Chapter 187 Orthoses
Complication Prevention and Management
Spinal bracing encompasses a variety of time-honored techniques that provide external support to injured or diseased segments of the vertebral column. The practice of bracing is as old as medicine itself, having appeared throughout history in the medical and surgical writings of Hippocrates, Galen, Pare, Levacher, and Andry.1–4 In more modern times, Frankel et al.5 showed that bedrest and immobilization can be effective means of achieving bony fusion. The pressures of modern medicine, however, require early mobilization both to decrease hospital length of stay and to minimize medical complications.
Principles of Spinal Bracing
By definition, all orthoses are externally applied devices that apply indirect forces to the spine for correcting or preventing deformity, stabilization, unloading, and/or supportive effects (e.g., massage, warmth, psychological comfort).6 The most common element among these goals is motion restriction.
The Spine as a Column
The manner by which orthoses exert restrictive effects is perhaps best understood in terms of column mechanics. Several authors have described the spine as a complex variant of an ideal column with a fixed base and free upper end.2,7 As a theoretical structure, this “ideal” column is considered a homogeneous rod of constant composition, length, and cross-sectional area. Its behavior when loaded by a balanced axial force has been described mathematically by Euler’s relationship for long-segment column dynamics:
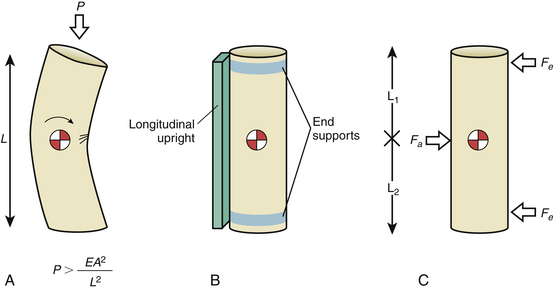
where P is the magnitude of the applied axial load, E is related to the modulus of elasticity of the column material, A is the cross-sectional area of the column, and L is the length8 (Fig. 187-1A). As the structure is progressively loaded, it initially shortens along its longitudinal axis. Once the axial load P exceeds a critical load specific for the column, failure occurs by elastic buckling.7 Methods for stabilizing or increasing the column axial load-bearing capacity involve altering one or more of three variables: column elasticity (E), cross-sectional area (A), or length (L).
Prototypical spinal orthoses consist of two end-fixation elements and a connecting longitudinal member (Fig. 187-1B). An example is the chairback, thoracolumbosacral orthosis (TLSO), which purchases the rib cage with a thoracic band and the hips with a pelvic band. Uprights interconnect the thoracic and pelvic bands.3 Sleeve-type orthoses, such as the clamshell TLSO (see later discussion), incorporate these elements into their circumferential design.1 In terms of column mechanics, braces add to the relative cross-sectional area and the total modulus of elasticity of the spine, thus creating a heterogeneous composite structure that shares the axial load.
Internal segmental fixation applies direct immobilization to spinal segments, while most spinal orthoses apply their forces at some distance from the spine. There is an inverse relationship between the thickness of the soft tissue separating the spine from the inner surface of the orthosis and the resulting effectiveness of immobilization. Conformation of the brace to the body helps to maintain the cylindrical body shell, thereby increasing the stability of the spine.9–12 Also, longer braces provide more stability than shorter ones do; therefore, the length-to-width ratio of the orthotic significantly affects efficacy (see Fig. 187-1A).
Orthoses may also apply balanced transverse forces in a three-point bending arrangement that resists bending forces and thus contributes to axial load bearing.1,8,13 The Jewett brace utilizes the aforementioned biomechanical advantage of a three-point bending force application produced by applying dorsal forces at the sternum and pubis in combination with a ventral force at the affected thoracic or lumbar vertebra.4,11 The long lever arms minimize the force required to produce a sufficient bending moment. Three-point bending also effectively divides the column functionally into two portions of smaller length, increasing the critical failure load of the whole column to that of each segment (Fig. 187-1C).
An underlying principle in long bone splinting is the immobilization of the fractured bone from one joint above to one joint below the site of injury. Extrapolating this concept to the axial skeleton, one may consider it to be composed of five segments, each of which may be considered a long bone (cranial, cervical, thoracic, lumbar, and sacropelvic) (see Figs. 187-1A and B). Therefore, one segment above and one segment below the unstable motion segment would be included in the brace.
Dynamic and Passive Control
All orthoses control spinal motion by a combination of dynamic and passive mechanisms. Dynamic control describes the significant role of intrinsic musculature in actively stabilizing the spine and is the major component in the action of most orthoses. It has been demonstrated experimentally that opposing muscular forces significantly stiffen the spinal column, increasing its load-bearing capacity.9 If isolated from its muscular support, the osseous and ligamentous spinal column holds only 2 kg of axial load before failure by buckling.2 In terms of a column model, muscular action directly affects the modulus of elasticity and relative cross-sectional area of the composite spinal column. Orthoses promote this muscular stabilization by tactile feedback that guides the patient to maintain proper positioning of the body. Pressure at the orthosis-skin contact site creates a reminder to maintain a safe position and limit unwanted gross body motion.4,13–16 The patient therefore is able to prevent undesirable motion of the spine by using only intrinsic muscular support guided by the orthosis. A stiffer, more securely worn appliance is more effective at limiting motion than is a flexible brace because of the heightened sensation of resistance that the stiffer appliance produces. Sypert and others have noted that the effectiveness of an appliance is directly related to the level of its discomfort.3,4 However, this discomfort may also contribute to higher levels of noncompliance.
Passive mechanisms for motion control are important in three-point bending mechanisms and are derived from intrinsic properties of the orthosis itself such as design, size, and material composition. The two common design elements of all orthoses are similar in principle to internal fixation constructs and include end-stabilizing elements (e.g., thoracic bands, pelvic bands) and longitudinal members or uprights that interconnect the end elements.1 Passive mechanisms apply reactive forces to the body that oppose forces resulting from physiologic movements of the head or trunk; viscoelastic forces of ligaments, discs, and muscles; and gravitational force.17 As summarized by White and Panjabi,8 passive mechanical strategies form the basis for most orthotic techniques and include spinal distraction, fluid compression, balanced transverse force application, and skeletal fixation. Most appliances use a combination of techniques for spinal motion control.
Distraction
Distracting the ends of a column is a useful means of correcting or preventing deformity. Its effectiveness depends on the efficiency of transmitting the distracting force directly to the column. Spinal distraction is a major strategy of internal fixation devices used for spine correction and stabilization. This is best illustrated by the Harrington apparatus.7 Distraction is also the technique that is used to reduce acutely unstable spine fractures with tong or halo traction. A braced column in distraction can be considered a composite of an externally applied distracting force plus the axial supporting properties of the original structure.
Distraction orthoses typically act on the head and thorax and cannot directly affect individual vertebral segments. Purchase of the head is either indirect, with pads located at the mandible and the occiput (conventional orthoses), or direct by means of skull pins (halo-skeletal fixation). Thoracic purchase is obtained at the sternum and rib cage through a combination of pads, straps, or vest attachment. The effectiveness of a distraction orthosis depends on the efficiency of force transmission to the vertebral segment of interest and the mechanical rigidity of the orthosis material itself.13 Inefficiency in transmitting external force to the spine has been termed “the transmitter problem” by White and Panjabi8 and represents the loss of energy that occurs when force is applied to “low stiffness, viscoelastic” structures such as overlying soft tissues, intervening normal joints, and ligaments. In the cervical area, distraction applied to the mandible is compromised by cushioning effects of soft tissue under the chin, the temporomandibular joint, cervical muscle tone, the C0-1 articulation, and each successive segmental articulation above the level at which the force is to have its effect (level of pathology). A more rigid brace with a tighter fit improves the efficiency of transmitting force by compressing intervening soft tissue.17 These factors paradoxically increase the risk of pressure injury to overlying soft tissues.18 Skeletal fixation improves the effectiveness of force transmission by directly purchasing the skull, minimizing the risk of pressure injury in the head and neck region.
Point-of-contact problems also exist with thoracolumbar braces that involve the shoulder girdle, pectoral muscles, rib cage, and upper abdomen. The shoulders have a significant amount of overlying skin, fat, and muscle and are by definition highly mobile structures involved in arm movement. Because of this mobility, orthoses that rely on shoulder straps or pads to apply a counterforce cannot consistently distract the spine.13 Changes in body position from sitting to supine also produce shoulder movement contributing to the difficulty of spinal distraction. Koch and Nickel19 studied this effect in six patients wearing the halo apparatus by measuring the forces of distraction and compression exerted through the device with an attached strain gauge. Distraction force varied by more than 20 pounds in a halo vest and 30 pounds in a halo cast when patients changed from supine to sitting positions. Similar variations in distraction with the halo device were noted during shoulder shrugging, coughing, sneezing, and deep breathing. Shoulder purchase is thus a highly variable means of anchoring the caudal end of a distraction orthosis.
Appliances with pads overlying the pectoral areas are compromised by the energy-absorbing effects of fat, muscle, and breast tissue. Movement of the chest occurs with arm motion in a manner similar to that of the shoulders. Although the rib cage is generally a stable structure, deep breathing, coughing, and sneezing produce significant motion that is directly transmitted by all devices purchasing the thorax. Orthoses extending below the thorax to the upper and lower abdomen are at an even greater disadvantage because of the highly elastic nature of this fluid- and air-filled region.8
Fluid Compression
Fluid compression refers to the ability of a tight circumferential binder, such as a corset, to compress partially fluid-filled soft tissues surrounding the spine, thus creating a fluid cylinder.6,8 Because of its mechanical incompressibility, a fluid-filled cylinder has axial load-bearing capacity. For a column model, this technique increases the aggregate cross-sectional area by converting soft tissues into load-bearing structures. Several studies have directly measured the effect of abdominal and thoracic cavity compression, noting little effect of compression on intra-abdominal pressure.6,9,12 In Nachemson and Morris’s20 classic report, however, a 25% reduction in intradiscal pressure was observed in lumbar segments that were braced with an inflatable abdominal corset. The true unloading effect of fluid compression is thought to be a minor factor for orthotic thoracolumbar stabilization and is beneficial only for restricting sagittal plane motion.6 Fluid compression is a strategy that is not applicable for the cervical spine, in which airway, vascular, and muscular tissues make up a relatively large proportion of the cross-sectional area of the neck and do not tolerate significant compression.4
Transverse Loading
Balanced transverse loading describes a common and effective strategy for restricting spinal rotation and translation. Orthoses typically use a three-point bending force application arrangement with two horizontal reactive forces applied at the ends of the column in one direction and a third balancing force in the opposite direction at the fulcrum of the deformity8,13 (see Fig. 187-1C). Because the system is in equilibrium, the sum of all horizontal forces is zero. This prevents translation. Similarly, bending moments generated by the applied forces acting at the axis of rotation for the injured segment also equal zero if rotational motion is adequately controlled.13 Keys to an effective transverse loading strategy include (1) identifying the axis of rotation at the level of injury or point of instability by using an appliance that is centered at or near this axis of rotation and (2) using an adequately long appliance that maximizes the length of the applied moment arm to control the spinal segment of interest.13
Classification
Spinal orthoses are generally considered either conventional orthotics or skeletal fixators. Conventional devices are contact-type orthoses that control spinal motion through direct contact with the skin and soft tissues of the head, neck, thorax, abdomen, or pelvis. A contact orthosis may have only limited skin contact through discrete pads and straps or extensive surface area coverage (e.g., total contact orthosis). Examples of total contact devices are the Yale brace21 and the molded clamshell TLSO (see later discussion). Advantages of newer contact orthoses that use thermoplastic materials include ease of application, light weight, warmth, ventilation, ability to be removed for optimal hygiene, and patient acceptance.22,23 All conventional devices provide some control of flexion and extension but are more limited in reducing lateral bending and rotation.24 Additional drawbacks include poor patient compliance, excessive warmth causing sweating, variability of fit, and complications of skin or soft tissue contact. All devices have limitations that must be balanced with their advantages. Each segment of the spine must be considered individually because of the variability of anatomy, mobility, and applicability of an orthosis.
Harris25 reported the results of a consensus task force of orthotists, spine surgeons, and other health officials who set forth a common nomenclature for conventional spinal orthoses with the intent of standardizing communication among spine professionals and avoiding the plethora of eponyms describing individual appliances (Table 187-1). In this scheme, devices are classified as cervical orthoses (CO), cervicothoracic orthoses (CTO), TLSO, lumbosacral orthoses (LSO), or sacroiliac orthoses (SIO). This classification, which was intended to reflect the region of the spine that is immobilized by the device, has become the standard nomenclature of spinal orthotics since 1973. Krag16 has recently expanded the cervical classification into four subcategories based on the specific anatomy of the region: cervical (CO), occipital-mandibular-cervical (OMC), occipital-mandibular-high thoracic (OMHT), and occipital-mandibular-low thoracic (OMLT).
| Appliance Category | Examples |
|---|---|
| Cervical orthoses | |
| Cervical collars | Foam collar |
| Occipital-mandibular-cervical | Thomas collar, Queen Anne collar |
| Occipital-mandibular-high thoracic | Philadelphia collar, Miami J collar, Guilford two-poster brace, four-poster brace |
| Cervicothoracic orthoses | Yale brace, Minerva brace, SOMI (sternal-occipital-mandibular immobilizer) brace |
| Thoracolumbosacral orthoses | Clamshell thermoplastic body jacket, Jewett extension brace, Boston overlap brace |
| Lumbosacral orthoses | Lumbosacral corset, chairback orthosis, Knight brace |
| Sacroiliac orthoses | Sacroiliac corset with perineal straps |
| Halo devices | Vest halo, four-pad halo, thermoplastic Minerva body jacket |
Cervical Orthoses
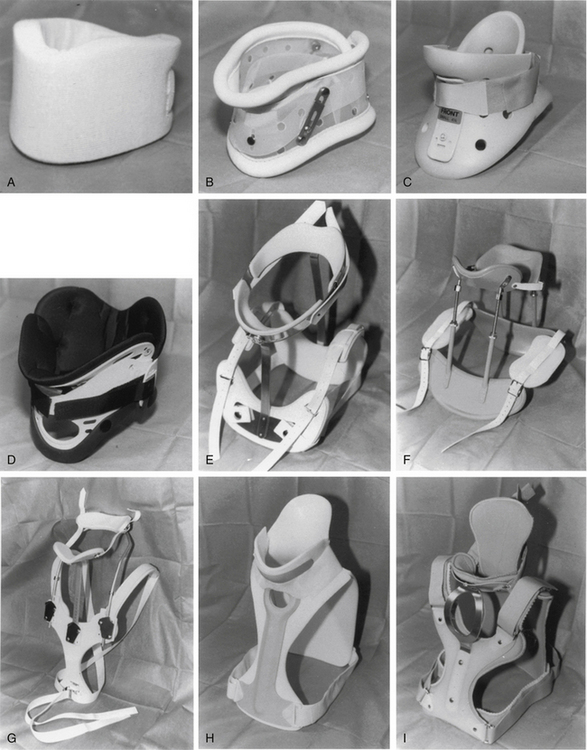
COs are basically soft foam or felt collars with minimal purchase of the mandible or occiput16 (Fig. 187-2A). These collars are light, inexpensive, easy to use, and relatively comfortable to wear. Regrettably, they offer negligible resistance to cervical motion in any plane of motion, functioning only to remind patients to limit voluntary extremes of neck movement.26–28 Because they are only supportive, cervical collars are inappropriate for patients with bony instability. They can provide tactile generated support of cervical musculature and psychological comfort in cases of myofascial strain or sprain or in straightforward postoperative patients without instability.23
Occipital-Mandibular-Cervical Orthoses
OMC orthoses are hard plastic collars that are more rigid than foam collars and offer slightly better purchase of the mandible or occiput16 (Fig. 187-2B). Most usage is as a prophylactic measure, in conjunction with a backboard, in acute trauma situations. They have no thoracic extension; therefore, while offering an improved cranial point of fixation, they lack a true caudal one. The addition of an adjustable chin or occipital piece increases resistance to flexion or extension to a mild degree.26 Lateral bending and rotation are poorly controlled with these braces.24 Like the soft collars, OMC orthoses do not provide significant immobilization to the cervical spine and are not recommended for patients with instability.
Occipital-Mandibular-High Thoracic Orthoses
Examples of OMHT orthoses are the widely used Philadelphia collar, the four-poster brace, the two-poster brace (e.g., Guilford, Duke), and several newly available hard plastic collars16 (Figs. 187-2C–F). All OMHT appliances control head movement with occipital and mandibular supports and have better upper thoracic purchase than collars because of longer length. Like the collars, they are relatively easy to apply, are lightweight, and are relatively inexpensive.
The popular Philadelphia collar is a Plastazote foam device reinforced with hard plastic. It is available in different sizes and consists of front and back halves connected by Velcro straps.3 Although generally well tolerated, it can be quite hot to wear, causing significant sweating and secondary skin maceration. The Plastazote material is less rigid than other OMHT appliances such as the poster orthoses.29 Despite its limitations, Johnson et al.24 found this device to be as effective in controlling upper (C0-3) flexion-extension as the rigid OMHT orthoses. It was less effective in restricting flexion-extension in the midcervical and lower cervical segments (Fig. 187-3) and poor in controlled rotation and lateral bending at all levels. The device is frequently used for patients with mild cervical injuries and in postoperative patients with minor instability. Polin et al.30 evaluated the use of the Philadelphia collar and the halo device in odontoid fractures. Their findings indicated no significant difference in the rate of fracture healing between the two orthoses for both type II and type III fractures and suggested that the less invasive collar may be adequate in this setting. Modifications of the Philadelphia collar have been developed that maintain cervical immobilization yet improve the comfort and convenience of a plastic removable collar. In 2009, Koller et al.31 did an in vivo analysis of atlantoaxial motion in 20 healthy volunteers, comparing the halo thoracic vest and the Philadelphia collar. They found that, as expected, the absolute range of motion of the subaxial spine was more restricted by the halo vest than that of the Philadelphia collar. However, they found that the atlantoaxial complex had a tendency to be more restricted in sagittal motion between extreme flexion and extension in the Philadelphia collar (mean, 1.3 degrees) than in the halo vest (mean, 3.3 degrees). The author subsequently suggested that a Philadelphia collar might be sufficient in the conservative treatment of stable odontoid fractures.
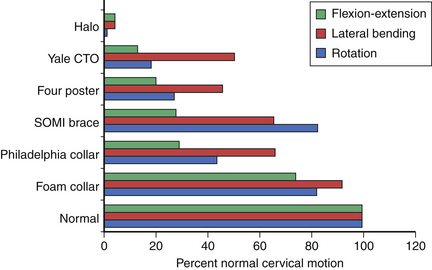
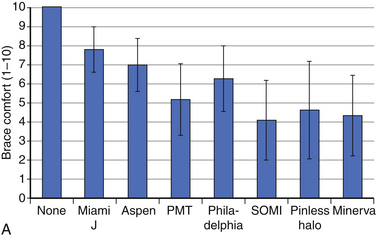
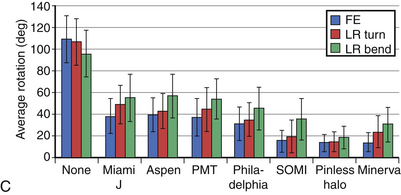
FIGURE 187-3 Overall motion allowed in cervical orthoses.
(From Johnson RM, Hart DL, Simmons EF, et al: Cervical orthoses: a study comparing their effectiveness in restricting cervical motion in normal subjects. J Bone Joint Surg [Am] 59:332–339, 1977.)
Schneider et al.32 did a biomechanical evaluation of common cervical orthoses. They looked at reduction in head and intervertebral motion provided by seven contemporary cervical orthoses in 45 individuals. They evaluated the overall range of motion of the head in three planes as well as intervertebral motion in the sagittal plane. The tested subjects also reported comfort for each brace being tested.
With respect to patient-reported comfort, there was a significant association between the type of brace and patient-reported brace comfort score. The most comfortable orthoses were the Miami J and the Aspen. In general, the cervical collars were more comfortable than the cervicothoracic orthoses32 (Fig. 187-4A).
With respect to the motion restriction of the head, all cervical braces significantly reduced overall sagittal plane flexion-extension motion of the head as well as axial rotation and coronal plane side-to-side bending. As was expected, however, some braces reduced motion significantly more than others did32 (Fig. 187-4B).
The intervertebral motion was measured from the fluoroscopic images of maximum flexion and extension; all braces significantly reduced intervertebral rotation at all levels. Some of the braces reduced rotation more than others, and the differences between braces were more pronounced at the midcervical than the upper or lower cervical levels32 (Fig. 187-4C).
Occipital-Mandibular-Low Thoracic Orthoses
The OMLT orthoses are represented by the sternal-occipital-mandibular immobilizer (SOMI), the extended Philadelphia collar (Yale brace), and the Minerva brace (Figs. 187-2G–I). These devices are essentially longer versions of the OMHT appliances with the addition of circumferential chest straps. In general, they are the most rigid of the conventional orthoses because of their increased length and better thoracic purchase24,29 (see Figs. 187-3 and 187-4). Advantages of the OMHT orthoses include best immobilization of flexion-extension and rotation of the conventional braces, noninvasiveness, and ease of application. However, they are more cumbersome and uncomfortable to wear than the smaller appliances. With the exception of the Yale brace, they are moderately expensive and still have limited control of lateral bending.21,24
Thoracolumbosacral Orthoses
Representative TLSOs include the clamshell thermoplastic body jacket and the thoracolumbar extension orthosis or Jewett brace (Figs. 187-5A–C). There are a number of modifications of these two basic designs. By definition, these appliances apply three-point bending forces at the upper thorax and pelvis and at the midportion of the brace across the thoracolumbar junction.1 This class of orthotic is best suited for restricting thoracolumbar and lumbar gross-body motion33 and poorly controls low lumbar and sacral segments.14 Molded appliances are particularly useful for thoracolumbar junction trauma in which the total contact feature helps to control lateral bending and rotation. Velcro straps and thermoplastic materials have greatly improved the ease of wear and comfort of TLSOs in recent years, improving both compliance and effectiveness.
Jewett braces primarily control flexion-extension and are therefore often used for minor flexion compression injuries such as stable compression fractures.3 More severe thoracolumbar injuries were recently studied by Patwardhan et al.34 with a finite element computer model. The Jewett brace was effective at preventing deformity under physiologic flexion loading with injuries that resulted in less than 50% normal spinal stiffness (single-column injuries). With injuries that reduced stiffness to between 50% and 85% (two-column injuries) and those greater than 85% (three-column injuries), the brace was ineffective for resisting spinal deformation.34
Lumbosacral Orthoses
Perhaps the most frequently prescribed appliances, LSOs are also the most controversial because of their questionable effectiveness.6 Lumbosacral corsets with or without stays, chairback braces, and the Knight brace are representative3 (Fig. 187-5D). LSOs stabilize the lumbar and sacral regions by encircling the upper abdomen and rib cage and the pelvis. Because of the difficulty in firmly purchasing these areas, three-point bending is probably not a major mechanism in the action of this class of orthosis. Fluid compression likely has a role, although measurements of intra-abdominal pressure while wearing the devices have been inconsistent.9
To quantify the effect of bracing on segmental motion, Norton and Brown11 measured lumbar motion in volunteers by following the motion of K-wires inserted into the spinous processes. Movement at the lumbosacral junction was paradoxically greater while sitting with an LSO than without the brace. The effect was thought to be secondary to stress concentration at the caudal end of the supported segment. Waters and Morris12 studied lumbosacral stabilization in orthoses by monitoring paraspinal muscle electromyography. Although back muscle activity during standing was reduced with an LSO, activity during fast walking was greater, possibly because of altered pelvis rotation. Lantz and Schultz33 measured gross trunk motion and myoelectric activity in five volunteers wearing the lumbosacral corset, a chairback brace, and a molded TLSO during standing and sitting. Gross upper body motion was reduced up to 20% in flexion and 45% in extension, lateral bending, and rotation. The TLSO was overall the most effective device tested. Myoelectrical activity varied widely, however, ranging from a 9% reduction to a 44% increase.35 Axelsson et al.14 used stereophotogrammetry in seven patients to analyze the effects of the LSO and the molded TLSO on intersegmental lumbar spine movement. Neither device had any effect in restricting segmental translation in sagittal, vertical, or transverse planes. They concluded that the orthoses serve only as a reminder to the patient to restrict gross trunk movements.14
These observations substantiate clinical experience that the LSO and TLSO do not adequately stabilize segmental motion of the lower lumbar spine and lumbosacral junction. They do appear to limit gross trunk movement, which is thought to be their major mechanism of action.33
Consistent with the principles of long bone splinting discussed earlier, control of the pelvis may be necessary to restrict movement at the lumbosacral junction.4,13 Fidler and Plasmans36 have shown that including the thigh with an extension (thigh spica) reduces gross pelvis motion more significantly than a conventional LSO does. Segmental translation with axial loading, however, is not affected by this device.37 In clinical practice, patient acceptance of thigh spica orthoses is limited because of severe restriction of walking and sitting (Fig. 187-5E).
Sacroiliac Orthoses
Rarely used today, sacroiliac orthoses were developed for pelvic instability after traumatic or postpartum pelvic disruption.14 They are not effective at reducing motion but rather serve as a kinesthetic device to remind the patient to maintain proper pelvic posture.
Halo Skeletal Fixation
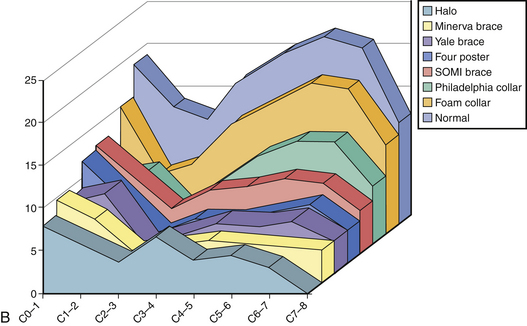
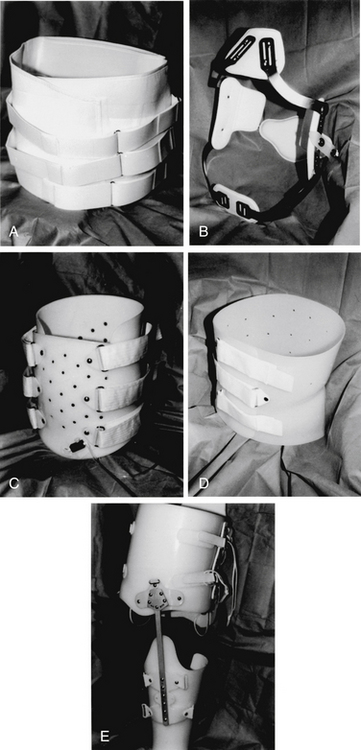
Halo fixation is currently the most effective method of externally immobilizing the cervical spine.16 Its basic components consist of a halo ring (or crown) for pin fixation of the skull, a plastic vest or pads secured with straps that encircle the thorax, and two or more upright connecting posts. A variety of commercial products are available that incorporate design features that reflect clinical experience and advances in metal and plastic technology38 (Fig. 187-6).
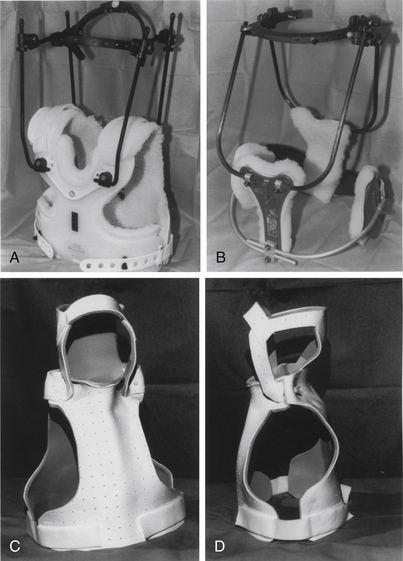
FIGURE 187-6 Halo-type orthoses. A, Standard halo vest. B, Four-pad halo vest. C and D, Thermoplastic Minerva body jackets.
Clearly, the major advantage to the use of the halo is the degree of stabilization that can be achieved. Johnson et al.24 demonstrated a reduction of lateral bending and axial rotation in five patients to 1% of that of normal volunteers. Whole cervical spine flexion-extension was similarly reduced to 4% of normal (see Fig. 187-4). Although the halo affords a high degree of stability, persistent significant motion does occur. Koch and Nickel19 studied halo immobilization in six patients with fractures, demonstrating an average of 31% normal motion for cervical spine flexion and extension at each motion segment. The greatest movement occurred between C2 and C3, with the least at C7-T1. They emphasized the importance of body position or activity such as lying, bending, or sitting in transmitting undesirable force to the cervical spine through the halo itself.
Although distraction is frequently useful to maintain reduction of highly unstable spines, the ability of the halo to provide fixed distraction is limited because of this significant effect of trunk position and patient activity.19 It should not be used as a principal distraction device.
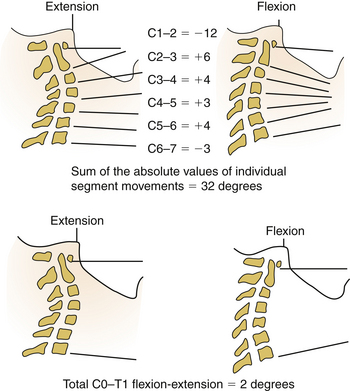
Paradoxical spinal motion described as snaking accounts for most of the undesirable movement that occurs with the halo.13,15,39 It is the segmental motion that occurs while the end points of the braced region remain relatively fixed along the spinal axis and involves simultaneous capital protraction and flexion of the upper cervical spine with extension of lower cervical segments (e.g., C0-3 flexion with C5-T1 extension on attempted neck flexion). The measured whole cervical spine movement from C0 to T1 may be minimal, yet individual midcervical segments move significantly without effective fixation13 (Fig. 187-7). Increasing the length and the conformation of a brace minimizes the parallelogram deformation of the spine and the snaking phenomenon. This also maximizes the biomechanical effect of the brace.
The thermoplastic Minerva body jacket (TMBJ)22 is an alternative to halo bracing (see Fig. 187-6). This device consists of a bivalved molded plastic shell that has contact-type purchase of the thorax like that of a standard halo vest and lateral extensions that incorporate a mandibular support, an occipital support, and a circumferential headband.23 Benzel et al.22 compared its effectiveness with the halo in 10 patients with cervical spine injuries. Each patient was tested in whole cervical spine flexion-extension with both the halo and the TMBJ. Their results indicate improved control of individual vertebral angulation at all levels except C1-2 with the TMBJ versus the halo. There was less paradoxical movement with the molded device, indicating a higher overall level of immobilization. Eight of 10 patients reported improved comfort.22 Maiman et al.40 also studied the TMBJ in 20 normal volunteers for controlling flexion-extension, lateral bending, and axial rotation. The TMBJ significantly reduced motion as compared with unrestricted controls in all planes except rotation. It was more effective than the halo in restricting flexion-extension and lateral bending when compared with the historical data of Johnson et al.24 and Wang et al.41 In practice, the effectiveness of the device depends on the ability to achieve an excellent fit, which requires an expert orthotist who is familiar with its use. The TMBJ also suffers the disadvantages of any contact orthosis, such as skin irritation, mandible obstruction, discomfort, and warmth.
Complications of Spinal Bracing
Complications of bracing can be organized into three general categories: skin and soft tissue injuries, ineffective stabilization, and a variety of miscellaneous complications, largely related to halo skeletal fixation (Box 187-1).
BOX 187-1 Complications of Orthoses
Skin and Soft Tissue Injury
All orthoses require some degree of skin-appliance connection to apply forces indirectly to the vertebral column. Excessive pressure on the skin causes ischemia with resulting pain, breakdown, and/or frank ulceration. Pressure is defined as force per unit area and is the major cause of decubitus ulcers occurring over bony prominences in patients with poor mobility and prolonged recumbency.17 Tissue breakdown is normally avoided because of painful exteroceptive feedback that occurs when skin pressure is prolonged. Discomfort stimulates subconscious shifting of position to unload the dependent body part. Altered sensation (Fig. 187-8), consciousness, or mobility impairs normal protective mechanisms13,42 and can lead to a variety of possible injuries, depending on the severity of the ischemic deficit43 (Table 187-2). Careful and frequent inspection of skin contact areas beneath braces is mandatory to identify the earliest stages of injury and allow intervention before irreversible skin damage occurs.42
| Stage I | Hyperemia | Nonblanching erythema appearing within 30 minutes of pressure that disappears within 1 hour |
| Stage II | Ischemia | Seen after 2–6 hours of continuous pressure; erythema requires 36 hours to resolve |
| Stage III | Necrosis | Skin appears blue and firm after 6 hours of pressure; skin changes do not resolve |
| Stage IV | Ulceration | Occurs 2 weeks after stage III injury appearing as ulcer formation and infection; may involve underlying bone |
Adapted from Edberg EL, Cerny K, Stauffer ES: Prevention and treatment of pressure sores. Phys Ther 53:246–252, 1973, with permission.
Because of their significant effect on patient management and the economic impact of treatment, decubitus ulcers have been the focus of a number of clinical and basic science investigations.18 Important factors identified experimentally for developing pressure sores include the magnitude and duration of the applied pressure, associated shear or friction of the skin, tissue distribution, skin moisture, hydration, and general nutrition.17,18,42 Tissue damage from pressure occurs by microvessel occlusion that impairs perfusion and leads to secondary ischemia. External pressures exceeding normal tissue capillary perfusion pressure (32 mm Hg)44 will interrupt blood flow, leading to ischemia and permanent tissue death if unrelieved. The duration of application is inversely related to the absolute pressure.18 Kosiak45 has reported the relationship between duration and the risk of pressure sores in a series of studies that used a canine model. Pressures of 500 mm Hg applied to the skin surface for only 2 hours produced ulceration, whereas 150 mm Hg was tolerated for up to 12 hours. Pressure as low as 70 mm Hg, however, was sufficient to produce microscopic ischemic changes after only 2 hours. Thus, a continuum of injury may be seen that is related to increasing pressure magnitude and duration.
Surface friction potentiates the risk of ulceration by creating shear in deeper soft tissues. Shear leads to capillary occlusion by kinking, stretching, and tearing and produces ischemia at lower absolute externally applied pressures.17,42 A study in a porcine model compared the threshold for skin damage from a force applied with and without linear shear.46 Ulceration occurred at less than one sixth the external pressure (45 mm Hg) when combined with shear than without added shearing forces (290 mm Hg). Surface friction also can abrade outer layers of skin, especially if the subcutaneous tissues are very firm or tightly tethered to the underlying bone.17 Friction abrasions then further contribute to decubitus ulcer formation. Adequate systemic hydration can mitigate the effects of shear by increasing the mechanical resilience of skin.42
An important consequence of pressure in advanced-stage injuries is the effect on muscle. Muscle is more vulnerable to ischemia than is skin, because it typically develops necrosis earlier and more extensively.18 Pressure distribution between the skin surface and the underlying bone concentrates force at the deep bone-muscle junction because of the abrupt tissue transition from bone to muscle. Necrosis tends to be maximal at the level of the underlying bone and decreases gradually outward toward more superficial layers.47 External skin ulceration is usually only the external manifestation of a more extensive soft tissue injury.42 Although vulnerable to ischemia, muscle and fat layers paradoxically are important for dissipating force through the energy-absorbing process of elastic deformation. Thus, poorly covered bony prominences such as the sacrum, greater trochanter, and heels that are without significant soft tissue layers are particularly vulnerable to skin breakdown. Pressure dissipation plays a major role in the beneficial effects of muscle flap transfers used to cover ulcerated bony prominences.48
The barrier function of skin is compromised by prolonged exposure of its surface to moisture. Moisture from incontinence or sweating overhydrates the outer layer of the stratum corneum, reducing its mechanical strength and resistance to bacterial permeation.42 Increased temperature caused by impaired heat convection further allows microflora to proliferate and reduces the tissue pH. These changes result in epidermal sloughing, deep layer exposure, and microbial invasion of the underlying dermis, all of which promote ulceration.
Similar conditions frequently threaten skin integrity beneath occlusive spinal orthoses. Braces that poorly dissipate pressure, impair proper hygiene, create significant shear, and allow moisture buildup are most likely to promote tissue injury. Regrettably, little data for the frequency of skin ulceration exist for conventional orthoses other than that noted in anecdotal reports. For the halo device, pressure sores have been observed in 4% to 11% of patients and usually occur over the scapulae or rib cage.49–52 Practical means to prevent these complications include optimizing the orthotic fit, maximizing the applied surface area of the brace to dissipate pressure, and avoiding appliances with sharp or uneven edges.17 As was stated, areas over bony prominences have minimal overlying soft tissue to distribute pressure by elastic energy absorption and are most vulnerable to ischemic injury under an orthosis. Adding special padding or cutting out a hole immediately over a prominence may avoid breakdown by shifting pressure away from high-risk areas to more tolerant tissues.
Hygiene is a function of patient education and proper nursing and is greatly facilitated by modern, removable appliances.42 Patients should be fully educated as to the risks and warning signs of early skin ulceration and should participate actively in its prevention. Special problems occur with anesthetic skin that does not produce noxious feedback to warn of excessive or prolonged pressure13 (Fig. 187-9). This can also occur in obtunded or comatose patients. Shear under an orthosis can be avoided by a properly fitted brace and by maintaining a moisture-absorbing layer between the skin and appliance at all times. A cotton undergarment that can be changed daily is useful in this regard both for hygiene and moisture reduction.
In the nutritionally depleted patient, general protein wasting may lead to tissue edema, altered tissue repair, and compromised antimicrobial mechanisms. Edema impairs tissue oxygenation, decreases elasticity, and reduces skin resistance to mechanical deformation. Marker serum proteins such as transferrin and albumin and anergy to injected antigens are common and useful indicators of nutritional status. Assessment of nutritional status and correction if inadequate may prevent or delay developing pressure sores associated with orthoses.42
To determine the incidence and risk factors associated with the development of cervical collar-related decubitus ulceration (CRU) in trauma patients immobilized in Philadelphia cervical collars, Ackland et al. did an exploratory study from a trauma registry database at a level 1 trauma center; 299 major trauma patients admitted over a 6-month period were identified. Predictors of CRU were retrospectively examined and assessed for relative importance by using medical records and prospective infection control and radiology databases. Using logistic regression analysis, they found that significant predictors of CRU were ICU admission (P = .007), mechanical ventilation (P = .005), the necessity for cervical MRI (P ≤ .001), and time to cervical spine clearance (P ≤ .001). Time to cervical spine clearance was the major indicator, such that the risk of CRU increased by 66% for every 1-day increase in cervical collar time.53
Postoperative wounds are especially prone to skin edge maceration and secondary bacterial invasion if covered by occlusive orthoses, because of the combined negative effects of sweating, external pressure, and shearing forces.54 Frequently changed, dry dressings over the wound reduce these effects and prevent most orthosis-associated wound infections. Alternatively, a noncontact or ventilated device may reduce this risk.
Other soft tissue complications of spinal bracing include muscle atrophy and contracture formation.4,6 Atrophy occurs rapidly after even brief periods of disuse because of a lack of normal motion and tone. Resulting loss of bulk and weakness may be profound, requiring progressive weaning from the appliance and active rehabilitation after bony healing is established. Although commonly observed in this setting, atrophy associated with spinal bracing has not been thoroughly quantified. Contractures are rigid deformities of a joint caused by immobilization or unbalanced effector forces across the joint. With time, the associated muscles can become painful and permanently fibrotic. Contractures are occasionally observed with long-term cervical bracing or halo use and primarily involve limited cervical rotation. Lind et al.52 have reported up to 80% residual neck pain and stiffness after halo bracing, which probably represents minor cervical contracture formation.
Korovessis et al.55 recently reported an interesting soft tissue complication associated with long-term use of a modified Boston brace in young women braced for scoliosis. The appliance uses a rigid pelvic band that covers the dorsolateral hips over the greater trochanters and is open over the lower flank region. Prolonged use (>6 months) led to upward migration of the lateral trochanteric fat pads in 23% of 300 subjects, resulting in significant cosmetic deformity. Suction lipoplasty was required in 74% of this group. Pressure atrophy of developing fat deposits with local redistribution appears to account for this phenomenon.55
Ineffective Stabilization
As was previously discussed, most conventional braces poorly transmit force directly to the spine and are limited in their ability to restrict segmental motion and/or unload the vertebral column. Long conventional appliances spanning many segments across the level of interest are most effective for controlling gross body movement because of significant three-point bending.33 Mismatch between the point of spinal instability and the optimal effective range for a particular brace (typically at its midpoint) accounts for a common cause of ineffective brace selection. Similarly, extensive instability or injuries that are only reduced by axial distraction are not usually amenable to conventional bracing. Most studies of orthotic effects involve kinematic evaluation of stability in single trials of spine motion, usually in healthy subjects. The questions of clinical effectiveness are less well answered because of limited availability of longitudinal outcome data for various devices.
Despite its limited effect on segmental motion, the TLSO may improve fusion success by restricting gross trunk motion. Johnsson et al.56 recently studied the effect of a molded TLSO in 22 patients undergoing dorsolateral fusions. One group of 11 patients was braced for 3 months, and the other group was braced for 5 months. Segmental motion was evaluated by stereophotogrammetry. Fusions became progressively more rigid beginning at 3 months in both groups. By 1 year, however, patients who had been immobilized for 5 months showed a higher rate of fusion than the 3-month group, indicating a direct benefit of longer immobilization.56
Although the halo is the most rigid cervical appliance in kinematic testing, success in clinical application varies, especially with ligamentous instability. Cooper et al.57 reviewed their experience with halo bracing of unstable injuries in 33 patients. They reported few minor complications and restored stability in 85%. In only four patients did therapy fail. Patients with ligamentous subluxation or angulation were most prone to lose halo reduction. Whitehill et al.58 also reported five patients with unstable ligamentous facet dislocations or subluxations who failed to maintain reduction with the halo. Of 36 patients with facet dislocations or fracture-dislocations reviewed by Beyer et al.,59 19 underwent halo immobilization. Only one third achieved proper alignment, and one fourth achieved anatomic reduction. Half of the halo group lost reduction during bracing. They recommended open reduction and fixation of facet dislocations for better alignment and fusion results. Rockswold60 reviewed 604 patients in five studies from the literature who were treated with halo stabilization for a variety of cervical injuries. Failed reduction and/or fusion occurred in 12% to 23% of patients. Hyperflexion ligamentous injuries had the highest failure rate. From these and other observations, it appears that the halo is an effective means for stabilizing many cervical injuries unless primary ligamentous instability exists. Paradoxical motion, or snaking, of the spine with associated midcervical angulation may account for the inadequate stability in ligamentous injuries.13
Noncompliance
As was previously stated, it was shown that the effectiveness of an appliance is directly related to the level of its discomfort.3,4 This also contributes to higher levels of noncompliance.
Regardless of the patient population, a limitation to studies assessing the effectiveness of bracing is the lack of objective data on how long a brace is actually worn. The majority of available literature regarding brace compliance is based on the assumption that subjective reports of brace compliance are accurate. Diaries, logs, and self-reporting have all been used as means of recording compliance with bracing. DiRaimondio and Green61 reported, on the basis of patient interviews, that fewer than 15% of their patients were highly compliant with the prescribed wearing schedule. Compliance rates as high as 64% and 88% have been reported with subject self-reporting.62,63 Subjective reports should not be considered the most accurate measurement of brace compliance. According to a recent study, Helfenstein et al.64 found that subjective reporting does not appear as accurate as using an objective measure of brace compliance. The investigators in this study used a temperature data logger to monitor the brace wear of nine women with idiopathic adolescent scoliosis up to 3 months. A questionnaire to measure self-reported compliance was used. The average objective compliance was 68% (subjects were recommended to wear the brace 23 hours per day), and the subjective self-reported compliance average was 94%.
Over the last several years, sensors that can be attached to braces have been designed to measure wearing time objectively. Takemitsu et al.65 used a temperature sensor embedded in the TLSO of children with idiopathic scoliosis. Havey et al.66 developed a force-sensitive resistor that was placed in TLSOs to assess wear time in normal volunteers and found it to be accurate and reliable.
Miscellaneous Complications of Spinal Bracing
Halo-vest immobilization (HVI), developed by Koch and Nickel,19 is the gold standard for providing maximal, externally mediated immobilization of the cervical spine. However, studies citing high complication rates and low success rates have called its clinical usefulness into question.19,67
Bransford et al.68 evaluated the survival of the halo vest to full completion of the originally prescribed treatment plan, as well as failure and complication rates. It was found that the intended duration of HVI was completed in 74% of patients. Also, the desired clinical outcome of avoiding surgical intervention was achieved in 85% of patients in whom the intent had been definitive halo treatment. This success rate is identical to the ones reported by Bucholz and Cheung69 and by Cooper et al.,57 in previous similar series.
Other than pin site infection, Bransford et al.68 found that the primary complications were instability or failure of the halo to maintain acceptable alignment, which consisted of approximately one third of all complications. In fact, failure to maintain acceptable stability of the spine was the leading cause of cessation of HVI. Other studies have shown similar secondary loss of reduction or persistent spinal column instability, with a previously reported incidence ranging from 9% to 15%.51,52,69–71 Two thirds of all failures occurred within the first 3 weeks of halo application, suggesting that this early phase is critical in determining the likelihood of success.
Halo Pin Site Complications
Pin site complications are among the most common limitations of halo bracing and have been studied extensively49,50,52,68,72 (Table 187-3).
| Complication | Percentage |
|---|---|
| Loosening | 36–60*† |
| Pin site infection | 20–22*† |
| Local pain | 18† |
| Ring migration | 13*† |
| Scarring | 9–30*† |
| Nerve injury | 2* |
| Pin site bleeding | 1* |
| Intracranial puncture | 1* |
* Data from Garfin SR, Botte MJ, Waters RL, et al: Complications in the use of the halo fixation device. J Bone Joint Surg [Am] 68:320–325, 1986.
† Data from Lind B, Sihlbom H, Nordwall A: Halo-vest treatment of unstable traumatic cervical spine injuries. Spine (Phila Pa 1976) 13:425–432, 1988.
Adapted from Botte MJ, Byrne TP, Abrams RA, Garfin SR: Halo skeletal fixation: techniques of application and prevention of complications. J Am Acad Orthop Surg 4:44–53, 1996, with permission.
Pin Loosening
Pin loosening is seen in 36% to 60% of patients and is usually heralded by pain in the absence of associated infection.52,71 Occasionally, a fall or blunt trauma to the halo ring will result in acute loosening.50 Current pin tip designs use a broad pin shoulder to maximize skull contact and help to limit loosening or perforation.73 Ballock et al.74 evaluated optimal pin site placement in a cadaver model, noting that pins inserted lower on the skull above the supraorbital ridge were more rigidly affixed than were more superiorly placed pins. The lower pins were more perpendicular in orientation, which reportedly accounts for their improved rigidity. Botte et al.71 studied the effect of pin insertion torque on subsequent pin loosening and reported improved mechanical characteristics of the pin-bone junction at 8 inch-pounds versus 6 inch-pounds. Loosening was reduced to 7% from 36%, respectively.13 Rizzolo et al.75 also addressed pin insertion torque, randomizing two groups with pins inserted to torques of 8 or 6 inch-pounds. No significant difference between groups was noted, although a trend toward higher rates of loosening (26% vs. 20%) and infection (13% vs. 7%) occurred with the 8-inch-pound insertion torque. Currently, 6 to 8 inch-pounds are recommended for initial insertion torque, which is subsequently checked at 24 to 48 hours.72 If remote loosening occurs without infection, the pins should be tightened once as long as resistance is encountered. Garfin et al.50 found that 16% of loosened pins reloosened after tightening. Pins that were moved also loosened in 17%, suggesting that loosened pins compromise the balance of the other pins in the halo ring.50 Repeated tightening leads to cranial perforation, because local bone erodes rapidly under pressure from the pin.
The actual force that is applied through the pin at the pin-skull junction appears to vary considerably for a given torque, depending on the method of insertion and the size and type of halo ring used. Whitesides et al.76 measured force exerted through the pin for different insertion torques in several types of halo rings. They noted a wide variation in force among rings of different size and material composition. Flexibility of the ring and its effect on the coefficient of friction at the pin-ring junction reportedly accounted for the variation. Lubrication of the junction with saline significantly reduced friction between the pin and the ring. They recommended using an insertion torque specific for the type of halo used to standardize the force applied to the skull.76 Kerwin et al.77 also found wide variation of pin force with different ring sizes and materials. Friction between the ring and pin threads increased with ring flexibility. Addition of a locking nut paradoxically reduced pin force by either backing out the pin or altering the ring shape.
Infection
Skeletal fixation by definition violates the integrity of the scalp, risking local infection. Pin sites require continuous daily inspection and cleaning with hydrogen peroxide and application of a topical antibiotic such as polymyxin ointment. Despite excellent pin site care, local infection will occur in between 13%68 and 22% of patients.49 Increasing erythema and purulent drainage around the pin indicate early soft tissue involvement and can usually be treated with a culture-specific oral antibiotic and close follow-up.
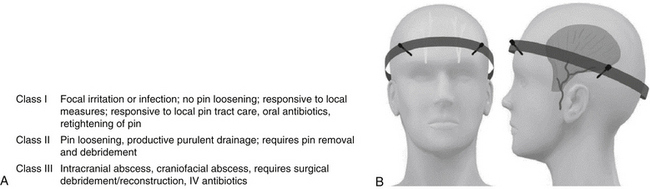
In 2009, Bransford et al.68 published a retrospective study of 490 cases of traumatic cervical fractures treated with HVI. The author classified the infection type in three categories (Fig. 187-10).68 Overall, 38% of infections were limited locally and required only local wound care and PO antibiotics (class I). Fifty-six percent were considered class II infections and required pin removal and local debridement. Finally, 5% were considered complicated infections such as brain abscess or major craniofacial abscess and required surgical debridement and IV antibiotics.
Brain abscess is a rare but serious result of cranial pin fixation that is typically associated with overlying soft tissue infection and/or secondary osteomyelitis. Of five cases reviewed by Goodman and Nelson,78 three had associated osteomyelitis, and all involved tightening of a loosened pin. Rosenblum and Ehrlich79 described a patient who presented with acute psychosis as an initial manifestation of an intracranial abscess. His halo pin had been tightened twice because of loosening, the second time 1 week before presentation. These reports underscore the danger of repeatedly tightening loose pins. A pin that becomes loose should be retightened only once in the absence of frank scalp infection. Further loosening after initial retightening is an indication for insertion at another site.
Less frequent halo complications include frontal scarring, nerve injury, bleeding, and cranial puncture.72 Scars from frontal pin sites are usually cosmetically acceptable for most patients. However, up to 30% of patients develop severe scarring that may require further treatment.52 Local infection, pin migration, and keloid formation may contribute to this problem. Incising the skin before insertion does not improve cosmetic outcome.72 Garfin et al.50 reported continuous local pain at pin sites in 17% of 180 patients who were treated in halos. Repeated periosteal irritation was thought to be the basis for chronic pin site pain.50 Alternatively, pins that are mistakenly positioned through the temporalis muscle in the temporal fossa are also painful because of muscle trauma and continued irritation during jaw movement.72 Paradoxically, newly developed pin site pain often indicates a loosening pin. Nerve injury with pain and paresthesias may occur with pin trauma to the supraorbital or supratrochlear nerves as they course superiorly from their foramina to innervate the frontal scalp. Pin movement is often required because of the severity of symptoms. Avoiding medial pin placement should prevent this complication.72 By placing frontal pins into the fronto-orbital crest, obvious scars, nerve injuries, and temporalis muscle pain may be avoided. Bleeding from pin sites has been reported in patients receiving chronic anticoagulants.50 Discontinuing anticoagulation resolves this rare and unusual complication. Intracranial puncture has been discussed in association with repeated pin tightening or frank trauma to the halo ring such as with a fall. Although rarely reported, this can lead to serious intracranial infection and loss of fixation72 (see Table 187-3). Figure 187-10B depicts the appropriate halo ring positioning to avoid nerve as well as cosmetic complications.
Overdistraction
Because the thoracic vest of the halo transmits significant force through the device to the cranium, distraction and compression forces vary widely with different patient positions and activities.19 Overly vigorous attempts to maintain axial traction in a halo can result in overdistraction and cause associated swallowing difficulties or neck discomfort. Dysphagia has been noted in up to 2% of patients50 and results from impaired larynx movement required for coordinated swallowing. Avoiding excessive distraction and head extension will usually prevent this complication.
Cardiopulmonary Complications
Cardiopulmonary complications of bracing mainly involve changes in venous pressures of the trunk, abdomen, and lower extremities. Kaplan et al.80 described acute pulmonary edema occurring in an obese 63-year-old trauma victim after removal of a halo that had been in place for 14 weeks. Occult mitral stenosis was subsequently diagnosed. They postulated that removal of the halo vest resulted in a loss of the mechanical impediment to venous return, resulting in rapid volume loading of the heart, which was not compensated because of occult mitral stenosis. Improved ventilatory mechanics after halo removal also increased venous return, worsening pulmonary edema. Lower-extremity venous hypertension is an additional concern for developing varicose veins, venous stasis with thrombosis, or hemorrhoids.4 This is most commonly seen with the TLSO, although it has not specifically been reported or quantified.
Conventional orthoses and halo vests may compromise respiratory function by restricting expansion of the chest and abdomen. To measure this effect, Lind et al.81 studied spirometry of 20 trauma patients in halos at 1 week of treatment, at 3 months, and after removal of the appliance. The halo reduced vital capacity by 8% to 9%. With prolonged wearing, vital capacity increased by 10% because of adjustment of the vest, reduction in acute pain, loss of cautiousness, and respiratory training. Levels remained at all times more than adequate to support normal respiratory function.81 Although this study demonstrates only a minimal reduction in vital capacity, the effect on patients with chronic obstructive pulmonary disease is unknown and may be more functionally significant.
Gastrointestinal Dysfunction
Compression of the abdomen, especially combined with extension, may occasionally stretch the superior mesenteric artery across the ventral aspect of the distal duodenum, compressing it against the aorta.13 The superior mesenteric artery syndrome or cast syndrome results in postprandial bilious emesis, epigastric pain, and distention from partial duodenal obstruction.82 A barium study typically shows duodenal compression with delayed passage into the small bowel. Contributing factors include acute weight loss, recumbency, posturing, and spasticity.83 Treatment is expectant with discontinued bracing, gastric decompression, parenteral alimentation, or enteral feeding through a tube passed beyond the duodenum. Refractory cases may require surgical exploration. Dysphagia is a frequent complaint related to the use of the halo. Mechanical changes in swallowing, with subsequent dysphagia, were noted with the application of the halo vest in overdistraction or hyperextention in healthy volunteers.84
Psychosocial Dysfunction
A number of authors have noted severe psychological problems associated with spinal bracing in up to 3% of patients.6,50,85 Scoliosis bracing typically involves female adolescents with a significantly intrusive appliance that markedly affects body image. Initial adjustment disorders have been described, ranging from varying degrees of depression to noncompliance and eating disorders.86–88 Similar adjustment problems with other conventional devices have not been quantified, although concerns about appearance, complaints of claustrophobia, and anxiety over lost independence are commonly expressed. Orthoses are very visible symbols of infirmity, which may foster adoption of a sick role. Psychological dependence and secondary gain are not uncommon among chronic collar users because of this change in body image and its connotation of legitimate injury.4 Bracing should therefore be used only when indicated for specific stabilization goals that have defined end points.
New Advances and Developments
Recent developments in materials and techniques have led to many improvements in older orthoses as well as the invention of some new strategies. Advances have sought to both simplify their application and to increase patient comfort, in turn delivering greater compliance. Specifically, new strap and closure configurations have made some devices easier to apply, adjust, and remove. Further front adjustments allow additional customization to follow body contour variations from the top of the torso to the waist and hips. Additional options include male and female liners, pendulous fronts, and adjustable lumbar control permitting custom curvatures from 0 degrees to 40 degrees. These advances have led some companies to claim the ability to fit 98% of the adult population (ComfAlign, The Bremer Group Company, Jacksonville, FL).
Some companies have adopted novel techniques to increase support while decreasing the incidence of skin breakdown. The Aspen cervical collar (Aspen Medical Products, Inc., Long Beach, CA) utilizes a three-layered system to achieve effective motion restriction. Two stiff inner layers of plastic provide the majority of support, while an outer, more flexible layer is slotted along its edges, allowing better conformation with the patient’s anatomy. The resultant better fit reduces the pressure points that are commonly found at the mandible, sternum, and clavicles. Studies have documented that the reduced pressure from an improved fit is significantly less than capillary closing pressure, an underlying cause of skin breakdown.5 The advent of cleanable and replaceable liners also results in better skin care without the need for multiple collars. Large anterior and posterior openings promote better airflow, increasing patient comfort (Fig. 187-11A). The Aspen CTO (Fig. 187-11B), which incorporates the Aspen cervical collar, gives the practitioner the flexibility of stepping down the level of motion restriction as the patient progresses. The integrated system allows one to go from a four-poster brace to a two-poster brace and finally to a stand-alone cervical collar. Other manufacturers have also developed options and attachments to increase their available applications, such as the Jewett brace (Florida Brace Corporation, Winter Park, FL) anterior and full cervical extensions to the company’s original hyperextension orthosis (Fig. 187-12).

FIGURE 187-12 The original Jewett Brace (Florida Brace Corporation, Winter Park, FL) is now available with a full cervical extension.
(From http://www.flabrace.com.)
The Orthotrac Pneumatic Vest (Orthofix, Inc., Lewisville, TX) represents a unique, noninvasive approach to low back pain. Utilizing a hand pump, the patient activates pneumatic lifters that tie into two custom-fitted belts that shift body weight from the lumbar spine onto the iliac crests (Fig. 187-13). Company literature claims the vest is designed to shift up to 30% to 50% of the body weight off of the spine and distract adjoining vertebral bodies up to 1 mm, which appears sufficient to off-load the spine in most cases.
The latest model of the Halo System (PMT Corporation, Chanhassen, MN) has incorporated several changes to keep up with the times (Fig. 187-14). Simply displacing the buckles yields cleaner lateral radiographs. The use of carbon graphite and titanium materials provides clear MRI or CT scans. New nylon ball joints make assembly quicker and easier. Adjustable headblocks can be independently adjusted to allow anterior-posterior positioning, flexion-extension, and traction-distraction.
Compliance monitors have been developed to objectively assess and optimize patient compliance to prescribed orthoses. Three devices are currently commercially available: the HOBO H8 4-Channel External device, the StowAway TidbiT data logger and temperature sensor, and the IntelliBRACE force sensor system.89
The HOBO H8 4-Channel External device consists of a data logger and a temperature sensor (Fig. 187-15) and is manufactured by Onset Computer Corporation (Bourne, MA). This compliance monitor weighs approximately 1 oz. Data obtained by the HOBO may be uploaded by using Onset Computer Corporation’s BoxCar Pro software and personal computer (PC) interface cable.89
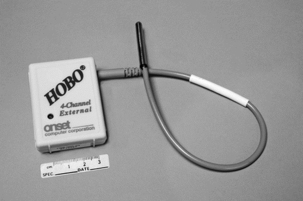
FIGURE 187-15 HOBO H8 4-channel external monitor.
(From Hunter LN, Sison-Williamson M, Mendoza MM, et al: The validity of compliance monitors to assess wearing time of thoracic-lumbar-sacral orthoses in children with spinal cord injury. Spine [Phila Pa 1976] 33[14]:1554–1561, 2008.)
The commercially available StowAway TidbiT consists of a data logger and an internal temperature sensor (Fig. 187-16). This device was adapted for this study by Onset Computer Corporation, the manufacturer, with a permanently attached external temperature sensor. The TidbiT weighs 0.8 ounces and may be mounted to a brace, such as a TLSO, with Velcro. To upload data to a PC also requires the use of Onset Computer Corporation’s BoxCar Pro software. For launching and readout purposes, the StowAway TidbiT uses an Optic Base Station connected to the PC.89
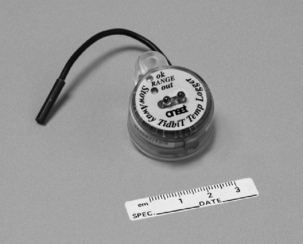
FIGURE 187-16 StowAway TidbiT.
(From Hunter LN, Sison-Williamson M, Mendoza MM, et al: The validity of compliance monitors to assess wearing time of thoracic-lumbar-sacral orthoses in children with spinal cord injury. Spine [Phila Pa 1976] 33[14]:1554–1561, 2008.)
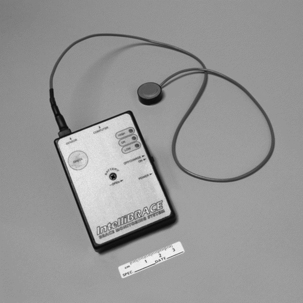
The IntelliBRACE System consists of a data logger and a force sensor that detects pressure (Fig. 187-17). This compliance monitor is manufactured by X3 Technologies (Edmonton, Canada). Data obtained from this compliance monitor were read by using IntelliBRACE Clinical Analysis Software and a PC interface cable.89
Benzel E.C. Spinal orthotics. In: Menezes A.H., Sonntag V.K.H., editors. Principles of spinal surgery. New York: McGraw-Hill; 1996:181-190.
Benzel E.C., Hadden T.A., Saulsbery C.M. A comparison of the Minerva and halo jackets for stabilization of the cervical spine. J Neurosurg. 1989;70:411-414.
Johnson R.M., Hart D.L., Simmons E.F., et al. Cervical orthoses: a study comparing their effectiveness in restricting cervical motion in normal subjects. J Bone Joint Surg [Am]. 1977;59:332-339.
Krag M.H. Biomechanics of the cervical spine: orthoses. In: Frymoyer J.W., editor. The adult spine: principles and practice. ed 2. Philadelphia: Lippincott-Raven; 1997:1110-1117.
Patwardhan A.G., Li S.P., Gavin T., et al. Orthotic stabilization of thoracolumbar injuries: a biomechanical analysis of the Jewett hyperextension orthosis. Spine (Phila Pa 1976). 1990;15:654-661.
Sypert G.W. External spinal orthotics. Neurosurgery. 1987;20:642-649.
White A.A., Panjabi M.M. Clinical biomechanics of the spine. Philadelphia: Lippincott-Raven; 1978.
1. American Association of Orthopedic Surgeons. Atlas of orthoses. St Louis: CV Mosby; 1985.
2. Lucas D.B., Jacobs R.R., Trautman P. Spinal orthotics for pain and instability. In: Redford J.B., editor. Orthotics etcetera. ed 3. Baltimore: Williams & Wilkins; 1986:122-152.
3. Schurr D.G., Cook T.M. Prosthetics and orthotics. Norwalk, CT: Appleton & Lange; 1990. pp 195–215
4. Sypert G.W. External spinal orthotics. Neurosurgery. 1987;20:642-649.
5. Frankel H.L., Hancock D.O., Hyslop G., et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia. 1969;7(3):179-192.
6. Nachemson A.E. Orthotic treatment for injuries and diseases of the spinal column. Phys Med Rehabil. 1987;1:11-24.
7. Ferguson R.L., Allen B.L., Tencer A.F. Biomechanical principles of spinal correction. In: Cotler J.M., Cotler H.B., editors. Spinal fusion: science and technique. New York: Springer-Verlag; 1990:45-57.
8. White A.A., Panjabi M.M. Clinical biomechanics of the spine. Philadelphia: Lippincott-Raven; 1978.
9. Morris J.M., Lucas D.B., Bresler B. Role of the trunk in stability of the spine. J Bone Joint Surg [Am]. 1961;43:327-351.
10. Morris J.M. Spinal bracing. In: Wilkins R.H., Rengachary S.S., editors. Neurosurgery. New York: McGraw-Hill; 1985:2300-2305.
11. Norton P.L., Brown T. The immobilizing efficiency of the back braces: their effect on the posture and motion of the lumbosacral spine. J Bone Joint Surg [Am]. 1957;39:111-139.
12. Waters R.L., Morris J.M. Effect of spinal supports on electrical activity of muscles of the trunk. J Bone Joint Surg [Am]. 1970;52:51-60.
13. Benzel E.C. Spinal orthotics. In: Menezes A.H., Sonntag V.K.H., editors. Principles of spinal surgery. New York: McGraw-Hill; 1996:181-190.
14. Axelsson P., Johnsson R., Stromqvist B. Effect of lumbar orthosis on intervertebral mobility: a roentgen stereophotogrammetric analysis. Spine. 1992;17:678-681.
15. Johnson R.M., Owen J.R., Hart D.L., Callahan R.A. Cervical orthoses: a guide to their selection and use. Clin Orthop Relat Res. 1988;154:34-45.
16. Krag M.H. Biomechanics of the cervical spine: orthoses. In: Frymoyer J.W., editor. The adult spine: principles and practice. ed 2. Philadelphia: Lippincott-Raven; 1997:1110-1117.
17. Smith E.M., Juvinall R.C. Mechanics of orthotics. In: Redford J.B., editor. Orthotics etcetera. ed 3. Baltimore: Williams & Wilkins; 1986:21-51.
18. Madsen B.L., Barth P.W., Vistnes L.M. Pressure sores: overview. In: Lee B.Y., Ostrander L.E., Cochran G.V., Shaw W.W., editors. The spinal cord injured patient: comprehensive management. Philadelphia: WB Saunders; 1991:202-209.
19. Koch R.A., Nickel V.L. The halo-vest: evaluation of motion and forces across the neck. Spine. 1978;3:103-107.
20. Nachemson A.L., Morris J.M. In vivo measurements of intradiscal pressure. J Bone Joint Surg [Am]. 1964;46:1077-1092.
21. Johnson R.M., Hart D.L., Owen J.R., et al. The Yale cervical orthosis: an evaluation of its effectiveness in restricting cervical motion in normal subjects and a comparison with other cervical orthoses. Phys Ther. 1978;58:865-871.
22. Benzel E.C., Hadden T.A., Saulsbery C.M. A comparison of the Minerva and halo jackets for stabilization of the cervical spine. J Neurosurg. 1989;70:411-414.
23. Millington P.J., Ellingsen J.M., Hauswirth B.E., et al. Thermoplastic Minerva body jacket: a practical alternative to current methods of cervical spine stabilization. Phys Ther. 1987;67:223-225.
24. Johnson R.M., Hart D.L., Simmons E.F., et al. Cervical orthoses: a study comparing their effectiveness in restricting cervical motion in normal subjects. J Bone Joint Surg [Am]. 1977;59:332-339.
25. Harris E.E. A new orthotics terminology. Orthotics Prosthet. 1973;27:6-9.
26. Colachis S.C., Strohm B.R., Ganter E.L. Cervical spine motion in normal women: radiographic study of effect of cervical collars. Arch Phys Med Rehabil. 1973;54:161-169.
27. Hartman J.T., Palumbo F., Hill B.J. Cineradiography of braced normal cervical spine: comparative study of five commonly used cervical orthoses. Clin Orthop Relat Res. 1975;109:97-102.
28. Jones M.D. Cineradiographic studies of collar immobilized cervical spine. J Neurosurg. 1960;17:633-637.
29. Fisher S.V., Bowar J.F., Awad E.A., et al. Cervical orthoses’ effect on cervical spine motion: roentgenographic and goniometric method of study. Arch Phys Med Rehabil. 1977;58:109-115.
30. Polin R.S., Szabo T., Bogaev C.A., et al. Nonoperative management of types II and III odontoid fractures: the Philadelphia collar versus the halo vest. Neurosurgery. 1996;38:450-456.
31. Koller H., Zenner J., Hitzl W., et al. In vivo analysis of atlantoaxial motion in individuals immobilized with the halo thoracic vest or Philadelphia collar. Spine. 2009;34(7):670-679.
32. Schneider A.M., Hipp J.A., Nguyen L., Reitman C.A. Reduction in head and intervertebral motion provided by 7 contemporary cervical orthoses in 45 individuals. Spine (Phila Pa 1976). 2007;32(1):E1-E6.
33. Lantz S.A., Schultz A.B. Lumbar spine orthosis wearing: 1. Restriction of gross body motions. Spine (Phila Pa 1976). 1986;11:834-837.
34. Patwardhan A.G., Li S.P., Gavin T., et al. Orthotic stabilization of thoracolumbar injuries: a biomechanical analysis of the Jewett hyperextension orthosis. Spine (Phila Pa 1976). 1990;15:654-661.
35. Lantz S.A., Schultz A.B. Lumbar spine orthosis wearing: 2. Effect on trunk muscle myoelectric activity. Spine (Phila Pa 1976). 1986;11:838-842.
36. Fidler M.W., Plasmans C.M.T. The effect of four types of support on the segmental mobility of the lumbosacral spine. J Bone Joint Surg [Am]. 1983;65:943-947.
37. Axelsson P., Johnsson R., Stromqvist B. Lumbar orthosis with unilateral hip immobilization: effect on intervertebral mobility determined by roentgen stereophotogrammetric analysis. Spine (Phila Pa 1976). 1993;18:876-879.
38. Krag M.H., Begnnon B.D. A new halo-vest: rationale, design and biomechanical comparison to standard halo-vest designs. Spine. 1988;13:228-234.
39. Ivancic P.C., Beauchman N.N., Tweardy L. Effect of halo-vest components on stabilizing the injured cervical spine. Spine (Phila Pa 1976). 2009;34(2):167-175.
40. Maiman D., Millington P., Novak S., et al. The effect of the thermoplastic minerval body jacket on cervical spine motion. Neurosurgery. 1989;25:363-368.
41. Wang G.J., Moskal J.T., Albert T., et al. The effect of halo-vest length on stability of the cervical spine. J Bone Joint Surg [Am]. 1988;70:357-360.
42. Abruzzese R.S. Pressure sores: nursing aspects and prevention. In: Lee B.Y., Ostrander L.E., Cochran G.V., Shaw W.W., editors. The spinal cord injured patient: comprehensive management. Philadelphia: WB Saunders; 1991:210-222.
43. Edberg E.L., Cerny K., Stauffer E.S. Prevention and treatment of pressure sores. Phys Ther. 1973;53:246-252.
44. Landis E.M. Micro-injection studies of capillary blood pressure in human skin. Heart. 1930;15:209-228.
45. Kosiak M. Etiology of decubitus ulcers. Arch Phys Med Rehabil. 1961;42:19-29.
46. Dinsdale S.M. Decubitus ulcers: role of pressure and friction in causation. Arch Phys Med Rehabil. 1974;55:147-152.
47. Daniel R.K., Priest D.L., Wheatly D.C. Etiologic factors in pressure sores: an experimental model. Arch Phys Med Rehabil. 1981;62:492-498.
48. Lee B.Y. Plastic surgery for pressure sores. In: Lee B.Y., Ostrander L.E., Cochran G.V., Shaw W.W., editors. The spinal cord injured patient: comprehensive management. Philadelphia: WB Saunders; 1991:223-230.
49. Botte M.J., Byrne T.P., Abrams R.A., Garfin S.R. Halo skeletal fixation: techniques of application and prevention of complications. J Am Acad Orthop Surg. 1996;4:44-53.
50. Garfin S.R., Botte M.J., Waters R.L., et al. Complications in the use of the halo fixation device. J Bone Joint Surg [Am]. 1986;68:320-325.
51. Glaser J.A., Whitehill R., Stamp W.G., Jane J.A. Complications associated with the halo vest. J Neurosurg. 1986;65:762-769.
52. Lind B., Sihlbom H., Nordwall A. Halo-vest treatment of unstable traumatic cervical spine injuries. Spine (Phila Pa 1976). 1988;13:425-432.
53. Ackland H.M., Cooper D.J., Malham G.M., Kossmann T. Factors predicting cervical collar-related decubitus ulceration in major trauma patients. Spine (Phila Pa 1976). 2007;32(4):423-428.
54. Massie J.B., Heller J.G., Abitbol J.J., et al. Post operative posterior spinal wound infections. Clin Orthop Relat Res. 1992;284:99-108.
55. Korovessis P., Stamatakis M., Baikousis A., et al. Vertical transmission of the hip rolls due to wearing of TLSO for scoliosis. J Spinal Disord. 1996;9:326-333.
56. Johnsson R., Stromqvist B., Axelsson P., Selvik G. Influence of spinal immobilization on consolidation of posterolateral lumbosacral fusion: a roentgen stereophotogrammetric and radiographic analysis. Spine (Phila Pa 1976). 1992;17:16-21.
57. Cooper P.R., Maravilla K.R., Sklar F.H., et al. Halo immobilization of cervical spine fractures: indications and results. J Neurosurg. 1979;50:603-610.
58. Whitehill R., Richman J.A., Glaser J.A. Failure of immobilization of the cervical spine by the halo vest. J Bone Joint Surg [Am]. 1986;68:326-332.
59. Beyer C.A., Cabanela M.E., Berquist T.H. Unilateral facet dislocations and fracture-dislocations of the cervical spine. J Bone Joint Surg [Am]. 1991;73:977-981.
60. Rockswold G.L. Halo management of cervical spine injuries. Contemp Neurosurg. 1991;13:1-6.
61. DiRaimondo C.V., Green N.E. Brace-wear compliance in patients with adolescent idiopathic scoliosis. J Pediatr Orthop. 1988;8(2):143-146.
62. Gurnham R.B. Adolescent compliance with spinal brace wear. Orthop Nurs. 1983;2(6):13-17.
63. Vandal S., Rivard C.H., Bradet R. Measuring the compliance behavior of adolescents wearing orthopedic braces. Issues Compr Pediatr Nurs. 1999;22(2–3):59-73.
64. Helfenstein A., Lankes M., Ohlert K., et al. The objective determination of compliance in treatment of adolescent idiopathic scoliosis with spinal orthoses. Spine (Phila Pa 1976). 2006;31(3):339-344.
65. Takemitsu M., Bowen J.R., Rahman T., et al. Compliance monitoring of brace treatment for patients with idiopathic scoliosis. Spine (Phila Pa 1976). 2004;29(18):2070-2074.
66. Havey R., Gavin T., Patwardhan A., et al. A reliable and accurate method for measuring orthosis wearing time. Spine (Phila Pa 1976). 2002;27(2):211-214.
67. Askins V., Eismont F.J. Efficacy of five cervical orthoses in restricting cervical motion: a comparison study. Spine (Phila Pa 1976). 1997;22(11):1193-1198.
68. Bransford R.J., Stevens D.W., Uyeji S., et al. Halo vest treatment of cervical spine injuries: a success and survivorship analysis. Spine (Phila Pa 1976). 2009;34(15):1561-1566.
69. Bucholz R.D., Cheung K.C. Halo vest versus spinal fusion for cervical injury: evidence from an outcome study. J Neurosurg. 1989;70(6):884-892.
70. Hosssain M., McLean A., Fraser M.H. Outcome of halo immobilisation of 104 cases of cervical spine injury. Scott Med J. 2004;49(3):90-92.
71. Botte M.J., Byrne T.P., Garfin S.J. Application of the halo cervical immobilizer using an increased torque pressure. J Bone Joint Surg [Am]. 1987;69:750-753.
72. Ballock R.T., Botte M.J., Garfin S.R. Complications of halo immobilization. In: Garfin S.R., editor. Complications of spinal surgery. Baltimore: Williams & Wilkins; 1989:376-388.
73. Garfin S.R., Lee T.O., Roux R.D., et al. Structural behavior of the halo orthosis pin-bone interface: biomechanical evaluation of standard and newly designed stainless steel halo fixation pins. Spine (Phila Pa 1976). 1986;11:977-981.
74. Ballock R.T., Lee T.Q., Triggs K.J., et al. The effect of pin localization on the rigidity of the halo-pin interface. Neurosurgery. 1990;26:238-241.
75. Rizzolo S.J., Piazza M.R., Cotler J.M., et al. The effect of torque pressure on halo pin complication rates: a randomized prospective study. Spine (Phila Pa 1976). 1993;18:2163-2166.
76. Whitesides T.E., Mehserle W.L., Hutton W.C. The force exerted by the halo pin: a study comparing different halo systems. Spine (Phila Pa 1976). 1992;17:S413-S417.
77. Kerwin G.A., Chou K.L., White D.B., et al. Investigation of how different halos influence pin forces. Spine (Phila Pa 1976). 1994;19:1078-1081.
78. Goodman M.L., Nelson P.B. Brain abscess complicating the use of a halo orthosis. Neurosurgery. 1987;20:27-29.
79. Rosenblum D., Ehrlich V. Brain abscess and psychosis as a complication of a halo orthosis. Arch Phys Med Rehabil. 1995;76:865-867.
80. Kaplan S.L., Rocco T.P., Tan C.G., et al. Acute pulmonary edema following removal of a spinal orthosis: an unusual complication of a halo vest. Arch Phys Med Rehabil. 1990;71:255-257.
81. Lind B., Bake B., Lundqvist C., Nordwall A. Influence of halo vest treatment on vital capacity. Spine (Phila Pa 1976). 1987;12:449-452.
82. Schwartz D.R., Wirka H.W. The cast syndrome: a case report and discussion of the literature. J Bone Joint Surg [Am]. 1964;46:1549-1552.
83. Roth E.J., Fenton L.L., Gaebler-Spira D.J., et al. Superior mesenteric artery syndrome in acute quadriplegia: case reports and review of the literature. Arch Phys Med Rehabil. 1991;72:417-420.
84. Morishima N., Ohota K., Miura Y. The influences of Halo-vest fixation and cervical hyperextension on swallowing in healthy volunteers. Spine (Phila Pa 1976). 2005;30(7):E179-E182.
85. Bunch W.H., Patwardhan A.G., editors. Scoliosis: making clinical decisions. St Louis: CV Mosby. 1989:237-255.
86. Bengtsson G., Fallstrom K., Jansson B., Nachemson A. A psychiatric investigation of the adjustment of female scoliosis patients. Acta Psychiatr Scand. 1974;50:50-59.
87. Bernstein A., Warner G. Onset of anorexia nervosa after prolonged use of the Milwaukee brace. Psychosomatics. 1983;24:1033-1034.
88. Schatzinger L., Nash C., Drotar D., Hall T. Emotional adjustment in scoliosis. Clin Orthop Relat Res. 1977;125:145-150.
89. Hunter L.N., Sison-Williamson M., Mendoza M.M., et al. The validity of compliance monitors to assess wearing time of thoracic-lumbar-sacral orthoses in children with spinal cord injury. Spine (Phila Pa 1976). 2008;33(14):1554-1561.