99
Other Lymphoproliferative and Myeloproliferative Diseases
Benign Lymphoctic Infiltrates
Lymphocytic Infiltrate of Jessner
• Males = females; onset typically during middle age; very rare in children.
• Most commonly appears on the head, neck, and upper back as one or several asymptomatic, erythematous papules, plaques (often annular) > nodules (Fig. 99.1); no secondary or surface changes (such as scale or crust).

Fig. 99.1 Lymphocytic infiltrate of Jessner. Annular erythematous plaque with central clearing on the face.
Cutaneous Lymphoid Hyperplasia (CLH); also known as ‘Pseudolymphoma’ or ‘Lymphocytoma Cutis’
• Females > males; adults > children.
• Presents most often on the head, neck, and upper extremities as one or several firm, erythematous to violaceous papules, plaques, or nodules (Fig. 99.3); usually no surface changes.
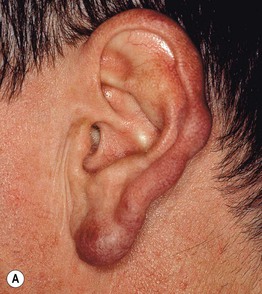

Fig. 99.3 Cutaneous lymphoid hyperplasia (lymphocytoma cutis). A Violet papulonodules on the helix and lobe of the ear (unknown etiology). B Multiple red-brown to violet papules at the sites of Hirudo medicinalis (medicinal leech) application. B, Courtesy, Josef Smolle, MD.
• Often spontaneously resolves without scarring.
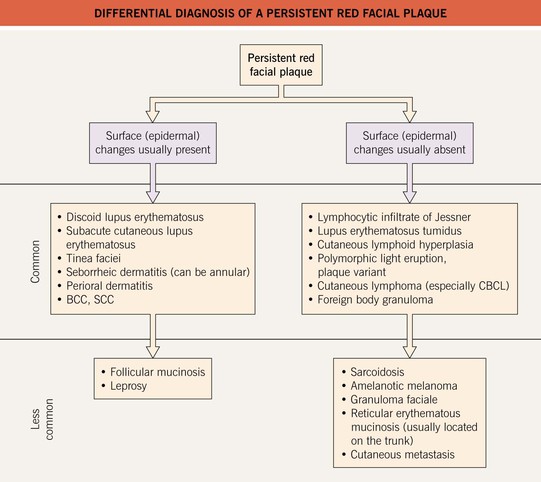
• DDx (see Fig. 99.2): lymphocytic infiltrate of Jessner, lymphoma cutis, leukemia cutis, solid organ metastases, and occasionally adnexal tumors.
Extramedullary Hematopoiesis
• Clinically presents with erythematous to violaceous papules and nodules > plaques, ulcers, or nasal polyps (Fig. 99.4).

Fig. 99.4 Extramedullary hematopoiesis. ‘Blueberry muffin baby’ secondary to congenital rubella. Courtesy, James Graham, MD.
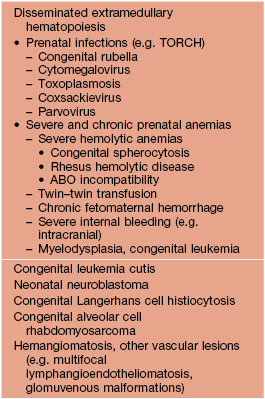
• When widely disseminated (typically in neonates) it leads to the classic ‘blueberry muffin baby’ presentation (Table 99.1).
• DDx: see Table 99.1 for neonates, leukemia cutis in adults.
Malignant Hematopoietic Infiltrates
Leukemia Cutis
• Cutaneous lesions associated with both acute and chronic leukemias may be either (1) nonspecific reactive skin lesions (Table 99.2) or (2) specific infiltrates, called ‘leukemia cutis’.
Table 99.2
‘Inflammatory’ disorders associated with acute and chronic leukemias.
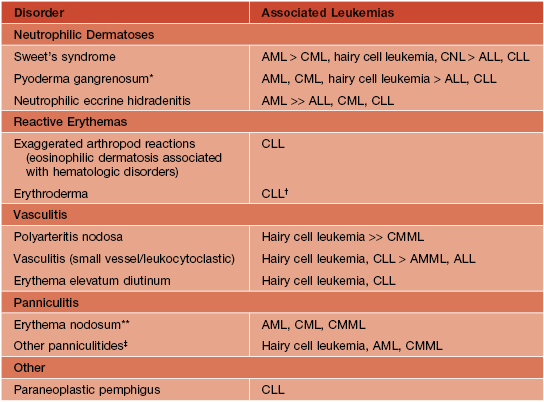
* Especially bullous.
† Many probably represent Sézary syndrome.
** Isolated case reports; may occur concomitantly with Sweet’s syndrome.
‡ Sweet’s syndrome may have a subcutaneous component.
ALL, acute lymphoblastic leukemia; AML, acute myelogenous leukemia; AMML, acute myelomonocytic leukemia; CLL, chronic lymphocytic leukemia; CML, chronic myelogenous leukemia; CMML, chronic myelomonocytic leukemia; CNL, chronic neutrophilic leukemia.
• Leukemia cutis typically presents as erythematous to violaceous firm papules or nodules (Fig. 99.5); less often purpura, ulcers, and rarely bullae; lesions may be hemorrhagic due to thrombocytopenia.

Fig. 99.5 Leukemia cutis. Multiple red-brown papules and plaques in a patient with hairy cell leukemia.
• Favors head, neck, trunk, and sites of scars or trauma.
• Less common presentations of leukemia cutis: chloromas, gingival hyperplasia.
Hodgkin Disease (HD; Hodgkin Lymphoma)
• Secondary cutaneous HD, occurring in patients with advanced systemic disease, constitutes the vast majority of cutaneous HD cases and as expected carries a worse prognosis.
• Secondary cutaneous HD usually presents with the rapid appearance of multiple, disseminated papulonodules and plaques, often on the trunk (Fig. 99.6), along with locations distal to affected lymph nodes.
Angioimmunoblastic T-Cell Lymphoma (AITL)
Lymphomatoid Granulomatosis (LYG)
• Cutaneous lesions are present in ~25–50% of patients, usually ranging from nodules to ulcerated plaques (Fig. 99.7); rarely an exanthematous eruption develops.

Fig. 99.7 Lymphomatoid granulomatosis. Ulcerated violaceous plaque in the popliteal fossa. Courtesy, Jean L. Bolognia, MD.
• Typically follows an aggressive, fatal course with a 5-year mortality rate of 60–90%.
• Rx: rituximab, multidrug chemotherapy, or perhaps interferon-α in earlier stage disease.
For further information see Ch. 121. From Dermatology, Third Edition.