Chapter 29 Orthopedics
Rheumatologic disorders
1. Is rheumatoid arthritis (RA) just a disease of the joints and adjacent connective tissue?
2. What are some of the clinical manifestations of RA?
3. What are some airway abnormalities that can occur in patients with rheumatoid arthritis?
4. Why might the normal mouth opening be decreased in patients with rheumatoid arthritis?
5. What occurs to the developing mandible in patients with juvenile rheumatoid arthritis that makes it more difficult to intubate the trachea in this patient population?
6. What are some of the clinical manifestations of cricoarytenoid arthritis?
7. Can neck movement in patients with RA result in cervical spine injury? What is the clinical implication of this?
8. What percent of patients with RA have involvement of their cervical spine?
9. What are three abnormal movements of the cervical spine that may be manifest in patients with rheumatoid arthritis?
10. What is atlantoaxial subluxation?
11. What pathology in RA patients can lead to atlantoaxial subluxation?
12. How is the degree of atlantoaxial subluxation measured? What is this measurement called?
13. What test can be used to determine the atlas-dens interval?
14. What degree of motion between the atlas and dens, or at what atlas-dens interval, is the patient considered to be at risk for spinal cord injury?
15. In the case of pure transverse axial ligament disruption, does flexion or extension increase the atlas-dens interval?
16. If a patient is asymptomatic with neck flexion and extension preoperatively can the anesthesiologist be reassured of an atlas-dens interval of less than 4 mm?
17. What is subaxial subluxation? What is its clinical significance?
18. What is superior migration of the odontoid? What are the potential clinical manifestations?
19. What is the surgical treatment for superior migration of the odontoid?
20. What effect does rheumatoid arthritis have on the trachea?
21. What is the pathology in ankylosing spondylitis?
22. What is the hallmark neck position in patients with ankylosing spondylitis?
23. Ankylosing spondylitis is associated with which HLA type?
24. What are some considerations for the anesthetic management of patients with ankylosing spondylitis?
Spine surgery
25. What are some considerations for the anesthetic management of patients undergoing spine surgery?
26. What are the various surgical approaches to spine surgery? What are the clinical implications of this?
27. What kind of endotracheal tubes can be employed to provide one-lung ventilation for thoracic spine surgery?
28. What is an advantage of a bronchial blocker to provide one-lung ventilation for thoracic spine surgery?
29. What newer technique do surgeons employ during thoracoscopic spine surgery to move the lung from the operative field that does not require one-lung ventilation?
30. Why is intraoperative awareness a possible complication of spine surgery?
31. Is it mandatory to employ a monitor for intraoperative awareness in patients undergoing spine surgery?
32. Name some methods to help decrease blood loss in a patients undergoing spine surgery.
33. What pharmacologic methods exist to diminish blood loss in patients undergoing spine surgery? Why is aprotinin not used?
34. What are some considerations for patients placed in the prone position?
35. Why is spinal cord integrity monitored during spine surgery?
36. What are various methods used to monitor the spinal cord during spine surgery?
37. What are somatosensory evoked potentials (SSEPs)? What part of the spinal cord do they monitor?
38. What changes in latency and amplitude are considered abnormal when monitoring SSEPs during spine surgery?
39. What anesthetic technique should be employed in patients being monitored with somatosensory and/or motor evoked potentials?
40. What are some surgically related conditions that can interfere with spinal cord monitoring waveform acquisition?
41. Why are some areas of the spinal cord more prone to ischemia?
42. What are some factors that can affect intraoperative spinal cord monitoring waveform acquisition?
43. During spine surgery, what is the time course in which changes in the SSEP waveforms manifest after the loss of spinal cord integrity?
44. What is the appropriate management of a patient during spine surgery once significant changes are noted in the spinal cord monitoring waveforms?
45. What area of the spinal cord is monitored by transcranial motor evoked potentials?
46. How does paralysis with neuromuscular blocking drugs affect transcranial motor evoked potentials?
47. Why might masseter muscle contraction occur during transcranial motor evoked potentials monitoring? What is the clinical implication of this?
48. What special precautions should be taken for patients undergoing transcranial motor evoked potentials monitoring during spine surgery?
49. How are intraoperative electromyelograms used to determine if a pedicle screw has been placed too close to a nerve root?
50. Can neuromuscular blockade be in effect when electromyelograms are being obtained?
51. What is the role of the intraoperative wake-up test?
52. How is an intraoperative wake-up test performed?
53. Name potential complications of the intraoperative wake-up test.
54. What considerations are important at the conclusion of a spine procedure?
55. How can postoperative pain be managed in the patient after spine surgery?
56. Which patients are at the greatest risk of postoperative visual loss? What are some other possible factors that contribute to postoperative visual loss?
57. What are some aspects associated with the prone position that may contribute to postoperative visual loss?
58. How much of postoperative visual loss is due to ischemic optic neuropathy?
59. What are the determinants of the ocular perfusion pressure? What is the clinical implication of this?
60. What intraoperative factors has the American Society of Anesthesiologists (ASA) registry determined to be present in the vast majority of postoperative visual loss patients?
61. According to the ASA practice advisory regarding patients at high risk for postoperative visual loss during spine surgery, is the use of deliberate hypotension associated with postoperative visual loss?
62. According to the ASA practice advisory regarding patients at high risk for postoperative visual loss during spine surgery, what type of fluid should be administered with crystalloid in these cases?
63. According to the ASA practice advisory regarding patients at high risk for postoperative visual loss during spine surgery, is there a defined transfusion trigger at which the risk of postoperative visual loss is eliminated?
64. According to the ASA practice advisory regarding patients at high risk for postoperative visual loss during spine surgery, how should the patient’s head and the operating room table be positioned when the patient is prone?
Surgery in the sitting position
65. What neurologic postoperative complications have been noted in patients who undergo surgery in the sitting position?
66. When devastating neurologic postoperative complications occur after surgery in the sitting position, what is the implicated cause?
67. Is the systemic arterial blood pressure at the level of the heart the same as that at the level of the circle of Willis when patients are anesthetized and placed in the sitting position?
68. What calculation more accurately determines the arterial blood pressure at the level of the circle of Willis when one knows the arterial blood pressure at the level of the heart when patients are anesthetized and placed in the sitting position?
69. What superficial landmark correlates with the circle of Willis?
70. What is the potential risk of hypotension in patients that are anesthetized and placed in the sitting position?
Fractured hip
71. Name several factors that predispose a person to a hip fracture.
72. What is the mortality rate associated with a hip fracture?
73. How do comorbidities in the patient with a fractured hip affect their postoperative outcome?
74. Does it make sense to delay surgery in a patient with a fractured hip and significant comorbidity to improve the patient’s medical status prior to surgery?
75. When should patients with a recent myocardial infarction and a fractured hip be scheduled for surgery?
76. What are some considerations for the anesthetic management of patients undergoing hip surgery?
77. Does choice of anesthetic technique—spinal or general anesthesia—play a role in the outcome of patients who have fractured their hip?
78. What are the pros and cons of regional or general anesthesia in the patient with a fractured hip?
79. How are the elderly affected by the use of narcotics in the perioperative period?
Total joint replacement
80. Use of methylmethacrylate cement is associated with what side effects?
81. What is the etiology of the systemic reaction to methylmethacrylate cement?
82. Which patients are at high risk for a systemic reaction to methylmethacrylate cement?
83. What is an appropriate tourniquet inflation pressure for lower extremity surgery?
84. What is the upper limit of tourniquet time before it should be deflated?
85. If tourniquet time exceeds 2 hours and the procedure is not completed, then the tourniquet should be deflated for how long before it is reinflated and why?
86. What are some complications associated with tourniquet use?
87. When does the major amount of blood loss occur during total knee replacement surgery?
88. What are current recommendations for performing a neuraxial block in patients who received enoxaparin?
89. When can redosing of enoxaparin occur after removal of an epidural catheter?
90. What are the current recommendations for performing a neuraxial block in patients taking clopidogrel?
Answers*
Rheumatologic disorders
1. RA is a chronic inflammatory disease, which initially destroys joints and adjacent connective tissue and then progresses to a systemic disease affecting major organ systems. (499, Figure 32-1)
2. Systemic manifestations of RA are widespread. They may include pulmonary involvement with interstitial fibrosis and cysts with honeycombing, gastritis and ulcers from aspirin and other analgesics, neuropathy, nephropathy, muscle wasting, vasculitis, and anemia. Ultimately the anatomy of the airway is damaged and altered in patients with rheumatoid arthritis. (499, Figure 32-1)
3. Some airway abnormalities that can occur in patients with rheumatoid arthritis include decreased mouth opening, a hypoplastic mandible, cricoarytenoid arthritis, and cervical spine abnormalities. (499-500)
4. Normal mouth opening may be decreased in patients with rheumatoid arthritis as a result of temporomandibular arthritis. (499)
5. The patient with juvenile rheumatoid arthritis often has a hypoplastic mandible as a result of early fusion. This results in the noticeable overbite in some patients with RA. (499)
6. As with other joints, the cricoarytenoid joint may be affected by rheumatoid arthritis. Cricoarytenoid arthritis may result in shortness of breath and snoring. RA patients have been misdiagnosed as having sleep apnea when in fact it they have cricoarytenoid arthritis. Patients with cricoarytenoid arthritis may present with stridor on inspiration. This may present in the postanesthesia care unit (PACU) while the patient is recovering from anesthesia. Acute subluxation of the cricoarytenoid joint, as a result of tracheal intubation, can cause stridor as well, and it is not responsive to racemic epinephrine. (500)
7. Yes, movement of the neck in patients with RA can result in cervical spine injury. The patient must be carefully evaluated for both the complexity and the risk of endotracheal intubation because of difficulty in visualizing the airway as a result of the anatomic changes that occur. Normal endotracheal intubation maneuvers with neck movement may result in an increased risk of cervical spine injury due to destruction of the bones and ligaments of the cervical spine. These can place the cervical spinal cord at risk. Many cervical spine abnormalities may occur in patients with RA. (499)
8. The cervical spine is affected in up to 80% of patients with RA. (500)
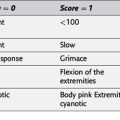
9. Three abnormal movements of the cervical spine that may be manifest in patients with rheumatoid arthritis include atlantoaxial subluxation, subaxial subluxation, and superior migration of the odontoid. (500, Figure 32-2).
10. Atlantoaxial subluxation is the abnormal movement of the C1 cervical vertebra (the atlas) on C2 (the axis). (500)
11. Normally, the transverse axial ligament holds the odontoid process, (also referred to as the dens), which is the superior projection of the vertebra of C2, in place directly behind the anterior arch of C1. With destruction of the transverse axial ligament by RA, movement of the odontoid process is no longer restricted. As the neck is flexed and extended, the C1 vertebra can sublux on the C2 vertebra. This can result in impingement of the spinal cord, placing it at risk for damage. (500-501, Figure 32-3)
12. Subluxation of C1 on C2, referred to as atlantoaxial subluxation, can be quantified by a measuring the distance between the back of the anterior arch of C1 and the front of the dens or odontoid. This distance is referred to as the atlas-dens interval. (501)
13. Flexion and extension radiographs of the cervical spine are obtained to determine the distance between the atlas and dens, or the atlas-dens interval, and thus the degree of subluxation. (501, Figure 32-4)
14. If the atlas-dens interval is 4 mm or more atlantoaxial instability is present, the amount of subluxation is considered significant, and the patient is considered to be at risk for spinal cord injury. (501)
15. In a situation in which the transverse axial ligament is disrupted, extension of the neck minimizes the atlas-dens interval and increases the safe area for the spinal cord. Conversely, flexion of the neck increases the atlas-dens interval and decreases the safe area for the spinal cord, making flexion a more frequent risk position. Still, rheumatoid arthritis affects more than just the transverse axial ligament; therefore, all neck movements in patients with rheumatoid arthritis have to be evaluated carefully as extension of the neck can also lead to problems. (501, Figure 32-5)
16. Patients with rheumatoid arthritis can be asymptomatic with neck flexion and extension preoperatively while awake, and still have an atlas-dens interval of greater than 4 mm and be at risk for cervical spine injury. These patients are able to compensate for their cervical spine instability through local muscle. Once anesthetized and the muscles are relaxed, atlantoaxial subluxation may occur. Therefore the anesthesiologist should not be falsely reassured by asymptomatic flexion and extension in the awake patient. (502)
17. Subaxial subluxation is the subluxation of 15% or more of one cervical vertebra on another at any level below C2. Subaxial subluxation most commonly occurs at the C5-C6 level. Patients with subaxial subluxation are at risk for spinal cord impingement with neck movement. Minimal neck movement is recommended in these patients. (502)
18. Superior migration of the odontoid is a condition where an intact odontoid process projects up through the foramen magnum and into the skull. This occurs because of inflammation and bone destruction that results in cervical spine collapse with sparing of the odontoid process. This can occur because not all areas of the cervical spine are equally affected in any given patient. If the odontoid is spared, the intact odontoid can impinge on the brainstem and patients may suffer neurologic symptoms including quadriparesis or paralysis. (502, Figure 32-6)
19. Surgical treatment for superior migration of the odontoid involves removal of the odontoid to decompress the spinal cord and brainstem. A complicated surgical procedure, referred to as a transoral odontoidectomy, may be performed to accomplish this and involves an incision in the posterior pharyngeal wall, followed by removal of the arch of C1 and then removal of the odontoid and pannus, to relieve neurologic symptoms. With completion of the transoral portion of the procedure, the cervical spine is very unstable, necessitating a posterior spinal fusion. (503)
20. Although the cervical spine is affected by rheumatoid arthritis and may collapse from bone destruction, the trachea is usually spared. This results in the trachea twisting in a characteristic manner as the cervical spine collapses, only serving to increase the difficulty of intubating the trachea of these patients. Tracheal intubation aids such as a fiber optic bronchoscope, Glidescope, Airtraq, or intubating LMA should be available for assistance in endotracheal intubation of these patients should it be required. (503)
21. Ankylosing spondylitis is a rheumatologic disorder in which repetitive minute bone fractures followed by healing results in the characteristic bamboo spine, disease of the sacroiliac joint, fusion of the posterior elements of the spinal column, and fixed neck flexion that is characteristic of this patient population.
22. The hallmark of patients with ankylosing spondylitis is a fused neck in flexion. (503)
23. There is an association between ankylosing spondylitis and HLA-B27, although not all HLA-B27 positive patients are affected with ankylosing spondylitis. (503)
24. Patients with ankylosing spondylitis typically have a rigid cervical spine and neck fused in flexion, which makes endotracheal intubation difficult. Airway manipulation should be performed only after careful assessment, and an intubation assist device can help secure the airway. Patients with ankylosing spondylitis may also develop thoracic and costochondral involvement, which may result in a rapid shallow breathing pattern. (503)
Spine surgery
25. There are several considerations for the anesthetic management of patients undergoing spine surgery, and much depends on the level of the spine in which the surgery will take place, as well as the surgical approach. Preoperative assessment of the patient for underlying neurologic deficits and chronic pain issues are important. For patients in whom the approach may be thoracic, pulmonary function tests may be indicated. In general, spine surgery can be long and complex with significant blood loss and hemodynamic alterations. Intravascular access and intraoperative monitoring should be adjusted accordingly, and blood products may need to be ordered. In the event that there will be intraoperative monitoring of the spinal cord with evoked potentials, the anesthesia administered for the surgery may need to be modified so as not to interfere with the acquisition of waveforms. (503-504)
26. Spine surgery may have anterior, posterior, lateral, and thoracic approaches. In some cases, two approaches may be used during the same surgery. Preoperative discussion with the surgeon is crucial: (1) to determine the surgical approach as it may influence the location of intravascular access and monitoring placement, (2) to ensure proper positioning and padding accessories, and (3) because there may be a need to provide lung isolation and one-lung ventilation. A thoracic surgical approach may involve open thoracotomy or thoracoscopic techniques. High thoracic and thoracoscopic procedures frequently require one-lung ventilation to ensure adequate visualization. (503)
27. A double-lumen endotracheal tube or a bronchial blocker can be employed to provide one-lung ventilation for thoracic spine surgery. (503)
28. A bronchial blocker can be used with a single-lumen endotracheal tube to provide one-lung ventilation for thoracic spine surgery. An advantage of the bronchial blocker is the avoidance of the need to change the tube between different stages of the procedure or at the end of the operation. With the bronchial blocker, deflating the cuff and withdrawing the catheter back into its casing and recapping the proximal end returns the endotracheal tube to its single-lumen tube characteristics. If extubation of the trachea at the end of the surgical procedure is not indicated, the endotracheal tube does not have to be changed, thereby avoiding the issue of changing an endotracheal tube in the presence of potentially significant airway edema. Make certain that the PACU staff is properly educated as to the various ports of the bronchial blocker. (503, Figure 32-7)
29. Some surgeons are using carbon dioxide insufflation as the sole means of moving the lung away from the surgical field even in high thoracic spine surgical procedures. This obviates the need for one-lung ventilation, and allows for the use of a single-lumen endotracheal tube for the entire procedure. (504)
30. Patients undergoing spine surgery appear to be at an increased risk for intraoperative awareness as a result of the requirement that the anesthetic technique administered to them be modified to allow for obtaining adequate intraoperative neurophysiologic monitoring waveforms to assess spinal cord integrity. Therefore, some advocate the use of brain function monitoring in these patients to help avoid intraoperative awareness. (504)
31. Awareness monitoring is not a standard and, as noted in the Practice Advisory for Intraoperative Awareness and Brain Function Monitoring, a decision should be made on a case-by-case basis by the individual practitioner for selected patients (e.g., light anesthesia). There was a consensus in the advisory that brain function monitoring is not routinely indicated for patients undergoing general anesthesia as the “general applicability of these monitors in the prevention of intraoperative awareness had not been established.” In fact, Avidan and associates demonstrated that awareness is not decreased with use of brain function monitoring. The need for brain monitoring is still not clear. (504)
32. Methods to decrease blood loss in spine surgery patients include predonation, hemodilution, wound infusion with a dilute epinephrine solution, hypotensive anesthesia techniques, red blood cell salvage, positioning to diminish venous pressure, careful surgical hemostasis, and the administration of antifibrinolytics. (504)
33. Medications to decrease blood loss during surgery include the antifibrinolytics aprotinin, tranexamic acid, and e-aminocaproic acid. Aprotinin, a serine protease inhibitor, effectively decreased blood loss in cardiac patients and has been demonstrated to be efficacious in patients undergoing spine surgery as well. The negative side effects of aprotinin in cardiac patients include an increased risk of myocardial infarction (MI) or heart failure by approximately 55%, nearly double the risk of stroke, increased risk of long-term mortality, and a higher death rate in patients receiving aprotinin as demonstrated in a study over a 5-year period comparing aprotinin and lysine analogs in high-risk cardiac surgery. The study was terminated early and resulted in relabeling and ultimately withdrawing aprotinin from the market so that it is no longer available. The synthetic lysine analogs, tranexamic acid and e-aminocaproic acid, have also been employed in spine surgery as well as in patients undergoing orthopedic surgery. Tranexamic acid can be administered by an initial bolus injection of 10 mg/kg over 30 minutes followed by a continuous infusion of 1 mg/kg/hr. (504)
34. Spine surgery is often performed with the patient in the prone position. Careful positioning is crucial to avoid patient injury. Movement to the prone position should be performed in a carefully coordinated manner with the surgical team. The neck should not be hyperextended or hyperflexed but placed in the neutral position. The endotracheal tube is positioned so it is not kinked, contact areas are padded, and the face and eyes are protected. Pressure and stretch on nerves is avoided by proper padding and avoiding any extension over 90 degrees. The abdomen needs to be hanging free to avoid increased venous pressure and thereby increased venous bleeding. The prone position alters pulmonary dynamics, so pulmonary function must be reassessed in this position. (504)
35. Monitoring spinal cord integrity is an important component of major surgical procedures involving distraction and rotation of the spine such as occurs with major anteroposterior spinal fusions and scoliosis surgery. Spinal cord monitoring is employed to detect, and hopefully reverse in a timely manner, any adverse effects on the spinal cord noted during the operative period. (505)
36. There are a variety of methods to monitor the spinal cord during spine surgery. These include SSEPs; motor evoked potentials, including transcranial motor evoked potentials, electromyograms (EMGs), or a wake-up test. (505)
37. SSEPs are sensory evoked potential waves generated in the extremities by repetitive stimulation that propagate up through the dorsum or sensory portion of the spinal cord and into the brain, where these signals or waveforms are detected via electrodes placed over the scalp. Specific areas on the scalp coincide with the brain’s sensory areas for the upper and lower extremities and proper signal acquisition obtained over these sites indicates an intact sensory or dorsal portion of the spinal cord. The SSEP waveform generated from multiple repetitive stimulations is analyzed for its latency and amplitude (505, Figure 32-8)
38. An increase in latency of greater than 10% or a decrease in amplitude of 60% or more, as well as the inability to obtain a proper waveform or signal, may be indicative of spinal cord dysfunction or disruption. (505)
39. If SSEPs alone are being monitored, an inhaled anesthetic, equivalent to a small percentage of 1 MAC, can be administered. Volatile anesthetics may interfere with signal acquisition in patients monitored with transcranial motor evoked potentials and may have to be discontinued, if used at all, if adequate signals cannot be obtained. Intravenous anesthetics will need to be administered in these surgical cases. While neuromuscular blockade may be used to facilitate tracheal intubation, paralysis should not be maintained if transcranial motor evoked potentials are being continuously monitored. If the patient is having pedicle screws placed, then the neuromuscular blockade needs to be terminated before the EMGs are obtained so that testing can be properly performed. A small dose of ketamine can be given in the perioperative period as an additional pain relief modality to provide analgesia for major surgery including spine surgery. (504)
40. Surgically related conditions that can result in interference of waveform acquisition during spinal cord monitoring include direct injury or trauma to the cord or impairment of the blood supply. Distraction, rotation, excessive bleeding, and severing or clamping of arterial blood supply can result in ischemia to the cord and neurologic injury. (505)
41. Some areas of the spinal cord are more vulnerable and therefore more prone to ischemia because their blood supply is dependent on watershed blood flow. (505)
42. Many factors can alter intraoperative spinal cord monitoring waveforms unrelated to surgery. These should be properly detected and eliminated. These may include hypotension, hypothermia, high concentrations of volatile anesthetics, benzodiazepines, hypercarbia or hypocarbia, and anemia. Only a small concentration of volatile anesthetic should be employed when SSEP monitoring is used. Midazolam and other benzodiazepines are avoided because they may interfere with obtaining a waveform. Some anesthesiologists even avoid nitrous oxide and use a combination of air in oxygen. (505)
43. Direct injury to the spinal cord results in immediate changes in SSEP waveforms. In contrast, if surgery impairs blood supply and thus renders the spinal cord ischemic, the change in SSEP waveforms may take up to half an hour to manifest. (505)
44. Once a significant change in intraoperative spinal cord monitoring waveforms is noted, specific maneuvers should be used to restore spinal cord blood flow, such as releasing the rotation and distraction of the spine if applicable. In addition, as a result of spinal cord manipulation there may be insufficient blood supply to the spine. Therefore the mean arterial blood pressure should be increased in an effort to restore adequate blood flow to the spine. All variables such as hemoglobin, temperature, arterial carbon dioxide concentration, and arterial blood pressure should be considered. Once these are all evaluated, a wake-up test may be necessary if the waveforms do not improve. (506)
45. Transcranial motor evoked potentials allow for monitoring the patient’s spinal cord motor pathways throughout the entire procedure. Stimulation over the motor cortex of the brain generates a waveform, which is propagated down the motor pathways and detected distally in the arm or leg. This stimulation results in a characteristic waveform. (506, Figure 32-9).
46. To generate transcranial motor evoked potentials, the patient cannot have residual neuromuscular blockade. (506)
47. The electrical current causing the stimulus over the motor cortex during transcranial motor evoked potentials monitoring also stimulates muscles directly in the area of the electrodes placed in the scalp—the masseter muscle and muscles of mastication. This muscle contraction may result in a strong bite, which can potentially injure the tongue, lip, and endotracheal tube. Instances of significant tongue lacerations and damage to endotracheal tubes can occur and this can develop into emergency situations, especially with the patient in the prone position. (506)
48. Special precautions should be taken for patients undergoing transcranial motor evoked potentials monitoring during spine surgery. The tongue should not protrude through the teeth. Placing a bite block made of tongue depressors and gauze in the back of the mouth along the teeth line bilaterally will help prevent injury. In the prone position, any motion may allow for the tongue to slip and fall between the teeth, rendering it vulnerable to laceration. Each stimulus is associated with a masseter muscle contraction, so the patient is at risk as long as waveforms are being generated. (506)
49. Intraoperative electromyelograms are used to determine if a pedicle screw has been placed too close to a nerve root. An electric current is sent through the screw and the electromyelogram is measured distally. If a low milliamp current can stimulate the nerve root, then the screw is too close to the nerve root. In general, a current greater than 7 mA is considered safe enough to know that the pedicle screw is not too close to the nerve root. (506)
50. For accurate electromyelogram testing, residual neuromuscular blockade must be terminated or reversed. (506)
51. The wake-up test was traditionally used to assess spinal cord integrity in many scoliosis cases. Development of sophisticated spinal cord monitoring is now standard in many hospitals and the wake-up test is generally reserved for those situations in which monitoring is unobtainable or a significant intraoperative change in spinal cord monitoring waveforms is noted. (506)
52. The intraoperative wake-up test is performed as follows: turn off all inhaled anesthetics, reverse any neuromuscular blocking drug present, and stop infusions such as dexmedetomidine, propofol, narcotics, or ketamine. If spontaneous respirations do not begin, inject naloxone, 0.04 mg at a time, to reverse any residual narcotic effect. The patient’s head should be held to reduce the risk of self-extubation. Prior to assessing lower extremity function, there should be confirmation of upper extremity function. Patient compliance denotes adequate recovery from general anesthesia. Then, while someone is observing the feet, ask the patient to wiggle his or her toes. A rapid-acting anesthetic such as propofol should be ready to be administered as soon as the assessment is complete, so the patient can rapidly be reanesthetized. If the wake-up test is not successful in demonstrating adequate motor movement, further surgical intervention may be warranted and the patient may require transport to the radiology suite for additional imaging studies. (507)
53. There are some potential complications of an intraoperative wake-up test. These include increased bleeding, venous air embolism, and even inadvertent extubation of the trachea in the prone position with the wound exposed. (506)
54. At the conclusion of a spine procedure, the patient is placed in the supine position. All lines and tubes are secured so that intravenous line, arterial line, and airway access are not lost at this crucial time. Carefully reassess the patient for hemodynamic status, intravascular fluid volume status, hematocrit, blood loss, degree of fluid and blood replacement, temperature, and the potential for airway edema. Premature extubation must be avoided. Also, facial edema, respiratory effort, the amount of pain medication, and the presence of splinting and pain should be evaluated before extubating the trachea. After tracheal extubation, the patient may be transported to the PACU. Supplemental oxygen should be administered in the PACU. Electrolytes, hemoglobin, and clotting studies should be ordered as indicated. (507)
55. Postoperative pain management may prove complicated after spine surgery because some patients may have been taking pain medications preoperatively, particularly opioids. Patient-controlled analgesia (PCA) may be effective, with the dose tailored to the patient’s needs. Some centers use ketamine as an analgesic adjunct. The use of nonsteroidal antiinflammatory drugs (NSAIDs), particularly ketorolac, needs careful consideration because it is a medication that interferes with bone formation and therefore should be avoided in patients who just underwent spinal fusion. NSAIDs may be appropriate when bone healing is not a factor. Other oral medications that are helpful may include acetaminophen, anticonvulsants (e.g., gabapentin and pregabalin), antispasmodics that work at the spinal cord level (e.g., baclofen, tizanidine), antiinflammatory medications, and opioids. (507)
56. Although its etiology is unclear, patients undergoing prolonged spine surgery (> 6 hours) in the prone position who have large blood loss (>1 L) are particularly at risk. Yet, patients with small blood loss and short procedures also have had visual loss. Perioperative factors such as anemia, hypotension, prolonged surgery, blood loss, increased venous pressure from positioning in the prone position, edema, a compartment syndrome within the orbit, and resistance to blood flow, such as from direct pressure on the eye, as well as systemic diseases such as diabetes, hypertension, and vascular disease, are all possible etiologic factors. One recent study entitled Risk Factors Associated with Ischemic Optic Neuropathy (Anesthesiology 2012;116:15-24) has reported that that male sex, obesity, use of a Wilson frame, longer cases, greater estimated blood loss, and a decreased percent of colloid are associated with an increased incidence of postoperative visual loss. (507)
57. There are several aspects of the prone position that may contribute to postoperative visual loss. These include increased venous pressure from positioning in the prone position, edema, a compartment syndrome within the orbit, and resistance to blood flow such as direct pressure on the eye. (507)
58. Ischemic optic neuropathy is a major cause of postoperative visual loss. Variations in the blood supply to the optic nerve may play a role in the development of ischemic optic neuropathy including reliance on a watershed blood supply to critical areas of the optic nerve.
59. Ocular perfusion pressure (OPP), or the blood pressure supplying blood flow to the optic nerve, is a function of the mean arterial pressure (MAP) and intraocular pressure (IOP) such that OPP = MAP − IOP. Increases in IOP or decreases in MAP can have a negative impact on the ocular perfusion pressure. The prone position is associated with increases in intraocular pressure, which can decrease the ocular perfusion pressure and lead to ischemia. The prone position allows edema to develop in the orbit and this increase in venous pressure may impact arterial blood flow. (507)
60. A visual loss registry has been established by the ASA to facilitate establishing the etiology of postoperative visual loss. Also, an ASA practice advisory points to ischemic optic neuropathy as the most likely cause of postoperative visual loss. Of the 93 cases reported in the registry publication, 83 resulted from ischemic optic neuropathy, with the remainder attributed to central retinal artery occlusion. Central retinal artery occlusion may be embolic in nature or the result of direct pressure on the eyeball and tends to be unilateral. Most patients in the registry were healthy and positioned prone for spine surgery. Blood loss of more than 1 L and procedures of 6 hours or longer were present in 96% of cases. (507, Table 32-1)
61. According to the ASA practice advisory regarding patients at high risk for postoperative visual loss during spine surgery, the use of deliberate hypotension has not been shown to be associated with postoperative visual loss. (507, Table 32-1)
62. According to the ASA practice advisory regarding patients at high risk for postoperative visual loss during spine surgery, colloid should be administered in addition to crystalloid to maintain intravascular volume. (507, Table 32-1)
63. According to the ASA practice advisory regarding patients at high risk for postoperative visual loss during spine surgery, there is no defined transfusion trigger at which the risk of postoperative visual loss is eliminated. (507, Table 32-1)
64. According to the ASA practice advisory regarding patients at high risk for postoperative visual loss during spine surgery, when in the prone position the patient’s head should be positioned level with or higher than the heart when possible. Also, when possible, maintain the head in a neutral forward position without significant neck flexion, extension, lateral flexion, or rotation. (507, Table 32-1)
Surgery in the sitting position
65. Postoperative complications that have been noted in the patient undergoing surgery in the sitting position are rare but significant and devastating. These neurologic complications include stroke, ischemic brain injury, and vegetative states. (507)
66. When devastating neurologic postoperative complications occur after surgery in the sitting position, the implicated cause is a decrease in cerebral perfusion pressure resulting in insufficient blood supply to the brain. (508)
67. No, the systemic arterial blood pressure is not the same at the level of the heart as it is at the level of the circle of Willis when patients are anesthetized and placed in the sitting position. This is due to the arterial blood pressure gradient that develops between the heart and brain in this position. (508)
68. When patients are anesthetized and placed in the sitting position, one can more accurately determine the arterial blood pressure at the circle of Willis through the following calculation: for each centimeter of head elevation above the level of the heart there is a decrease in arterial blood pressure of 0.77 mm Hg. Therefore, arterial blood pressure measured at the level of the heart is not the blood and perfusion pressure at the brain. Indeed, a 20-cm difference in height between the heart and the circle of Willis calculates to approximately a 15- to 17-mm Hg gradient. (508)
69. A convenient point for measuring height difference between the heart and brain is the external auditory meatus, which is at the same level as the circle of Willis. Even so, there is still a significant amount of brain tissue above this level. (508)
70. When patients are anesthetized and placed in the sitting position, the mean arterial blood pressure should be maintained to avoid decreases in the cerebral perfusion pressure and to potentially avoid devastating neurologic injury. Thus, hypotension in these patients should be avoided. This is particularly true in the elderly or in patients with chronic hypertension in whom the cerebral autoregulatory curve is altered. (508)
Fractured hip
71. Factors predisposing a person to a hip fracture include medical comorbidities, osteoporosis, lower limb dysfunction, visual impairment, increasing age, Parkinson’s disease, previous fracture, stroke, female gender, dementia, institutionalized patients, excess alcohol or caffeine consumption, cold climate, and use of psychotropic medications. (508)
72. Mortality rates can range up to 14% to 36% in the first year after fracture. (508)
73. Medical status affects morbidity and mortality. One example is the number of comorbidities from which the patient suffers, as in one study the presence of four to six comorbidities is associated with increased mortality rate when compared to patients with less comorbidity. Roche and associates, in studying 2448 patients, reported that the presence of three or more comorbidities was a strong preoperative risk factor with the postoperative development of chest infection or heart failure being associated with a high mortality rate. White and associates reported that ASA I and II patients had mortality rates equal to age-matched control subjects, but ASA III and IV patients had higher mortality rates (49% vs. 8%) after a hip fracture. Moran and colleagues, in a study of 2660 hip fracture patients with an overall mortality rate of 9% at 30 days, 19% at 90 days, and 30% at 12 months, noted that healthy patients did well as long as surgery was performed within 4 days. Patients with comorbidities had a nearly 2.5 times increased mortality rate at 30 days as compared with healthy patients. (508)
74. Generally, when significant comorbidities that need correction exist, patients benefit from a delay in surgery while their medical status improves. The mortality rate in high-risk patients in one study decreased from 29% to 2.9% when time was taken to correct physiologic abnormalities. This was also demonstrated by Kenzora and co-workers, who noted a higher mortality rate (34% vs. 6.9%) in patients who went immediately into surgery as compared to those who were delayed 2 to 5 days to improve their medical status. Also, patients admitted to the hospital immediately after fracture did better than those admitted more than a day later. (508)
75. The management of a patient with a recent myocardial infarction (MI) and hip fracture illustrates how evaluations and management have changed. Previously, surgery was delayed up to 6 months following a myocardial infarction, but now the tendency is to risk-stratify patients based on the severity of their myocardial infarction to determine wait time until surgery. The recent MI needs to be evaluated on a risk-benefit ratio comparing the risk of surgery after a recent MI with the negative side effects of keeping a patient bed bound with its attendant risks of pneumonia, pulmonary embolism, pain, loss of ability to walk, and decubitus ulcers. Factors to consider are the extent of the MI, additional myocardium that may be at risk, if the patient suffers from postinfarct angina, and the presence of congestive heart failure (CHF). Although ongoing angina or the presence of CHF may preclude early surgery, a small subendocardial MI with a minimal increase in cardiac enzymes and normal echocardiogram and stress test would allow consideration for an earlier intervention. A fractured hip usually prevents the patient from undergoing a normal exercise stress test. Therefore, if indicated, a pharmacologic stress test may be needed. (508)
76. Considerations for the anesthetic management of patients undergoing hip surgery include the patient’s intravascular fluid volume status and the potential for significant perioperative blood loss, patient positioning and proper padding on the fracture table, maintaining normothermia, and whatever additional comorbidities may be present as these patients are typically elderly. (509)
77. For patients undergoing hip surgery, there is no clear advantage of one anesthetic technique over another. Therefore, choice of spinal or general anesthesia should be made on a case-by-case basis taking the patient’s specific medical issues into consideration. (508-509)
78. Although no one anesthetic technique has proven to be superior, the pros and cons of both spinal and general anesthesia must be considered when choosing the anesthetic technique for a given patient. Advantages of regional anesthesia, such as provided by a spinal anesthetic, are that (1) it avoids endotracheal intubation and airway manipulation and the medications that need to be administered to accomplish this, (2) it decreases the total amount of systemic medication the patient receives throughout the procedure, and (3) it may play a role in decreasing the risk of thromboembolism. The vasodilatory effect of the spinal anesthetic may help the patient with CHF. However, intravascular fluid still should be given cautiously because CHF may worsen as the intravascular vasodilatory effect of the spinal anesthesia recedes. General anesthesia, in contrast, is easy to administer, particularly in patients in whom movement and positioning for a regional anesthetic may be painful. In addition, in a patient who may be hypovolemic, general anesthesia may be preferred to avoid a precipitous decrease in arterial blood pressure that may occur as a result of the decrease in systemic vascular resistance that accompanies regional anesthesia. (509)
79. The dose and frequency of pain medication given to elderly patients in the perioperative period may need to be decreased, and should be given cautiously because of an increased circulation time, and the cumulative effect of administered opioids may become evident when not expected. (509)
Total joint replacement
80. The use of methylmethacrylate cement is associated with cardiopulmonary side effects such as hypoxia, bronchoconstriction, hypotension, cardiovascular collapse, and even death. (510)
81. The systemic reaction to methylmethacrylate cement may result from the liquid methylmethacrylate cement monomer itself, which is used in producing the cement for cementing the prosthesis, or may be due to air, fat, or bone marrow elements being forced into the circulation. The higher the liquid content of the liquid monomer in the mix with the polymer methylmethacrylate cement at the time of insertion, which occurs from not adequately mixing or not waiting long enough for mixing to occur, the more frequently side effects are noted. (510)
82. Patients who are at high risk for a reaction to methylmethacrylate cement include those who are hypovolemic at the time of cementing, hypertensive patients, and patients with significant preexisting cardiac disease. (510)
83. In the lower extremity surgery, the tourniquet is inflated to approximately 100 mm Hg above the systolic blood pressure, as this will prevent arterial blood from entering the exsanguinated limb. (510)
84. As tourniquets render the limb ischemic, there is a limit to inflation time before the ischemia can result in permanent limb damage. The safe upper limit of ischemia time is considered to be 2 hours. The surgeon should be informed of tourniquet inflation time at 1 hour and then as the tourniquet approaches the 2-hour limit so it can be deflated in a timely manner. (511)
85. If the total tourniquet time will exceed the 2-hour limit, the tourniquet should be deflated at 2 hours for a period of at least 15 to 20 minutes before it is reinflated. This will allow for the “wash-out” of acidic metabolites from the ischemic limb as the limb is reperfused with oxygenated blood. Recirculation of the ischemic limb with release of the tourniquet is noted by a decrease in blood pressure and an increase in end-tidal carbon dioxide as the acid products recirculate. The hypotension usually responds to intravascular fluid administration and vasopressors if necessary. (510)
86. Complications associated with tourniquet use include nerve damage, vessel damage especially in patients with atherosclerosis, pulmonary embolism, and skin damage. One source of skin damage is the antiseptic prep solution, if it is allowed to seep under the tourniquet and tourniquet padding at the time of skin prep, causing a chemical burn. Additional concerns at the time of tourniquet deflation are pulmonary embolism and a decrease in core temperature as the isolated extremity is reperfused. (510)
87. During total knee replacement surgery a tourniquet is used, and in the operating room blood loss is usually not significant. However, if much blood loss occurs into drains in the PACU, hypotension may result. Some surgeons do not deflate the tourniquet until the wound is closed and the dressing is on the patient. In this situation blood loss is usually less but there is a risk of bleeding. (510)
88. Consensus statements from the American Society of Regional Anesthesia and Pain Medicine (ASRA) addressed the issue. Recommendations included waiting at least 10 to 12 hours before neuraxial needle placement in a patient who received a preoperative dose of enoxaparin. (511)
89. Consensus statements from the American Society of Regional Anesthesia and Pain Medicine recommend waiting 2 hours prior to dosing enoxaparin after an epidural catheter is removed. Patients on warfarin should have their catheter removed only when the international normalized ratio (INR) is below 1.5, and care should be taken to avoid other anticoagulants and antiplatelet medications when low-molecular-weight heparin is being used and an epidural catheter is in place. (511)
90. Current recommendations in the ASRA Practice Advisory, Anticoagulation, 3rd edition, 2010, suggest that clopidogrel be discontinued for 7 days prior to performing a neuraxial block. However, the article quotes labeling as recommending this while the PDR section for clopidogrel actually recommends that for elective surgery it only be discontinued for 5 days. The executive summary for the Anesthetic Management of the Patient Receiving Antiplatelet Medication, as part of the third edition, states, “On the basis of labeling and surgical reviews, the suggested time interval between discontinuation of thienopyridine therapy and neuraxial blockade is 14 days for ticlopidine and 7 days for clopidogrel. If a neuraxial block is indicated between 5 and 7 days of discontinuation of clopidogrel, normalization of platelet function should be documented.” In patients who need to be maintained on clopidogrel or who have not discontinued it for an adequate time period, other anesthetic techniques should be considered. The guidelines for some of the antiplatelet medications will probably undergo revision as physicians gain experience with the use of medications such as clopidogrel in the perioperative period. (511)