47 Other Autoimmune CNS Demyelinating Disorders
Neuromyelitis Optica / Devic Disease
Diagnosis
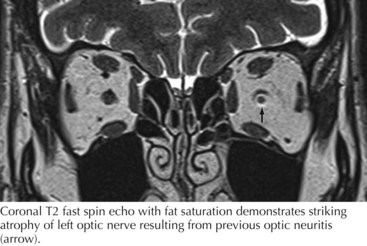
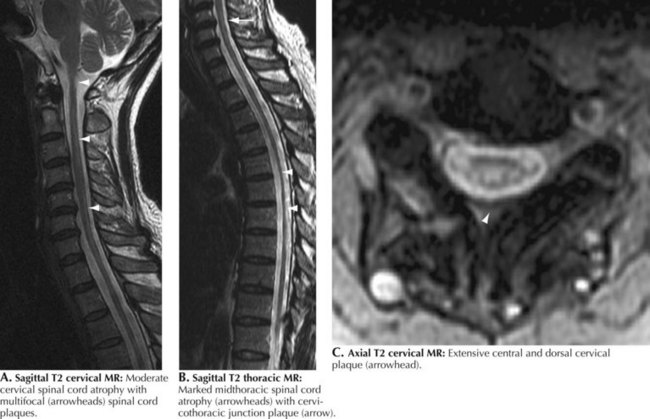
The diagnosis of NMO, rather than MS, in a patient with a history of ON (Fig. 47-1) and myelitis is largely dependent on documentation of longitudinally extensive spinal cord lesions (more than three spinal segments). Such extensive intramedullary spinal cord lesions are unique to NMO in contrast to the very short segment MRI findings in MS (Fig. 47-2).
Acute Disseminated Encephalomyelitis
Diagnostic Approach
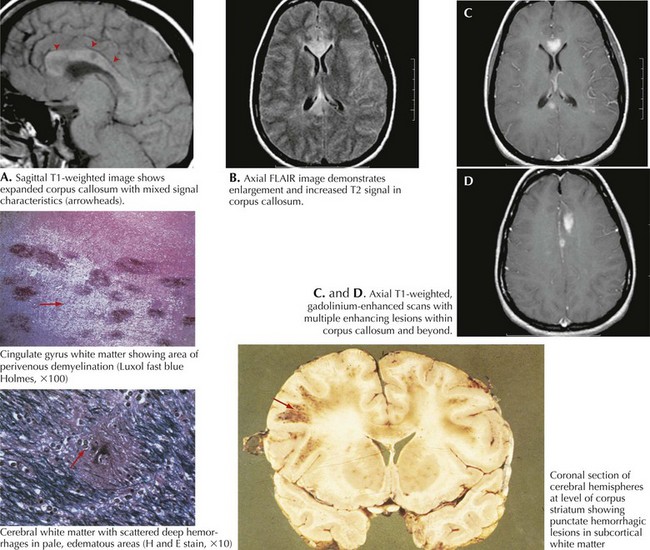
MRI is the primary diagnostic methodology. Commonly one sees multifocal asymmetric gadolinium-enhancing lesions throughout the brain and spinal cord (Fig. 47-3). Typically these lesions have varied imaging patterns, including nodular, gyral, amorphous, spotty, and ringlike shapes. ADEM patients typically have MRI abnormalities seen at the cortical gray and subcortical white matter interface. This contrasts significantly with MS, where the periventricular white matter is most commonly involved.
Differential Diagnosis
This includes acute MS, various acute aseptic meningoencephalitides, vasculitides, and very rare metabolic leukoencephalopathies, such as Schilder disease or Leigh syndrome. Cerebral biopsy is often necessary to confirm an ADEM diagnosis, especially in adults and atypical cases. Perivenous mononuclear cell infiltration associated with demyelination within the cellular cuff is the typical finding in patients with ADEM (Fig. 47-2).
Acute Hemorrhagic Leukoencephalopathy
Cree B. Neuromyelitis Optica: Diagnosis, pathogenesis, and treatment. Current Neurology and Neuroscience Reports. 2008;8:427-433. Excellent overview of the immunologic aspects of this disorder
Dale RC. Acute disseminated encephalomyelitis. Semin Pediatr Infect Dis. 2003;14:90-95.
Giovannoni G. To test or not to test NMO-IgG and optic neuritis. Neurology. 2008;70:2192-2193. A fine “state of the art” overview
Jacob A, Weinshenker BG, Violich BS, et al. Treatment of neuromyelitis optica with rituximab: retrospective analysis of 25 patients. Arch Neurol. 2008;65:1443-1448.
Lennon VA, Wingerchuk DM, Kryzer TJ, et al. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet. 2004;364:2106-2112. The original report defining the presence of this specific antibody
Matiello M, Lennon VA, Jacob A, et al. NMO-IgG predicts the outcome of recurrent optic neuritis. Neurology. 2008;70:2197-2200.
Roemer SF, Parisi JE, Lennon VA, et al. Pattern-specific loss of aquaporin-4 immunoreactivity distinguishes neuromyelitis optica from multiple sclerosis. Brain. 2007;130:1194-1205.
Rust RS. Multiple sclerosis, acute disseminated encephalomyelitis, and related conditions. Semin Pediatr Neurol. 2000;7:66-90.
Tenembaum S, Chamoles N, Fejerman N. Acute disseminated encephalomyelitis: a long-term follow-up study of 84 pediatric patients. Neurology. 2002 Oct 22;59(8):1224-1231.
Waters P, Jarius S, Littleton E, Leite MI, Jacob S, Gray B, Geraldes R, Vale T, Jacob A, Palace J, Maxwell S, Beeson D, Vincent A. Aquaporin-4 antibodies in neuromyelitis optica and longitudinally extensive transverse myelitis. Arch Neurol. 2008 Jul;65(7):913-919.
Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG. Revised diagnostic criteria for neuromyelitis optica. Neurology. 2006;66:1485-1489.
Wingerchuk DM, Pittock SJ, Lucchinetti CF, Lennon VA, Weinshenker BG. A secondary progressive clinical course is uncommon in neuromyelitis optica. Neurology. 2007;68:603-605.