gold standard of spine imaging, beating even the highest-quality MRI scan for detail of osseous and soft tissue anatomy on the same study (see Fig. 173-3).
Discography
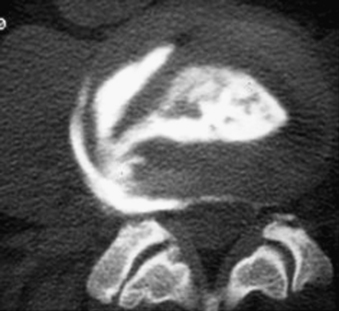
The old-fashioned discogram has made a resurgence (see Fig. 173-4). Direct injection of contrast material into the nucleus pulposus has always been an effective, if extremely painful, invasive procedure with the potential to yield valuable clinical information on the effect of pressure loading on an intervertebral disc.7 This procedure had limited usefulness until recently because of its invasiveness. There has always been the potential for development of discitis as an adverse outcome, and until recently the discogram technique has been difficult to master. With the advent of better C-arm fluoroscopy and fluoroscopy-like guidance applications for CT, direction of a needle into the exact center of a disc has become much easier and less painful for the patient, at least until the injection into the disc itself takes place. When a normal disc is pressure loaded with 1 mL or more of contrast material, it typically does not respond by duplicating or significantly worsening the patient’s pain. However, when the material is injected into a disc that is responsible for the patient’s symptoms, those symptoms are typically made much worse, and the disc can then be labeled a “pain generator.”7,8 Axial CT images of the disc may then be acquired that often adequately demonstrate the internal architecture of the disc and the extent of anular tearing that is present. The modern discogram, properly performed, has definite value as an adjunct to other routine diagnostic procedures, but because it is still an invasive procedure it is reserved for the most difficult diagnostic problems. Carragee et al. received a prize at the 2009 meeting of the International Society for the Study of the Lumbar Spine for their review of 10 years of follow-up from discography. They showed that there was “accelerated disc degeneration, disc herniation, loss of disc height and signal and the development of reactive end plate changes compared to match-controls.”9 Therefore, when MRI or CT myelography does not yield a clear diagnosis, one may consider discography.8
Diagnostic Spinal Anesthetic and Steroid Injections
These are anesthesia procedures that have been adapted to the imaging realm by adding image guidance to aid proper performance and improve outcomes. Whether that guidance is with fluoroscopy or CT makes no difference, as long as proper protocol is followed. The target is either a facet joint or a dorsal root ganglion as it exits the nerve root foramen. In either case, care must be taken in the cervical and thoracic spine to avoid injection into a vascular structure, such as a radicular artery or vein, which might supply/drain into the spinal cord and cause a cord infarct. If the injection is into a nerve root or a nerve root sleeve, it is technically a localized epidural steroid injection. If the injection is into a facet joint, it is an intra-articular injection into a synovial joint. In either case, temporary relief of the patient’s specific pain sensations is good diagnostic information that the injected structure is anatomically either entirely or partially responsible for the patient’s pain syndrome. These minimally invasive procedures are also reserved for cases in which there is still some question of diagnosis after exhausting all other noninvasive diagnostic modalities.8
Magnetic Resonance Imaging
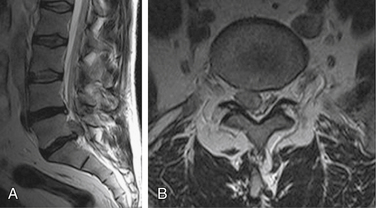
Magnetic resonance imaging provides visualization of the vertebral bodies, thecal sac and intradural structures, disc spaces, and adjacent soft tissue structures of the spine with startling clarity, and without resorting to invasive maneuvers (Fig. 173-5). MRI was so revolutionary when it appeared in the mid-1980s that everyone wanted their own machine. Despite the immense setup costs involved, the new technique was so well reimbursed and so lucrative that even a businessman without any medical experience knew that he could buy a scanner, hire a radiologist, and be profitable.10 As a direct result of those initial economic conditions, which lasted well into the turn of the century, there are now many more MRI scanners than are necessary in the United States. A legitimate argument can be made that the ultimate cost of MRI scanner proliferation to the American medical bottom line was at least partly responsible for today’s medical insurance crisis.11
The differences in image quality between open and closed systems is directly related to field strength.12 Faster MRI scanners in the 1.5- to 3-Tesla field-strength range are routinely capable of producing superior anatomic detail compared with lower field-strength machines. On the other hand, there is the minor downside of the enclosed magnet bore (uncomfortable for those claustrophobic and/or very large patients) and the problem of core heating (referred to as SAR, the specific absorption rate). As a result, one must consider the trade-off between image quality and speed of acquisition versus patient comfort when ordering MRI studies. Unlike the hazards of ionizing radiation in x-ray techniques, the downsides of long-term exposure to high magnetic fields are not well known at this time and may be nonexistent other than core heating.
The only absolute contraindication to MRI today appears to be the presence of a cardiac pacemaker, implantable defibrillator, or spinal cord stimulator. Virtually all other modern devices, including stents, aneurysm clips, surgical clips, orthopaedic implants, spinal fixation screws, and fusion constructs, are thought to be safe because no manufacturer today makes surgically implanted devices from ferromagnetic materials. MRI compatibility should, however, be confirmed with a reliable source before imaging.13 Pregnant women should not be imaged in the first trimester unless the risk-benefit ratio indicates otherwise. Contrast administration with gadolinium carries a very rare but specific risk of systemic fibrosis and should be used only in patients with suitable renal function.14 Fortunately, there are not many instances in which contrast is warranted when imaging the spine for anything but tumors and postoperative examination of the lumbar spine.
Axial and sagittal T1- (T1WIs) and T2-weighted images (T2WIs) are typically all that is required for imaging of the cervical, thoracic, and lumbar spine. If there is a question of congenital vertebral body abnormality, as in children with scoliosis, a sequence in the coronal plane is also indicated. T2WIs can be either T2* (gradient echo) images or fast-spin echo T2. If there is a question of metastatic disease, or acute fracture, a sagittal short-tau inversion recovery (STIR) sequence can be added to evaluate for marrow edema. At least one series of axial T2WIs is necessary, and it is helpful if a gradient echo sequence is added as well. The axial images should be 3 to 4 mm thick and contiguous. Some 3-Tesla scanners are capable of excellent 1- and 2-mm thick, contiguous axial T2WIs, which are ideal for spinal cord anatomy. A series of axial T1WIs can also be added.
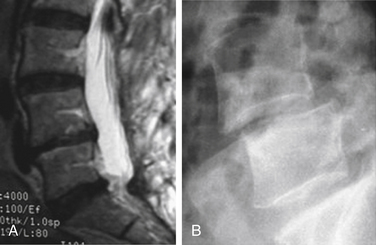
One drawback with conventional MRI is that the patient is not in a position of function when the spine is being studied.15 The patient must be supine to fit into the bore of the high-field machine and into the image volume of most of the open MRI scanners. Because the spine is not weight bearing in such a position, some information may be lost, as in the case of a 65-year-old man who had a perfectly aligned spine while recumbent in the scanner (with a few degenerative discs) but who clearly exhibited instability when the upright, weight-bearing plain radiograph was obtained (Fig. 173-6). Open upright MRI scanners have been developed and are in the community, but they are available only as low-field scanners, which are less technically optimal than high-field systems.
Nomenclature
One of the more Sisyphean projects of all time has been the American Society of Spine Radiology’s (ASSR) Nomenclature Project, an attempt to bring consistency to the naming of disc abnormalities.16 The project was initiated in 1994 and was not formalized until the year 2000. The ASSR initially saw a need to bring consensus to the chaotic nomenclature of disc abnormalities, as first proposed in the seminal article by Jensen et al.17 The resultant 54-plus-page document earned the stamp of approval of all of the major spine organizations, yet is still not widely used even today. The entire document is very accessible and appears in its entirety online at www.asnr.org/spine_nomenclature.
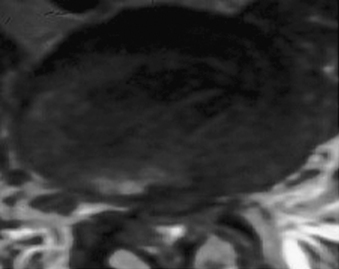
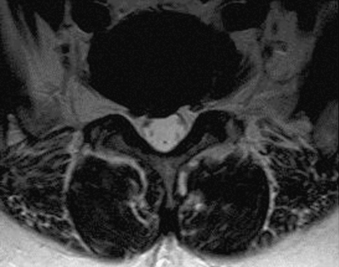
Historically, nearly everyone involved in diagnosing and treating spinal diseases had an unfortunate tendency to refer to every disc abnormality, no matter what it looked like, as a “herniation.” With the superior routine ability to visualize spine anatomy that came with the advent of MRI, it was clear that there were multiple variations. “Herniations” are now subdivided into “protrusions” and “extrusions,” depending on morphology, and neither one should be confused with a degenerative disc “bulge” (Figs. 173-7 to 173-9). As defined by the Nomenclature Project, a disc bulge is a deformity of the circumference of a disc margin between 90 and 360 degrees, whereas a protrusion is a deformity of less than 90 degrees. An extrusion is a true “herniated nucleus pulposus” in which nuclear material extrudes through a full-thickness defect of the anulus. The project is currently limited to describing only lumbar discs, but may be applied empirically to thoracic and cervical discs. However, it is important to take into account anatomic differences among the three regions, which probably are not significant when considering thoracic discs, but can cause problems when viewing cervical discs because of their morphology, particularly the presence of lateral limitation afforded by zygapophyseal joints.
Fardon D.F., Milette P.C., et al. for the combined task forces: Nomenclature and classification of lumbar disc pathology: recommendations of the combined task forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. http://www.asnr.org/spine_nomenclature/. American Society of Neuroradiology websiteUpdated February 2003. Accessed September 10, 2011
Leone A., Gugliemi G., Cassar-Pullicino V.N., et al. Lumbar intervertebral instability: a review. Radiology. 2007;245:62-77.
Jensen M.C., Brant-Zawadzki M.N., Obuchowski N., et al. MRI of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69-73.
Walker J., El Adb O., Isaac Z., et al. Discography in practice: a clinical and historic review. Curr Rev Musculoskelet Med. 2008;1:69-83.
Williams A.L., Murtagh F.R. Handbook of diagnostic and therapeutic spine procedures. St. Louis: Mosby; 2002.
1. Chotas H.G., Dobbis J.T., Ravin C.E. Principles of digital radiography with large-area, electronically readable detectors: a review of the basics. Radiology. 1999;210:595-599.
2. Vano E., Fernandez J.M., Ten J.I., et al. Transition from screen-film to digital radiography: evolution of patient radiation doses at projection radiography. Radiology. 2007;243:461-466.
3. Leone A., Gugliemi G., Cassar-Pullicino V.N., et al. Lumbar intervertebral instability: a review. Radiology. 2007;245:62-77.
4. Miller G.M., Krauss W.E. Myelography: still the gold standard [editorial]. AJNR Am J Neuroradiol. 2003;24:298.
5. Perisinakis K., Damilakis J., Theocharopoulos N., et al. Patient exposure and associated radiation risks from fluoroscopically guided vertebroplasty or kyphoplasty. Radiology. 2004;232:701-707.
6. McAfee P.C., Ullrich C.G., Levinsohn E.M., et al. Computed tomography in degenerative lumbar spinal stenosis: the value of multiplanar reconstruction. Radiographics. 1982;2:529-551.
7. Walker J., El Adb O., Isaac Z., et al. Discography in practice: a clinical and historic review. Curr Rev Musculoskelet Med. 2008;1:69-83.
8. Williams A.L., Murtagh F.R. Handbook of diagnostic and therapeutic spine procedures. St. Louis: Mosby; 2002.
9. Carragee E.J., Angus S.D., Hurwitz E.L., et al. Does discography cause accelerated progression of degeneration changes in the lumbar disc: a ten-year matched cohort study. Spine (Phila Pa 1976). 2009;34:2338-2345.
10. Bell R.A. Magnetic resonance in medicine in 2020. http://www.imagingeconomics.com/issues/articles/2004-12_02.asp.. Imaging Economics website. December 2004Accessed September 10, 2011
11. Abelson R., An M.R. I machine for every doctor? Someone has to pay. New York Times. http://www.nytimes.com/2004/03/13/business/an-mri-machine-for-every-doctor-someone-has-to-pay.html. March 13, 2004Accessed September 10, 2011
12. Jarvik J.G., Roberston W.D., Wessbecher F. Variation in the quality of lumbar spine MR images in Washington State. Radiology. 2000;215:483-490.
13. MRIsafety. www.mrisafety.com. Accessed February 11, 2010.
14. American College of Radiology. Updated ACR screening recommendations on gadolinium-based MR contrast agents, renal disease patients, and nephrogenic systemic fibrosis (NSF). http://www.acr.org/SecondaryMainMenuCategories/quality_safety/Contrast_manual/FullManual.aspx.
15. Weishaupt D., Schmid M.R., Zanetti M. Positional MR imaging of the lumbar spine: does it demonstrate nerve root compromise not visible at conventional MR imaging? Radiology. 2000;215:247-253.
16. Fardon D.F., Milette P.C., et al. for the combined task forces: Nomenclature and classification of lumbar disc pathology: recommendations of the combined task forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology,. http://www.asnr.org/spine_nomenclature/. American Society of Neuroradiology websiteUpdated February 2003. Accessed September 10, 2011
17. Jensen M.C., Brant-Zawadzki M.N., Obuchowski N., et al. MRI of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69-73.