18
Ovarian neoplasms
Introduction
Ovarian cancer is the second most common of the gynaecological malignancies in most affluent countries, and the incidence is rising. In the UK, there are around 7000 newly diagnosed cases each year and approximately 4300 women annually die of the disease. The overall 5-year survival is around 40%.
Ovarian cancer occurs predominantly in the fifth, sixth and seventh decades of life, with the peak age being around 75 years.
Natural history
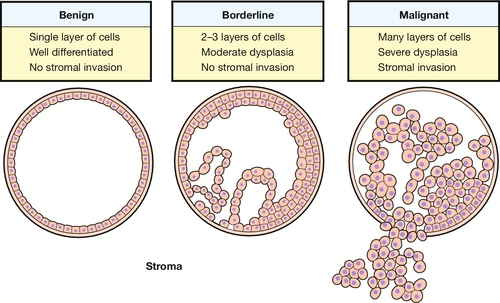
Unlike cervical cancer, there is no clearly defined pre-invasive ovarian lesion. Benign, borderline and invasive tumours are recognized but these are distinct pathological entities and there is little evidence of progression from one to the other (Fig. 18.1). Indeed, there is even controversy about whether malignant epithelial tumours, which are the most common, arise from the ovary and then metastasize or arise as multicentric disease de novo. The multicentric theory is supported by the fact that ovarian-like tumours can arise in the peritoneum of women who have previously had both ovaries removed. Cancer in this case is called primary peritoneal cancer.
Aetiology
It is entirely possible that the different types of ovarian neoplasm have differing aetiologies, particularly as germ cell tumours, which account for 25% of ovarian neoplasms, occur in much younger women than do the epithelial tumours.
Reproductive history
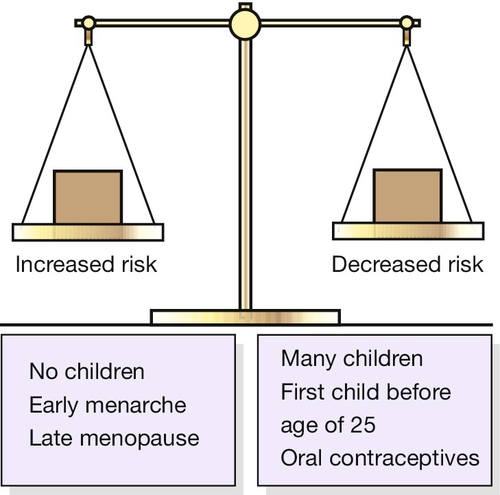
Reproductive history is an important determinant of epithelial ovarian cancer risk. Nulliparous women have a higher risk than parous women and the risk is inversely correlated with parity (Fig. 18.2). It is thought that the number of ovulation events in a woman’s reproductive life is the main risk factor.
Exogenous oestrogens
Oral contraceptives
Overwhelming evidence now exists that women who have used the combined oral contraceptive pill at some stage in the past have a reduced risk of developing ovarian cancer. The longer the use, the lower the risk. This is again thought to be through the reduction in the number of ovulation events.
Hormone replacement therapy (HRT)
In postmenopausal women, the effect of oestrogen replacement therapy has been investigated because of a reported increased risk in women who received diethylstilboestrol (a non-steroidal oestrogen) early in life. The balance of evidence, however, suggests that HRT has no significant effect on ovarian cancer risk.
Repeated (incessant) ovulation
It has been suggested that the more often a woman ovulates, the greater the risk of ovarian carcinoma. The apparently protective effects of both pregnancy and the combined oral contraceptive pill further support this theory. The mechanism is uncertain, but it may be that repeated monthly repair of the ovarian epithelium after ovulation predisposes to malignant change. Despite this plausible theory, however, it is likely that ovarian carcinogenesis is multifactorial.
Genetic factors
It is now accepted that a genetic predisposition exists in at least a proportion of ovarian cancer cases. Although overall, there is a slightly increased risk of ovarian cancer in those with a family history, the risk is small for most categories except for those of early onset, and those with more than one affected first-degree relative. If one affected primary relative has ovarian cancer and the cancer was diagnosed when she was < 50 years old, a woman’s risk of developing ovarian cancer is around 5%. If there are two primary relatives under the age of 50 years with the disease, the risk is approximately 25%.
Only 5–10% of cases of ovarian carcinoma, however, have a direct genetic association. Of particular significance in this small group are the breast–ovarian cancer tumour suppressor genes BRCA1 and BRCA2, as these are associated with a 10–50% lifetime risk of developing ovarian carcinoma. Mismatch repair genes associated with cancer of the colorectum, endometrium, stomach, urinary tract and small bowel are also responsible for a small proportion of this hereditary group. Women with such a history may warrant regular screening, and it is reasonable to consider bilateral oophorectomy after completion of their family. Such an operation will substantially reduce the risk but will not prevent primary peritoneal carcinoma.
Other factors
There has been controversy about the possible role of asbestos and talcum powder in the aetiology of ovarian cancer. Insufficient evidence in the form of case–control studies exists to completely dismiss reported associations. Similar problems beset the assessment of smoking, diet and alcohol consumption.
Pathology
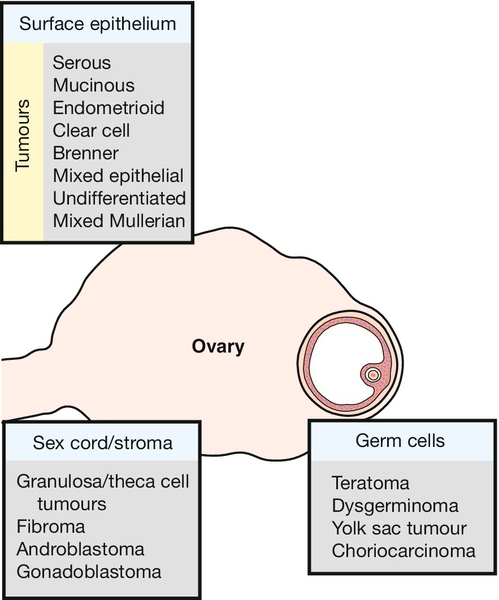
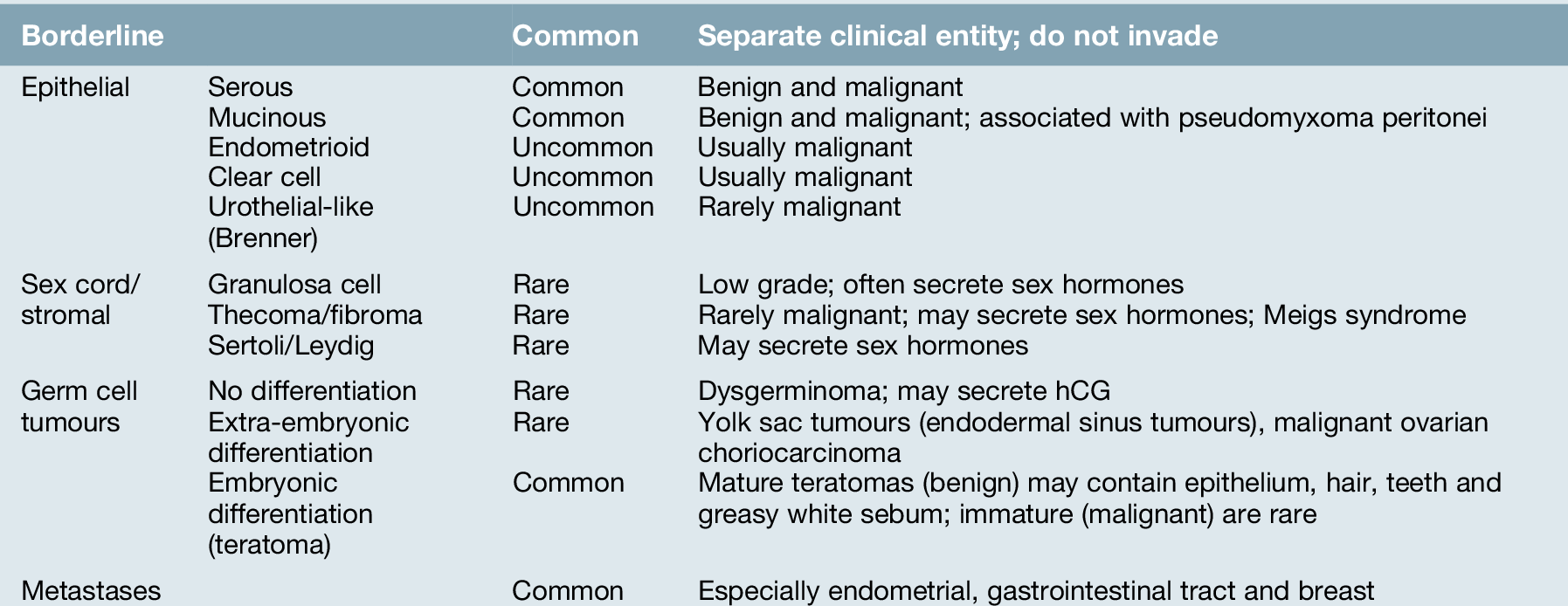
Neoplasms can arise from any of the elements that comprise a mature ovary, including its surface serosal or mesothelial elements (Fig. 18.3). A number of simpler themes can be drawn from a wide diversity of tumour types, namely: epithelial tumours, which are by far the most common (70% of primary ovarian tumours); sex cord/stromal tumours; germ cell tumours; and metastatic tumours (Table 18.1). Most of the epithelial tumour types can be further broadly classified as benign, borderline or malignant.
Borderline tumours
The term ‘borderline’ is reserved for tumours which display the characteristics of malignant tumours but show no evidence of invasion. Women with borderline ovarian tumours have a much better prognosis than those with frankly malignant tumours. Nevertheless, long-term survival is by no means as high as might be expected and late recurrence up to 20 years after removal of the primary does occur. Despite lacking the features of invasion, these tumours may present at an advanced stage, raising the possibility of multicentric origin. The treatment of these is predominantly surgical as they tend to be resistant to chemotherapy.
Epithelial tumours
Serous tumours
Serous tumours are the most common ovarian neoplasm, accounting for almost 50% of ovarian cancers. They also account for 20% of all benign ovarian tumours, and these cases occur primarily in women of reproductive age. Serous cystadenomas (benign) are usually unilocular cysts, filled with straw-coloured fluid and of variable size (Fig. 18.4). They are bilateral in 20% of cases. Serous cystadenocarcinomas involve both ovaries in over 50% of cases and may have both cystic and solid components. Psammoma bodies, concentrically laminated calcified concretions, are a frequent histological finding.
Mucinous tumours
These comprise 20% of all ovarian tumours and less than 10% are malignant. Benign tumours are usually unilateral and only 20% of malignant tumours are bilateral. Mucinous tumours are usually multiloculated and contain mucinous fluid of variable viscosity. They are generally the largest of the common epithelial tumours. Uncommonly, concomitant pseudomyxoma peritonei may be present. There is characteristic gelatinous tumour within the peritoneal cavity. It is unclear to what extent pseudomyxoma peritonei truly arises from the ovary rather than from a primary mucinous tumour of the appendix.
Endometrioid tumours
Endometrioid tumours are usually malignant and closely mimic endometrial cancer in histological appearance. In around 30% of cases there is a coexistent second primary in the endometrium.
Clear cell tumours
These are virtually all malignant and may be a variant of endometrioid tumours. They are the most frequent epithelial tumour found in association with ovarian endometriosis. It must be emphasized however, that ovarian cancer developing from endometriosis is uncommon.
Urothelial-like tumours
Urothelial-like or Brenner tumours (history box) are uncommon, usually unilateral and rarely malignant. They in part comprise epithelium of urothelial type but their main component is ovarian stroma. A rare aggressive variant is the urothelial or transitional cell carcinoma.
Sex cord/stromal tumours
Rare neoplasms, which comprise < 5% of all ovarian tumours.
Granulosa cell tumours
These are functional low-grade cancers and account for around 5% of ovarian malignancies. Three-quarters secrete sex hormones, most commonly oestrogen, which in turn may lead to precocious pseudopuberty, irregular menstrual bleeding or postmenopausal bleeding, depending on the age of presentation. They tend to recur late but can be monitored with serum oestradiol measurements. Characteristically they contain cells with ‘coffee bean’ nuclei and ‘gland-like’ spaces called Call–Exner bodies (see History box), which are pathognomonic.
Thecoma/fibroma
These tumours are usually unilateral and rarely malignant. They contain cells ranging from theca cells to fibroblastic-type cells. Tumours containing the former are oestrogenic, although they are less common than granulosa cell tumours. Rarely, ovarian fibromas may present with non-malignant ascites and pleural effusion, which resolve after removal of the tumour (Meigs syndrome, see History box).
Sertoli/Leydig cell tumours
These are among the rarest ovarian tumours, accounting for < 1% of such. They occur in young women, the mean age being in the mid-20s. They are almost invariably unilateral and are commonly androgenic, though many are non-functional and only a few are oestrogenic. They contain either Sertoli cells or Leydig cells (see History boxes) and in the case of the latter, may be accompanied by stroma-derived fibroblasts.
Germ cell tumours
This heterogeneous group of tumours affects mainly children and young women and comprises 20–25% of all ovarian tumours. Only around 4% are malignant. However, they represent the majority of ovarian tumours in children, where around one-third are malignant.
Teratoma
Teratomas are colloquially known as ovarian dermoid cysts, and these are almost always benign and are very common. They characteristically contain elements from all three embryonic germ cell layers and are thought to occur via parthenogenesis, a form of reproduction in which the ovum develops without fertilization. Mature teratomas may contain epithelium, hair, teeth and greasy white sebum, and constitute 20% of all ovarian neoplasms. They are commonest in women in their 20s but account for 50% of ovarian neoplasms in females under 20 years. Malignant change, usually squamous cell, is rare (< 1%) and usually occurs in postmenopausal women.
Immature teratomas are rare, characteristically occurring in children under 15 years of age. Specialized tissue derivatives from a single germ layer are found in 3% of teratomas, notably among those with predominantly thyroid tissue (struma ovarii) and carcinoid tumours.
Dysgerminoma
Dysgerminoma is the most common malignant germ cell tumour, comprising at least 50% of this group. Nevertheless, it is relatively uncommon and represents only 3% of all ovarian cancers. Some 75% occur in females aged 10–30 years, the median being 22 years, and it is the most frequently encountered ovarian malignancy in pregnancy. It is also the malignancy most likely to be associated with gonadoblastoma in gonadal dysgenesis. At least 10% are bilateral and there may be a raised serum human chorionic gonadotrophin (hCG) level.
Endodermal sinus or yolk sac tumour
This is the second most common malignant germ cell tumour of the ovary but comprises only 1% of all ovarian cancers. It rarely affects women over 40, the median age being 19 years. Presentation is commonly with a sudden onset of pelvic symptoms and a pelvic mass. Elevated serum levels of alpha-fetoprotein are found with normal hCG levels. Coexistent teratomas are found in 20% of patients.
Choriocarcinoma
These secrete hCG and may present with precocious pseudopuberty. They have a poor prognosis and do not respond well to chemotherapy (unlike uterine trophoblastic disease).
Metastatic tumours
Secondary tumours in the ovaries are surprisingly common. Cervical cancer only rarely metastasizes to the ovaries, but spread from endometrial cancer is far more frequent. Breast cancer may also metastasize to the ovaries, and patients presenting with single or bilateral ovarian masses should be examined carefully to exclude a breast lesion.
Cancers of the gastrointestinal tract also metastasize to the ovary and in the case of gastric cancer give rise to the so-called Krukenberg tumour (see History box). This contains mucin-producing ‘signet ring’ adenocarcinoma cells. Such tumours may elicit a stromal response in the ovary, which may cause hormone production; as a result, virilization may be a presenting complaint. In such cases, confusion with sex cord/stromal tumours is possible, although these, unlike Krukenberg tumours, are usually unilateral.
Spread
Ovarian cancer spreads trans-coelomically, whereby tumour is ‘seeded’ onto the surfaces of the intraperitoneal structures and organs. Those who die usually do so from intestinal obstruction and cachexia as a consequence of widespread intraperitoneal disease. Intrahepatic metastases and malignant pleural effusions are seen, and para-aortic lymph node metastases are found in up to 18% of cases where the disease appears otherwise to be confined to the ovary.
Presentation
As a rule, ovarian cancer tends to present at a late stage. Occasionally, ovarian cancers are diagnosed incidentally during pelvic or abdominal palpation for another reason. This mode of presentation, however, is the exception rather than the rule. In general the symptoms are diverse and non-specific. As a result, patients often do not recognize the sinister nature of their symptoms, and the disease progresses insidiously until they develop gastrointestinal complications or bowel obstruction secondary to widespread intraperitoneal malignancy. This is the reason for a new guideline from NICE emphasizing the importance of investigating persistent nonspecific symptoms.
The varied nature of these symptoms results in many cases being referred to inappropriate specialties for investigation. The most frequent complaint is abdominal distension due either to ascites or masses (Table 18.2). The most common clinical signs are an abdominal or pelvic mass and ascites (Table 18.3).
Table 18.2
Symptoms in ovarian cancer
| Symptom | % of patients |
| Pain (late symptom) | 50–60 |
| Abdominal swelling (persistent bloating) | 50–65 |
| Anorexia | 20 |
| Nausea and vomiting | 20 |
| Weight loss | 15 |
| Abnormal vaginal bleeding | 15 |
| Frequency | 10 |
| Malaise | 5 |
| Change in bowel habit | 5 |
| Virilization | Rare |
| Precocious puberty | Rare |
Table 18.3
Signs in ovarian cancer
| Sign | % of patients |
| Pelvic mass | 70–80 |
| Abdominal mass | 60–70 |
| Ascites | 30–40 |
| Pleural effusion | 10–15 |
| Hepatomegaly | < 5 |
| Cervical lymphadenopathy | < 5 |
Investigation and staging
If there is a low index of suspicion, investigation is often with ultrasound and tumour markers. The risk of malignancy index (RMI) aids in the differentiation of benign from malignant lesions (RMI = ultrasound score × menopausal score × CA125). If the index of suspicion is high, then CT or MRI can be used in addition to the tumour markers to examine the pelvis, and to look for peritoneal spread, ascites, liver metastases and ureteric obstruction. An X-ray or CT scan of the chest is important to look for pleural effusions or macroscopic chest disease. Until a mass has been assessed histopathologically, it is never possible to be certain of its exact nature. Across the UK any suspected ovarian cancer should be referred to a specialist gynaecological-oncology team who will assess the potential diagnosis and decide upon appropriate management through a multidisciplinary meeting. This team comprises gynaecological surgeons, oncology physicians, radiologists and pathologists, among other specialists such as nurse specialists. It is through this process that the management of all gynaecological cancers will be determined.
Ovarian cancer is staged surgically according to the FIGO system (Table 18.4).
Table 18.4
Staging of ovarian cancer
| Stage | Definition | 5-year survival |
| IA | One ovary | |
| IB | Both ovaries | 60–70% but can be 95% for IA |
| IC | IA or IB with ruptured capsule, tumour on the surface of the capsule, positive peritoneal washings or malignant ascites | |
| IIA | Extension to uterus and tubes | |
| IIB | Extension to other pelvic tissues, e.g. pelvic nodes, pouch of Douglas | 50% |
| IIC | IIA or IIB with ruptured capsule, positive peritoneal washings or malignant ascites | |
| IIIA | Pelvic tumour with microscopic peritoneal spread | |
| IIIB | Pelvic tumour with peritoneal spread < 2 cm | 20% |
| IIIC | Abdominal implants > 2 cm ± positive retroperitoneal or inguinal nodes (Fig. 18.5) | |
| IV | Liver parenchymal disease. Distant metastases. If pleural effusion, must have malignant cells | 6% |
Tumour markers
Around 80% of epithelial ovarian cancers are associated with elevated levels of a tumour marker (blood test) called CA125. This marker is of value in the assessment of patients presenting with pelvic masses, as well as in sequentially monitoring the response to treatment and to help identify presymptomatic relapse during follow-up. However, CA125 may also be elevated in the serum of women with benign conditions, such as endometriosis, or where peritoneal irritation has taken place. It can also be elevated in cardiac failure (particularly right sided), hepatic failure and some systemic inflammatory conditions. A positive result, therefore, while suggestive of ovarian cancer, is not diagnostic. Conversely, a negative result for tumour markers does not exclude a diagnosis of ovarian cancer, as 50% of stage 1 (confined to the ovary) ovarian cancers will have a normal CA125.
About 65% of ovarian germ cell tumours produce elevated serum levels of hCG, alpha-fetoprotein or both. These markers can again, if elevated, be very useful in monitoring response to therapy and in detecting tumour recurrence after completion of therapy.
Treatment
Benign tumours
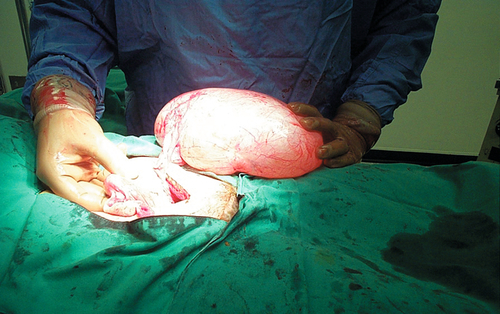
Benign tumours require either excision or possibly drainage under laparoscopic control. There may be difficulties in deciding whether a cyst is benign or malignant. In general, ovarian cysts in young women tend to be benign and the risk of malignancy increases with age. A cyst is often assumed at surgery to be benign if it is unilateral and unilocular with smooth external and internal surfaces and no solid elements (Fig. 18.4). Although not conforming to this rule, teratomas are benign and the diagnosis is usually obvious when they are opened after removal.
Epithelial cancers
Most patients with epithelial ovarian cancer present late and the overall survival is poor (Fig. 18.5). Because of this and because of new developments, particularly with chemotherapeutic agents, the modern approach to treatment is to consider ovarian cancer as a chronic disease. This means that the tumour is primarily treated with the aim of achieving remission but accepting that the tumour will probably become active again in the future. When this occurs, further treatment to achieve control will be given. In this way, while most patients will not be cured in the conventional sense, many patients will have a prolonged period of good-quality life.
Optimal debulking was not achieved.
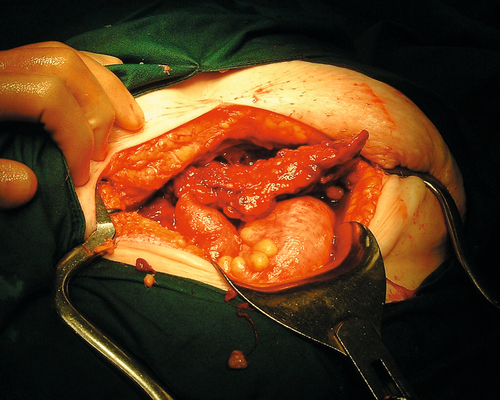
Treatment is usually a combination of surgery and chemotherapy. Traditionally, this has been in the form of aggressive surgery attempting to remove all areas of tumour and including removal of both ovaries, the uterus and omentum. Complete removal of tumour is often unrealistic however, and the concept of surgical debulking has arisen. This is where the tumour deposits are removed as far as possible, aiming to reduce the size of deposits to below 1 or 2 cm in dimension. Chemotherapy will almost certainly be used as well. In this setting, it is called ‘adjuvant chemotherapy’. There are many active chemotherapeutic agents that can be used in ovarian cancer. In the first-line setting, the current standard is platinum-based. This is usually carboplatin, which will usually be combined with a taxane. This chemotherapy is given over 6 cycles and usually in the outpatient setting.
Recently, in many cancer centres, a different approach has been adopted for the most advanced cases of ovarian cancer. These patients are frequently unfit and with the advent of CT imaging, it is easier to identify patients in whom surgery will achieve little. In these cases, after histological confirmation with guided needle biopsy, chemotherapy is used first of all rather than surgery. Surgery will usually be considered midway through the chemotherapy treatment. The effect of this is more rapid control of the cancer and a reduction in the surgical related morbidity. This approach of neoadjuvant chemotherapy followed by surgery is currently being evaluated by randomized trial.
Most patients with advanced ovarian cancer will relapse at some point after primary treatment. In this situation, further chemotherapy will usually be considered. The specific type of chemotherapy will depend upon the chemotherapy that has been used in the past, as well as the interval since chemotherapy was last used. In the case of the first relapse, if the interval since treatment is significant, then further challenge with carboplatin will frequently be tried. Other drugs include the taxanes, topotecan and Caelyx and more recently, Avastin. Ideally, patients should be considered for entry into clinical trials, as the evidence suggests that patients who are entered into trials tend to have better outcomes. Many patients will have several lines of chemotherapy over a number of years before eventually dying of their disease. As most patients will eventually die of their disease progression, it is important to consider formal palliative care when appropriate.
In young women who wish fertility to be preserved and in whom the disease appears confined to one ovary, it is reasonable to consider conservative surgery. The other ovary and omentum, a common site for metastases, should be biopsied and a thorough inspection made of all peritoneal surfaces.
Non-epithelial tumours
These tumours frequently occur in young women where preservation of fertility is an important consideration. It is also clear that many of these tumours, especially those of germ cell origin, are exquisitely sensitive to chemotherapy, and radical surgery is therefore inappropriate. Extremely good survival can be achieved with limited surgery and subsequent combination chemotherapy.
Survival
It is difficult to accurately estimate survival and the rate depends upon methodology and definitions. Overall 5-year survival (all stages) is in the order of 40% (Table 18.4). Although the overall prognosis from ovarian cancer is poor, the 5-year survival has improved markedly over the past three decades. A better prognosis can be expected for women with malignant germ cell tumours, where the reported 5-year survival from most studies is in excess of 75%.
The only real prospect for improving survival in epithelial cancers is either detection at an early stage or development of better chemotherapy. Screening is still the subject of research, with trials involving the combination of tumour markers (such as CA125) and ultrasound. At present, it seems unlikely that screening and early detection of low-risk groups is going to be a useful proposition.