CHAPTER 56 Osteotomy for Extra-articular Malunion of the Distal Radius
Distal radius fractures, first described in the 18th century by Petit1 and Pouteau2 commonly account for 10% of all fractures3 and 72% of all forearm fractures.4 For most authors, the most common complication of distal radius fractures is malunion, with a prevalence that ranges from 5% to 70% of all distal radius fractures, depending on the articles reviewed.5–12
Etiology and Pathophysiology
Approximately 25% of distal radius fractures treated by closed means heal with deformities that exceed general parameters of acceptance (dorsal tilt of 20 degrees in the sagittal plane and 10 degrees in the coronal plane, <10 degrees of rotation, <2 mm radial shortening, and <2 mm intra-articular step-off).8,9,11,13–16 When these fractures are treated by surgical means, however, regardless of the stabilization method employed, the incidence rate of malunion decreases to 10% or less.16,17 As a result, almost 80% of corrective osteotomies for malunion of the distal radius are done after failed closed treatment, and the remaining 20% are done after failed osteosynthesis, usually procedures done with minimally invasive techniques, such as external fixators or percutaneous Kirschner wires (K-wires).5,8,9,11,14,15,18–21
Diagnosis, Indications, and Timing
The need for surgical correction is multifactorial. Wrist deformity after fracture, even when exceeding the previously mentioned parameters of acceptance, may or may not produce symptoms. Differentiating symptomatic from asymptomatic malunion is paramount to decide whether treatment is necessary. Adequate, painless wrist function can be expected despite radiographic evidence of deformity, shortening, and degenerative changes. By necessity, the surgical decision is based on limitation of joint motion, grip strength, level of pain, and degree of cosmetic deformity. The intensity of these symptoms and their relative impact on activities of daily living, as correlated with radiocarpal radiographic findings, help define deformity tolerance and indications for corrective surgery.5,7,8,16,22
Pain
A malunited radius fracture may be a source of pain for various and often overlapping reasons, each of which must be assessed carefully because each sheds relevance in the selection of treatment. Intra-articular incongruence, be it at the radiocarpal joint or DRUJ, can produce early and often incapacitating pain.7,23,24 Loss of radial length can result in ulnocarpal abutment and may be a source of ulnar-sided wrist pain. Depending on the integrity of the distal radioulnar ligaments (volar and dorsal) of the triangular fibrocartilage complex, the abutment pain may be associated with limited forearm rotation (ligaments intact) or an unstable DRUJ (ligaments disrupted).25–27 A significant dorsal deformity (>20 to 30 degrees in the sagittal plane) displaces the proximal carpal row dorsally and overloads the articular cartilage in this reduced surface area (Fig. 56-1). Not only is this a common source of pain, but it also has been considered a prearthritic condition.28,29
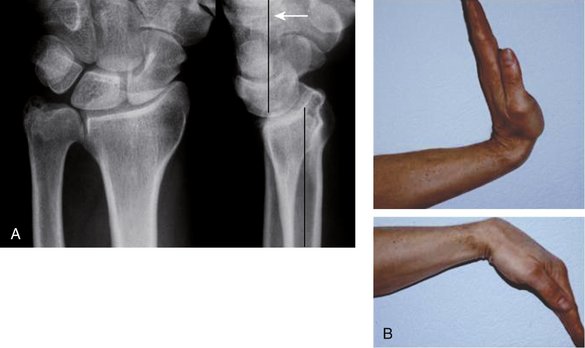
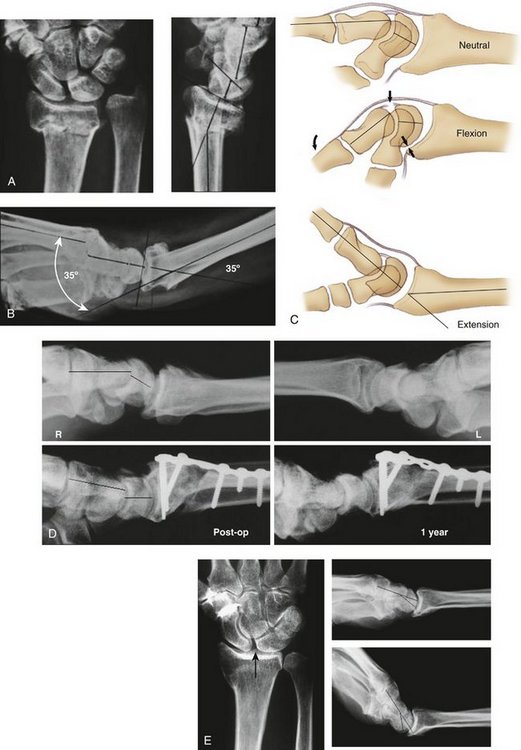
FIGURE 56-1 A, Malunited Pouteau-Colles fracture with severe dorsal tilt of the joint surface. Notice dorsal subluxation of the carpus without intercarpal malalignment. B, Dorsally displaced flexion-extension arc of motion.
Capsular contractures and synovitis that result from positional abnormalities within the carpal rows are responsible for painful limitation of wrist flexion. At the midcarpal articulation, a dorsally malunited fracture can result in several distinct problems and compensatory deformities: (1) an adaptive (type I) dorsal intercalated segment instability (DISI), in which the midcarpal flexion is lax and fully correctable by radial osteotomy (Fig. 56-2A-D)30,31; (2) a fixed (type II) DISI malalignment, which does not improve after radial osteotomy and may represent a chronic stage of scapholunate instability, not diagnosed at the time of injury, or the stiffening with time of a previously lax deformity (Fig. 56-2E)9,30,32; and (3) the already mentioned dorsal subluxation of the entire carpus.25 Differentiating DISI types I and II can be done with a lateral x-ray of the wrist taken in the same amount of extension as the dorsal angulation of the malunited distal radius (see Fig. 56-2).30,32
Grip Strength
Another important parameter when deciding whether a corrective osteotomy is indicated is the loss of grip strength. Grip strength, when compared with the uninjured side or with cohorts of the healthy general population, often represents the degree of deformity and the associated functional impairment.33 Although there is no generally established quantity of weakness to warrant an osteotomy, it is thought that a grip of at least 30 kg is needed for most activities of daily living.34 In addition to the loss of strength secondary to pain, the spatial angulations that result from malunion alter the flexor and extensor tendinous vectors of traction.7 The change in position of the wrist’s center of rotation results in diminished efficiency of the tendon lever arms.
Range of Motion
The third evaluation criterion for corrective osteotomy is limitation of joint motion. Malunions with intra-articular incongruity greater than 2 mm have considerable limitations in range of motion.23,24 It is common to have less than 40 degrees in extension or supination or both in a Smith fracture and flexion of only 30 degrees in a Colles’ fracture.32 Limited motion may be severe enough to indicate a corrective osteotomy alone, despite adequate grip strength and absence of pain. When combined with pain and weakness, decreased function significantly limits activities of daily living.
Cosmetic Appearance
For certain patients, malunion deformity may be so obvious that esthetic considerations may incline the surgeon toward correction despite nonsuggestive functional and radiographic parameters. An isolated deformity does not justify corrective osteotomy.7,16,22 Regardless, it is rare for such deformities to occur in the absence of symptoms.
Radiographic Findings
My colleagues and I do not believe in the use of fixed radiographic angles for determining if correction is needed. Certain parameters that are associated with rapid degenerative changes, such as an articular incongruence greater than 2 mm or the prearthritic deformity of a dorsal defect greater than 20 to 30 degrees, are considered formal surgical indications, independent of patient symptoms, especially in a young patient. Lanz and Kron35 suggest comparisons of the affected wrist with statistical radiographic standards to quantify amount of deformity.3,15,22,36 In contrast, a comparison tailored to the patient’s particular anatomy can be obtained with radiographs of the uninjured wrist, as suggested in an earlier work.7
Timing
Although correction of extra-articular deformity can be safely delayed until the soft tissues offer an ideal surgical environment, and maximal residual function of the wrist has been regained, intra-articular deformity should be dealt with as soon as possible, before irreversible articular damage occurs. Jupiter and Ring37 compared the results of early and late osteotomies in two similar cohorts and concluded that early correction provided easier radial and DRUJ realignment because of the absence of soft tissue and capsular contractures. The need for structural iliac crest bone graft is diminished because the local nascent callus material can be used to fill defects. Jupiter and Ring37 concluded that although functional results are similar in both groups, early surgery resulted in considerably less total disability and earlier return to work.
Surgical Correction of Extra-articular Dorsal Deformity: Management Options
Dorsal Approach
Preoperative Planning
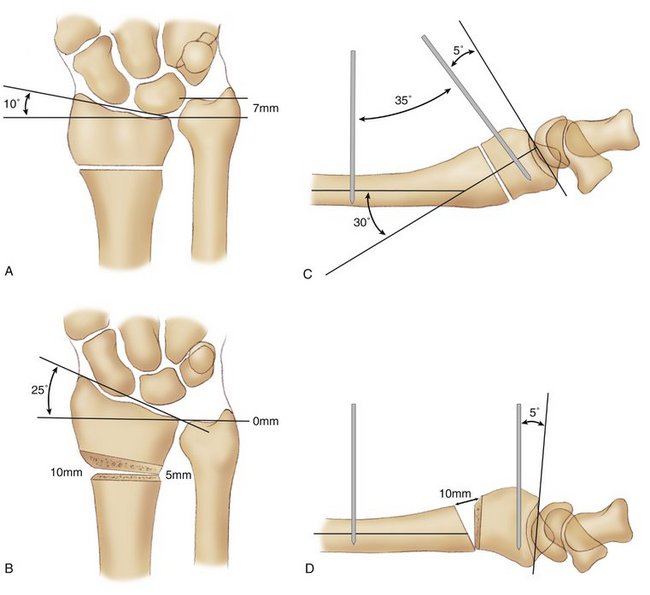
A careful preoperative plan incorporating K-wires that mark the angles of correction is characteristic of this technique (Fig. 56-3). These angles are mandatory to simplify the procedure, guarantee an accurate angular correction, and diminish the need for intraoperative image control. Prerequisites for this planning process are standard radiographs of the injured and uninjured side. When superimposed, these images allow localization of the osteotomy site and measurement of angular deformity in the two orthogonal projections: the lateral view (sagittal plane) and the anteroposterior view (frontal plane).
Rotational deformity is more accurately measured by superimposing tracings of symmetrical computed tomograms of both forearms. The proximal cuts of the scan should include the bicipital tuberosity, and the distal cuts should be at the level of Lister’s tubercle. The “radial torsion angle” is defined as the angle between the proximal and distal reference axes.38 The difference between the radial torsion angles for the injured and contralateral side represents the true bony rotational malalignment.
The osteotomy entails a wedge opening on the dorsal and radial side, with a volar and ulnar hinge. Two K-wires are planned for intraoperative monitoring and inserted precisely in the sagittal plane, converging at the intended angle of correction. The osteotomized distal fragment is outlined and tilted around the respective hinge at the predetermined correction angles. The resulting length is evaluated and checked with respect to the distal ulna and adjusted if necessary. For a true hinge or wedge (unicortical osteotomy), its height at the ulnopalmar corner is zero and at the ulnodorsal corner equals the dorsal gap from the lateral projection. The radiopalmar corner is taken from the plan converting the arc of correction in millimeters. The radiodorsal height is the sum of the two aforementioned measurements. For a trapezoidal-shaped defect (bicortical osteotomy), the dimensions are calculated in the same manner, in addition to its depth, which is given by the sagittal and frontal diameter of the radius at the level of the cut.
Technique
To ensure proper orientation and location of the osteotomy, a fine K-wire is inserted through the dorsal capsule into the radiocarpal joint along the articular surface of the radius, indicating the sagittal plane of the joint. If a single angular correction is planned, the osteotomy cut has to be exactly parallel to the joint surface in the sagittal plane. If correction of radial inclination and malrotation is needed, the cut has to be aligned perpendicular to the distal fragment in both planes (i.e., in the anteroposterior view as well). Otherwise, rotation along a nonorthogonal interface results in secondary angular malpositioning. According to the operative plan, two threaded 2.5-mm K-wires are inserted subtending the angle of correction on both sides of the future osteotomy (Fig. 56-4). These K-wires not only serve to guide intraoperative correction, but also to manipulate and maintain the distal fragment in the correct position. A small external fixator may be used temporarily to maintain correction, if needed.
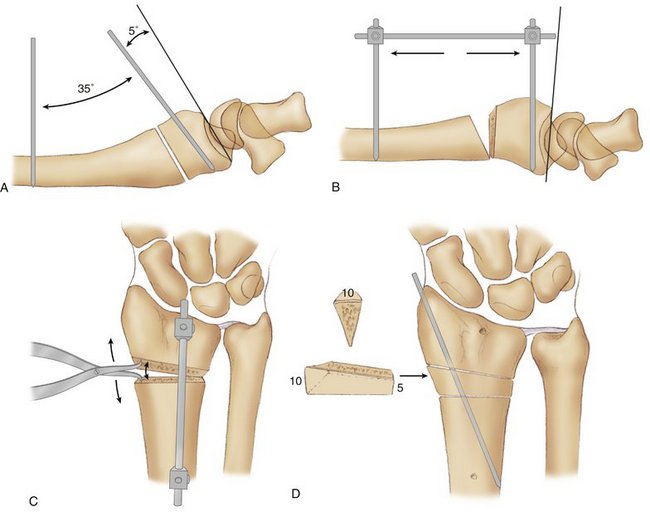
FIGURE 56-4 Osteotomy technique—dorsal approach. A, Threaded wires subtend the angle of correction. The osteotomy is parallel to the joint surface in the sagittal plane. Note the fine Kirschner wire introduced into the radiocarpal joint. B and C, The osteotomy is opened dorsally and radially with a small spreader clamp. A fixator bar maintains the correction. D, An iliac graft shaped to conform to the defect is inserted, and one oblique Kirschner wire is driven through the radial styloid and graft into the radial metaphysis. The fixator is removed, and definitive plate fixation is carried out.
Protecting the volar soft tissues, the osteotomy is performed with the oscillating saw parallel to the distal K-wire, taking care not to osteotomize completely the volar cortex. The osteotomy is opened dorsally and radially by manipulating the wrist into flexion and with the assistance of a small laminar spreader. The osteotomy is opened until both K-wires are parallel in the sagittal plane. Complete tenotomy of the brachioradialis or Z-lengthening is recommended to facilitate radial lengthening. Next, a corticocancellous strut graft is harvested from the iliac crest, shaped according to the resulting osteotomy defect, incorporated with the cortical portion oriented dorsally, and temporarily fixed with K-wires. If rotational correction is needed, one or two K-wires are inserted through the graft into the proximal fragment to secure the correct axial alignment. Then the distal fragment can be rotated (usually pronated) on the graft to the desired position. The amount of rotational correction is monitored with the two K-wires in the sagittal plane.
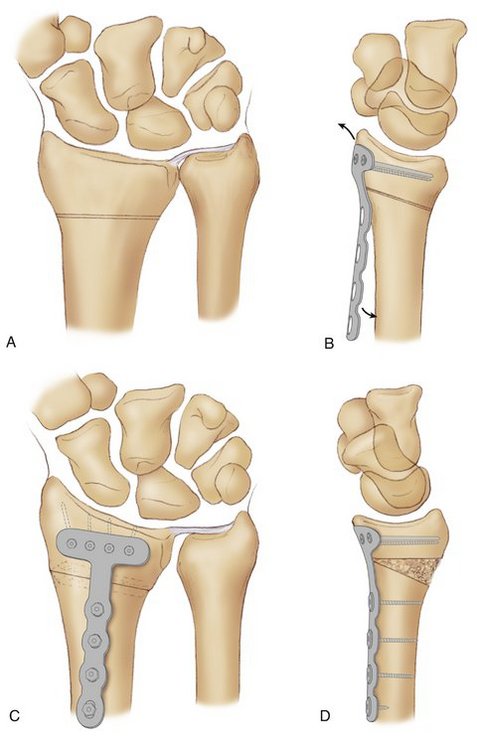
Various methods of stable fixation are available. In our practice, a 2.7-mm condylar plate or the use of two 2.4-mm locking plates are preferred for the following reasons: (1) The 2.7-mm condylar plate can be completely covered by the fourth compartment and does not interfere with the extensor pollicis longus or the wrist extensors, diminishing the risk of attrition tendinitis; (2) its fixed-angle component minimizes loss of correction by fragment settling; (3) by virtue of the low profile of the plate, extensor tendon irritation is uncommon, and removal of hardware is seldom necessary; and (4) stability of the construct can be augmented by inserting a separate oblique lag screw across the osteotomy. If the 2.4-mm distal radius plates are used, one is applied on the radial border between the wrist extensors and the first dorsal compartment, and the other is applied dorsoulnarly under the fourth compartment (Fig. 56-5).
If fixed-angle devices are used, morcellized cancellous grafts may be used because the chances of loss of correction are minimized, especially if the distal locking screws are placed in the subchondral area of the epiphysis.20 With increasing stability of the construct, an earlier return of unrestricted active wrist motion can be offered. During wound closure, the extensor pollicis longus is protected from the plate by the interposition of an extensor retinacular flap or returned to its groove, if Lister’s tubercle has been preserved. Deep suction drainage of the wound is recommended for 24 hours postoperatively.
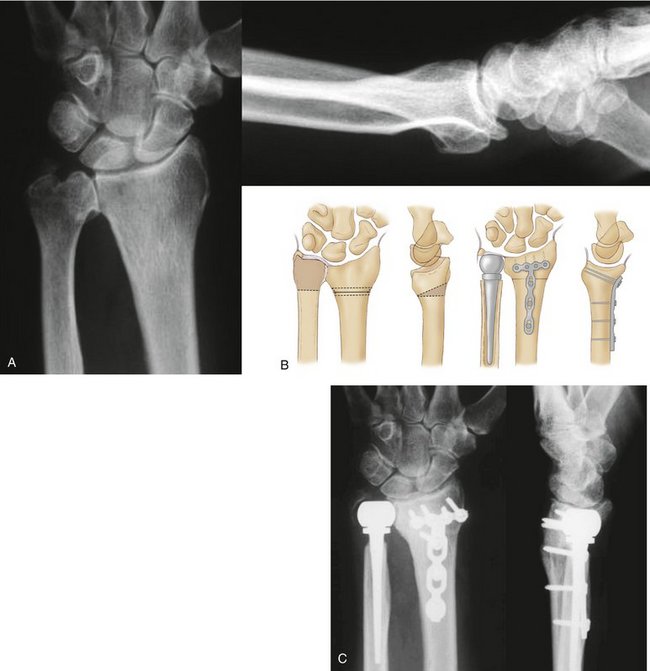
Volar Approach
The volar approach, originally described by Lanz and colleagues,35,39 consists of performing the dorsal correction through a volar approach, and internally fixing the distal radius with an anatomically congruent, fixed-angle volar plate. This method, although technically challenging, has the undeniable advantage of an automatic correction of deformity by the correct placement of an anatomically congruent volar plate to the distal fragment (Fig. 56-6). There is no risk of extensor tendinitis, provided that screws do not protrude through the dorsal cortex,34 and the approach permits an “en-bloc” manipulation of the osteotomized fragment.
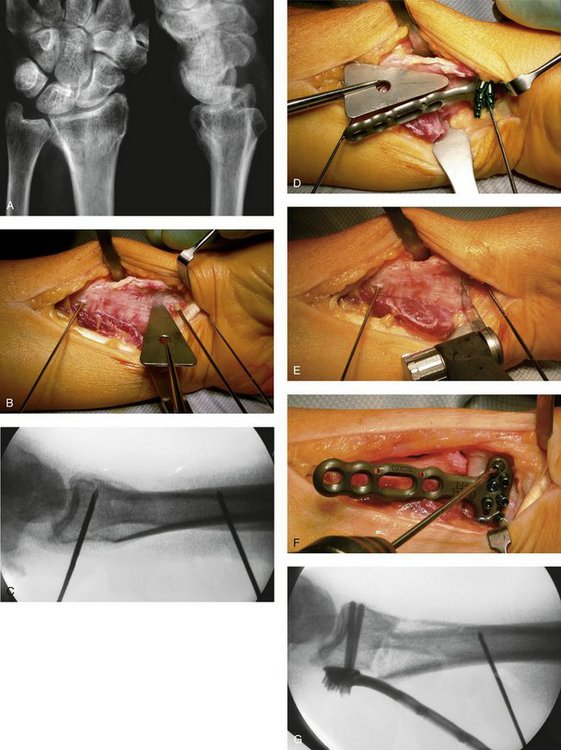
Technique
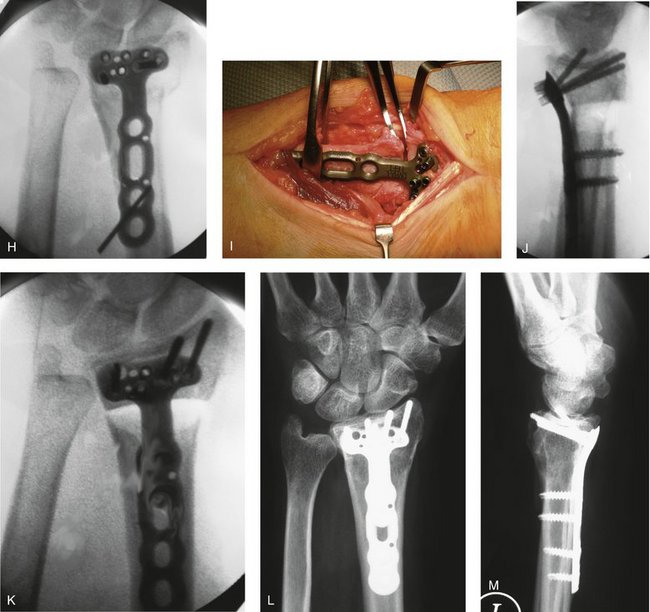
The distal part of the Henry approach between the flexor carpi radialis and radial artery is used (Fig. 56-7). After detachment of the pronator quadratus, the lateral border of the radius is exposed. This exposure is facilitated with detachment or a Z-tenotomy of the brachioradialis and by opening the floor of the first dorsal compartment.40 At this point, a flat Hohmann retractor should be carefully placed under the extensor tendons (see Fig. 56-7B). Two 2-mm K-wires subtending the correction angle are driven into the shaft and distal fragment. The distal K-wire should be parallel to the joint surface in the sagittal plane (see Fig. 56-7C). Before the osteotomy cut, the distal component of the plate is fixed temporarily to the distal radius (see Fig. 56-7D).
The drill holes for the most ulnar and radial fixed-angle pegs of the proximal row of holes in the DVR plate are prepared at this point. The plate is removed, and the osteotomy cut is performed at the old fracture site from volar dorsal parallel to the distal K-wire (see Fig. 56-7E). As described for the dorsal approach, the same principles for preoperative planning, and making the osteotomy cut perpendicular to the axis of the radius in the anteroposterior plane and parallel to the joint surface in the sagittal plane, apply. After completion of the osteotomy, the distal fragment is supinated and extended while the shaft is maintained pronated. This maneuver facilitates dorsal exposure to visualize and resect the dorsal callus and periosteum, diminishing the danger of damaging the extensor tendons. A dorsal release also is imperative to permit ease of correction and restoration of radial length. Next the plate is fixed with subchondral fixed-angle pegs and screws to the distal fragment (see Fig. 56-7F-H).
Correction in all three planes occurs simultaneously as the proximal part of the plate is progressively reduced to the radial shaft with a bone clamp. A laminar spreader may be used simultaneously to open the dorsal wedge and help in restoring length and performing frontal plane corrections (see Fig. 56-7I). After fluoroscopic verification of correction, the plate is fixed to the radial shaft (see Fig. 56-7J and K).
The intrinsic stability of these fixed-angle devices, especially when distal pegs are placed subchondrally, guarantees the maintenance of length. These devices have become the implant of choice for fixation of osteoporotic bone and have allowed us to extend the indications of radial osteotomy in elderly patients. For the same reasons, there is no need of structural corticocancellous bone grafts, and the gap may be filled with morcellized autologous grafts or even with bone substitutes. At 1 year, complete radiographic bone remodeling of the bone defect may be observed (see Fig. 56-7L and M).
Volar Closing Wedge Osteotomies
Because most of the failures of reconstructive surgery after distal radius fracture are due to persistent symptoms arising from the DRUJ, some authors have advocated distal ulnar resection at the time of the corrective radial osteotomy. Posner and Ambrose41 described a closing wedge osteotomy associated with a Darrach procedure, fixed with K-wires and protected with plaster immobilization. This approach has clear advantages for malunions in elderly patients with osteoporotic bone and degenerative changes of the DRUJ or associated intra-articular sigmoid notch involvement in the radius malunion. A similar technique was proposed by Viso and colleagues,42 whereas other authors11,12 recommend an ulnar shortening osteotomy, if the DRUJ shows no degenerative changes. If degenerative changes of the DRUJ are present, I prefer a closing wedge palmar osteotomy and primary prosthetic ulnar head replacement with restoration of a 0-mm ulnar variance.43,44 I no longer resect the distal ulna (Bowers or Darrach) in these situations in an effort to maintain the integrity of the DRUJ, the load transmission of the ulnar side of the carpus, and the kinematics of forearm rotation (Fig. 56-8).
Surgical Correction of Metaphyseal Volar Deformity (Malunited Smith-Goyrand Fractures)
The classic symptoms of malunion following volarly displaced fractures include decreased wrist extension, ulnar deviation, and supination. Because of the tendency for Smith’s fractures to heal with a pronation deformity of the distal radius, the lack of supination may be especially troublesome for the patient. Volarly angulated malunions following Smith’s fractures require a palmar open wedge osteotomy. A straight volar incision between the flexor carpi radialis tendon and the radial artery is performed. The pronator quadratus muscle is detached radially, and the flexor pollicis longus muscle is mobilized from the radial shaft. The malunion is approached subperiosteally by dissecting the pronator quadratus muscle to the ulnar side, and the soft tissues are protected with Hohmann retractors. The palmar opening wedge osteotomy, grafting, and plating are done in a “reversed” fashion—as in Colles’ deformity, but from the volar side (Fig. 56-9).
Care must be taken not to overcorrect the physiological palmar tilt of 10 degrees when manipulating the distal fragment into dorsiflexion. The application of a volar buttressing T-plate automatically derotates the pronated distal fragment by virtue of the flat surface of the plate.3,21,45,46 Plate fixation is strongly recommended on the volar side because practically all malunited Smith’s fractures have a pronation deformity of the distal fragment and an apparent dorsal subluxation of the distal ulna. Most available volar radial plates have been procontoured to fit the anatomical concavity of the distal radial volar surface, so that now overcorrection into a dorsal tilt is a rare complication. Care has to be taken with the screw length; attrition tendinitis and tendon ruptures may occur with the screw protruding dorsally. Dorsiflexion of the distal fragment and derotation and lengthening reorient the sigmoid notch of the radius with respect to the head of the ulna, restoring articular congruity of the radioulnar joint.
Discussion
In a meta-analysis of the results of almost 600 corrective osteotomies published in the French and English literature, Gonzalez del Pino and associates34 noted that overall results depended fundamentally on the quality and exactness of the correction obtained. Approximately 40% of the cases require a second or third surgical procedure for implant extraction (most cases), treatment of complications, or correction of residual deformity or to address problems in the DRUJ. Obtaining an adequate correction is not always possible. Good and excellent results were obtained in 72% of the cases, fair results were obtained in 15% to 20%, and poor results were obtained in the remaining 10% to 15%. Given the multiple techniques employed, and the variation in deformity, patient selection, and methods of outcome evaluation, these figures serve as rough estimates of a general trend.
Despite the fact that corrective osteotomy for a malunited distal radius has become a standardized surgical procedure, and that advances in diagnosis, instrumentation, and surgical technique continue to evolve, it remains obvious that the best treatment is prevention (immediate surgical fracture stabilization). Major advances include the use of fixed-angle plates that allow rigid fixation of the osteotomy even in osteoporotic bone, obviating the need for structural bone grafting. Prosthetic replacement of the ulnar head provides a sound alternative to DRUJ salvage and rescue of postresection radioulnar impingement.
1. Petit J. L’Art de Guerir les Maladies de l’Os. Paris: d’Houry; 1705.
2. Pouteau C. Oeuvres posthumes de M Pouteau: Memoire, contenant quelques reflexions sur quelques fractures de l’avant-bras sur les luxations incompletes du poignet et sur le diastasis. Paris: Pierres; 1783.
3. Prommersberger KJ, Van Schoonhoven J, Laubach S, et al. Corrective osteotomy for malunited, palmarly displaced fractures of the distal radius. Eur J Trauma. 2001;27:16-24.
4. Alffram P, Bauer G. Epidemiology of fractures of the forearm: A biomechanical investigation of bone strength. J Bone Joint Surg Am. 1962;44:105-114.
5. Brown JN, Bell MJ. Distal radial osteotomy for malunion of wrist fractures in young patients. J Hand Surg [Br]. 1994;19:589-593.
6. Hunt TR, Hasting H2nd, Graham TJ. A systematic approach to handling the distal radio-ulnar joint in cases of malunited distal radius fractures. Hand Clin. 1998;14:239-249.
7. Jupiter JB, Fernandez DL. Complications following distal radial fractures. J Bone Joint Surg Am. 2001;83:1244-1265.
8. Ladd AL, Huene DS. Reconstructive osteotomy for malunion of the distal radius. Clin Orthop. 1996;327:158-171.
9. McGrory BJ, Amadio PC. Malunion of the distal radius. In: Cooney WP, Linscheid RL, Dobyns JH, editors. The Wrist: Diagnosis and Operative Treatment. St. Louis: Mosby, 1998.
10. McKay SD, MacDermid JC, Roth JH, et al. Assessment of complications of distal radius fractures and development of a complications checklist. J Hand Surg [Am]. 2001;26:916-922.
11. Sennwald G, Fischer W, Stahelin A. Le cal vicieux du radius distal et son traitement: a propos de 122 radii. Int Orthop. 1992;16:45-51.
12. Voche P, Merle M, Dautel G. Les cals vicieux extra-articulaires du radius distal: evaluation et techniques de correction. Rev Chir Orthop Reparatrice Appar Mot. 2001;87:263-275.
13. Fourrier P, Bardy A, Roche G, et al. Approche d’une definition du cal vicieux du poignet. Int Orthop. 1981;4:299-305.
14. Hove LM, Mölster AO. Surgery for posttraumatic wrist deformity: Radial osteotomy and/or ulnar shortening in 16 Colles’ fractures. Acta Orthop Scand. 1884;65:434-438.
15. Prommersberger KJ, van Schoonhoven J, Lanz UB. Outcome after corrective osteotomy for malunited fractures of the distal end of the radius. J Hand Surg [Br]. 2002;27:55-60.
16. Wright T. Osteotomy for distal radius malunion. Tech Hand Upper Extrem Surg. 2000;4:222-235.
17. Treatment of distal intra-articular malunions. In: Saffar P, Cooney WP, editors. Fractures of the Distal Radius. London: Martin Dunitz, 1995.
18. Linder L, Stattin J. Malunited fractures of the distal radius with volar angulation: corrective osteotomy in 6 cases using the volar approach. Acta Orthop Scand. 1996;67:179-181.
19. Oskam J, Bongers KM, Karthaus AJ, et al. Corrective osteotomy for malunion of the distal radius: the effect of concomitant ulnar shortening osteotomy. Arch Orthop Trauma Surg. 1996;115:219-222.
20. Ring D, Roberge C, Morgan T, et al. Osteotomy for malunited fractures of the distal radius: a comparison of structural and non-structural autogenous bone grafts. J Hand Surg [Am]. 2002;27:216-222.
21. Shea K, Fernandez DL, Jupiter JB, et al. Corrective osteotomy for malunited, volarly displaced fractures of the distal end of the radius. J Bone Joint Surg [Am]. 1997;79:1816-1826.
22. Prommersberger KJ, Lanz UB. Corrective osteotomy for malunited Colles’ fractures. Orthop Traumatol. 1998;6:75-87.
23. Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68:647-659.
24. Marx RG, Axelrod TS. Intraarticular osteotomy of distal radius malunions. Clin Orthop. 1996;327:152-157.
25. Adams BD. Effects of radial deformity on distal radioulnar joint mechanics. J Hand Surg [Am]. 1993;18:492-498.
26. Bronstein AJ, Trumble TE, Tencer AF. The effects of distal radius fracture malalignment on forearm rotation: a cadaveric study. J Hand Surg [Am]. 1997;22:258-262.
27. Kihara H, Palmer AK, Werner FW, et al. The effect of dorsally angulated distal radius fractures on distal radioulnar joint congruency and forearm rotation. J Hand Surg [Am]. 1996;21:40-47.
28. Pogue DJ, Viegas SF, Patterson RM, et al. Effects of distal radius fracture malunion on wrist joint mechanics. J Hand Surg [Am]. 1990;15:721-727.
29. Short WH, Palmer AK, Werner FW, et al. A biomechanical study of distal radial fractures. J Hand Surg [Am]. 1987;12:529-534.
30. Fernandez DL. Reconstructive procedures for malunions and traumatic arthritis. Orthop Clin North Am. 1993;24(2):341-364.
31. Psychoyios VN, Ring D, Roberge C, et al. Carpal alignment after corrective osteotomy for malunited fractures of the distal radius. J Hand Surg [Br]. 2000;25:38.
32. Park MJ, Cooney WP3rd, Hahn ME, et al. The effects of dorsally angulated distal radius fractures on carpal kinematics. J Hand Surg [Am]. 2002;27:223-232.
33. Torres M, Gonzalez del Pino J, Yánez J, et al. Estudio dinamometrico de la mano y el pulgar. Rev Ortop Traumatol. 1999;43:321-326.
34. Gonzalez del Pino J, Bartolomé del Valle E, Lopez Graña G, et al. Consolidaciones viciosas tras fracturas del extremo distal del radio: patogenia, indicaciones y técnicas quirúrgicas. Rev Ortop Traumatol. 2003;47(Suppl 1):55-69.
35. Lanz U, Kron W. Neue Technik zur Korrektur in Fehlstellung verheilter Radiusfrakturen. Hand Chir Mikrochir Plast Chir. 1976;8:203-206.
36. Kwasny O, Fuchs M, Schabus R. Opening wedge osteotomy for malunion of the distal radius with neuropathy: 13 cases followed for 6 (1-11) years. Acta Orthop Scand. 1994;65:207-208.
37. Jupiter JB, Ring D. A comparison of early and late reconstruction of malunited fractures of the distal end of the radius. J Bone Joint Surg Am. 1996;78:739-748.
38. Bindra RR, Cole RJ, Yamaguchi K, et al. Quantification of the radial torsion angle with computerized tomography in cadaver specimens. J Bone Joint Surg Am. 1997;79:833-837.
39. Prommersberger KJ, Moossavi S, Lanz U. Ergebnisse der Korrekturosteotomie fehlverheilter Extensionsfrakturen der Speiche an typischer Stelle. Handchir Mikrochir Plast Chir. 1999;31:234-240.
40. Orbay J, Indriago I, Badia A, et al. Corrective osteotomy of dorsally malunited fractures of the distal radius via the extended FCR approach. J Hand Surg [Br]. 2003;28(Suppl 1):2-3.
41. Posner MA, Ambrose L. Malunited Colles’ fractures: correction with a biplanar closing wedge osteotomy. J Hand Surg [Am]. 1991;16:1017-1026.
42. Viso R, Wegener EE, Freeland AE. Use of a closing wedge osteotomy to correct malunion of dorsally displaced extra-articular distal radius fractures. Orthopedics. 2000;23:721-724.
43. van Schoonhoven J, Fernandez DL, Bowers WH, et al. Salvage of failed resection arthroplasties of the distal radioulnar joint using a new ulnar head prosthesis. J Hand Surg [Am]. 2000;25:438-446.
44. Fernandez DL. Management of acute and chronic derangement of the distal radioulnar joint following radius fractures. In: Jakob RP, Fulford P, Horan F, editors. EFORT Instructional Course Lectures. J Bone Joint Surg Br; 1999:41-53.
45. Fernandez DL. Correction of post-traumatic wrist deformity in adults by osteotomy, bone-grafting, and internal fixation. J Bone Joint Surg Am. 1982;64:1164-1178.
46. Fernandez DL, Jupiter JB. Fractures of the Distal Radius: A Practical Approach to Management, 2nd ed. New York: Springer; 2002.