Chapter 553 Other Abnormalities of Arginine Vasopressin Metabolism and Action
Hyponatremia (serum sodium <130 mEq/L) in children is usually associated with severe systemic disorders and is most often due to intravascular volume depletion, excessive salt loss, or hypotonic fluid overload, especially in infants (Chapter 52). The syndrome of inappropriate antidiuretic hormone secretion (SIADH) is an uncommon cause of hyponatremia in children.
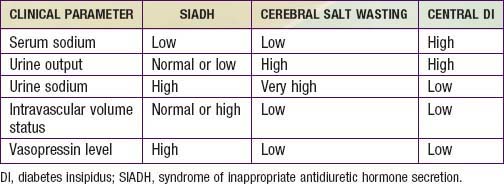
The initial approach to the patient with hyponatremia begins with determination of the volume status. A careful review of the patient’s history, physical examination, including changes in weight, and vital signs helps determine whether the patient is hypovolemic or hypervolemic. Supportive evidence includes laboratory data such as serum electrolytes, blood urea nitrogen, creatinine, uric acid, urine sodium, specific gravity, and osmolality (Chapter 52.3; Tables 553-1 and 553-2).
Table 553-1 DIFFERENTIAL DIAGNOSIS OF HYPONATREMIA
| DISORDER | INTRAVASCULAR VOLUME STATUS | URINE SODIUM |
|---|---|---|
| Systemic dehydration | Low | Low |
| Decreased effective plasma volume | Low | Low |
| Primary salt loss (nonrenal) | Low | Low |
| Primary salt loss (renal) | Low | High |
| SIADH | High | High |
| Cerebral salt wasting | Low | Very high |
| Decreased free water clearance | Normal or high | Normal or high |
| Primary polydipsia | Normal or high | Normal |
| Runner’s hyponatremia | Low | Low |
| NSIAD | High | High |
| Pseudohyponatremia | Normal | Normal |
| Factitious hyponatremia | Normal | Normal |
NSIAD, nephrogenic syndrome of inappropriate antidiuresis; SIADH, syndrome of inappropriate antidiuretic hormone secretion.
Table 553-2 CLINICAL PARAMETERS TO DISTINGUISH AMONG SIADH, CEREBRAL SALT WASTING, AND CENTRAL DIABETES INSIPIDUS
Causes of Hyponatremia
Syndrome of Inappropriate Antidiuretic Hormone Secretion
SIADH is characterized by hyponatremia, an inappropriately concentrated urine (>100 mOsm/kg), normal or slightly elevated plasma volume, normal-to-high urine sodium, and low serum uric acid. SIADH is uncommon in children, and most cases result from excessive administration of vasopressin in the treatment of central diabetes insipidus. It can also occur with encephalitis, brain tumors, head trauma, psychiatric disease, prolonged nausea, pneumonia, tuberculous meningitis, and AIDS and in the postictal phase following generalized seizures. SIADH is the cause of the hyponatremic second phase of the triphasic response seen after hypothalamic-pituitary surgery (Chapter 552). It is found in up to 35% of patients 1 wk after surgery and can result from retrograde neuronal degeneration with cell death and vasopressin release. Common drugs that have been shown to increase vasopressin secretion or mimic vasopressin action, resulting in hyponatremia, include oxcarbazepine, carbamazepine, oxcarbazepine, chlorpropamide, vinblastine, vincristine, and tricyclic antidepressants.
Pseudohyponatremia and Other Causes of Hyponatremia
Pseudohyponatremia can result from hypertriglyceridemia (Chapter 52). Elevated lipid levels result in a relative decrease in serum water content. As electrolytes are dissolved in the aqueous phase of the serum, they appear low when expressed as a fraction of the total serum volume. As a fraction of serum water, however, electrolyte content is normal. Modern laboratory methods that measure sodium concentration directly, independent of sample volume, do not cause this anomaly. Factitious hyponatremia can result from obtaining a blood sample proximal to the site of intravenous hypotonic fluid infusion.
Albanese A, Hindmarsh P, Stanhope R. Management of hyponatremia in patients with acute cerebral insults. Arch Dis Child. 2001;85:246-251.
Almond CS, Shin AY, Fortescue EB, et al. Hyponatremia among runners in the Boston Marathon. N Engl J Med. 2005;352:1550-1556.
Feldman BJ, Rosenthal SM, Vargas GA, et al. Nephrogenic syndrome of inappropriate antidiuresis. N Engl J Med. 2005;352:1884-1890.
Goldsmith SR. Treatment options for hyponatremia in heart failure. Heart Fail Rev. 2009;14:65-73.
Huang EA, Feldman BJ, Schwartz ID, et al. Oral urea for the treatment of chronic syndrome of inappropriate antidiuresis in children. J Pediatr. 2006;148:128-131.
Muglia LJ, Majzoub JA. Disorders of the posterior pituitary. In Sperling MA, editor: Pediatric endocrinology, ed 2, Philadelphia: WB Saunders, 2002.
Sterns RH, Silver SM. Cerebral salt wasting versus SIADH: what difference? J Am Soc Nephrol. 2008;19:194-196.






