CHAPTER 17 Orthopaedics
Fractures
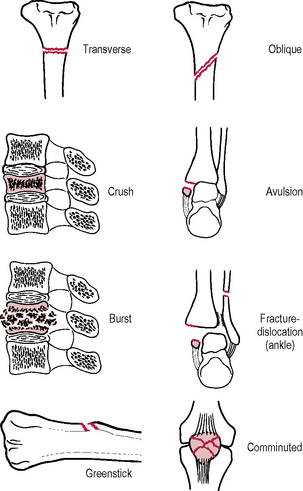
Pattern (→ Fig. 17.1)
Principles of fracture treatment
First aid
Follow Advanced Trauma Life Support (ATLS) principles (→ Ch. 4). Ensure clear airway. Ensure adequate breathing. Stop bleeding. Splintage to prevent further damage by movement of fragments. If open fracture, cover with Betadine-soaked gauze, administer prophylactic antibiotics and check tetanus status.
The fracture itself
Reduction
Methods of stabilizing a fracture
Internal fixation
Indications for internal fixation
Open fractures
Principles of management of open fractures include:
Complications of fractures
Immediate (at time of fracture)
Early (during the period of initial treatment)
Late (after the period of initial treatment)
Avascular necrosis of bone
Part of a bone necroses when its blood supply is interrupted by the fracture. Common sites are:
Spinal trauma
Management of spinal injuries
Scene of the accident
Initial management at the receiving hospital
Fractures and dislocations of the spine
Classification by mechanism of injury
Cervical spine fractures and dislocations
Spinal cord injury
Types of spinal cord injury
Injuries to the lower limb
Hip and thigh
Fractures of the proximal femur
The blood supply to the head of the femur comes from three sources:
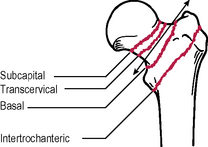
The main source is via the retinacular vessels and these may be damaged in fractures of the femoral neck. Fractures may be classified as intracapsular (subcapital, transcervical), or extracapsular (basal, intertrochanteric → Fig. 17.4). Extracapsular fractures do not damage the blood supply to the femoral head and therefore there are no risks of avascular necrosis of the femoral head and non-union. They are most common in the elderly, especially females with osteoporotic bones when the traumatic cause is relatively trivial, e.g. a fall in the house. In the young patient they result from major trauma.
Fractures of the femoral shaft
Treatment
Surgical
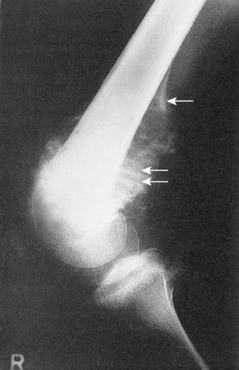
Fractures and dislocations around the knee
Fractures and dislocations of the patellae
Fractures of the tibial shaft
Fractures around the ankle
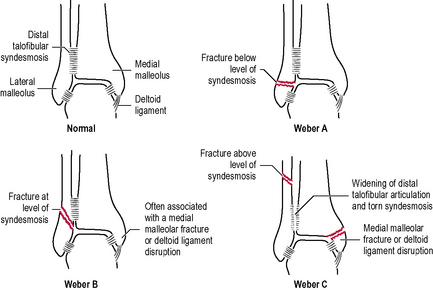
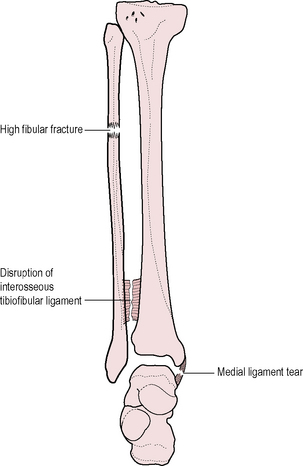
Classification (Fig. 17.7)
Injuries to the upper limb
Fractures and dislocations around the shoulder
Dislocation of the shoulder
Fractures of the humerus
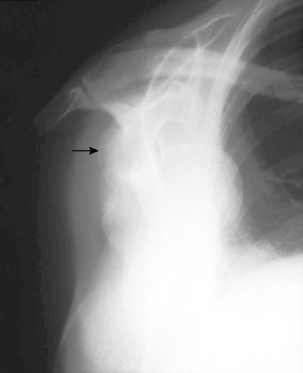
Proximal humerus (→ Fig. 17.10)
This is usually due to indirect violence, i.e. a fall on the shoulder, often in the elderly.
Fractures and dislocations around the elbow
Fractures of the radius and ulna
Fractures of the distal radius
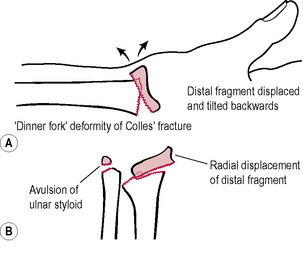
Distal radial fracture
Investigations
Radiograph in two planes (→ Fig. 17.12): distal fragment is displaced dorsally, radially (with pull-off of the ulnar styloid) and supinated; check for intra-articular fracture lines and associated scaphoid fracture.
Fractures and dislocations of the carpal bones
Fractures and dislocations of the metacarpals and phalanges
Fractures and dislocations of the phalanges
These are often serious injuries and may be associated with tendon and nerve damage.
Conditions of joints
Arthritis
Osteoarthritis (osteoarthrosis, OA)
Investigations
Radiographs (→ Fig. 17.13): narrowing of joint space, subchondral bone sclerosis, subchondral cysts, osteophytes, evidence of other underlying pathology. Symptoms do not necessarily correlate with the severity of radiological changes.
Treatment
Conservative
Analgesia: start with mild analgesia, e.g. paracetamol; NSAIDs are usually required eventually.
Surgical
Rheumatoid arthritis (RA)
Arthroplasty
Design of joint replacements
Conditions of menisci, ligaments, tendons, capsules and bursae
Knee
Ligamentous damage
Miscellaneous conditions of the limbs
Infection of bones and joints
Acute infection of bones and joints
Acute osteomyelitis
Chronic infections of bones and joints
Chronic osteomyelitis
Secondary to acute osteomyelitis
Investigations
Bone tumours
Benign tumours
Malignant tumours
Primary
Osteosarcoma (osteogenic sarcoma)
Investigations
Ewing’s tumour (primitive peripheral neuroectodermal tumour)
Investigations
Backache
This is an extremely common complaint accounting for about 20% of musculoskeletal triage referrals. Most cases are either traumatic or degenerative but other causes are numerous (→ Table 17.1). The more common causes will be described in this section.
| Congenital | Kyphoscoliosis |
| Spina bifida | |
| Spondylolisthesis | |
| Acquired Traumatic |
Vertebral fractures |
| Ligamentous injury | |
| Joint strain | |
| Muscle tears | |
| Infective | Osteomyelitis – acute and chronic, TB |
| Inflammatory | Ankylosing spondylitis |
| Discitis | |
| Rheumatology disorders | |
| Neoplastic | Primary tumours (rare) |
| Metastases (common) | |
| Degenerative | Osteoarthritis |
| Intervertebral disc lesions | |
| Metabolic | Osteoporosis |
| Osteomalacia | |
| Endocrine | Cushing’s disease (osteoporosis) |
| Idiopathic | Paget’s disease |
| Scheuermann’s disease | |
| Psychogenic | Psychosomatic backache is common |
| Visceral | Penetrating peptic ulcer |
| Carcinoma of the pancreas | |
| Carcinoma of the rectum | |
| Vascular | Aortic aneurysm |
| Acute aortic dissection | |
| Renal | Carcinoma of the kidney |
| Renal calculus | |
| Inflammatory disease | |
| Gynaecological | Uterine tumours |
| Pelvic inflammatory disease | |
| Endometriosis |
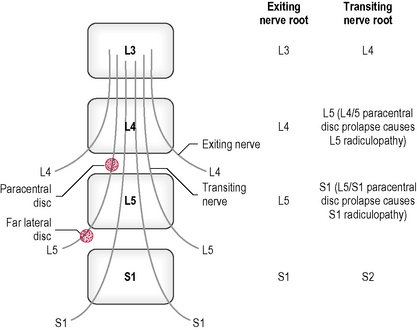
Prolapsed intervertebral disc
This is a common cause of low back pain and sciatica. There is often a history of pain or mild injury, e.g. while lifting. Backache and radicular pain occur. Most disc prolapses are posterior and pass lateral to the posterior longitudinal ligament (paracentral disc) causing compression of the transiting nerve root. Far lateral discs may compress the exiting nerve root also (Fig. 17.16) Central disc prolapses may compress the cord (cord compression) or more commonly, as discs herniated at the level of the cauda equina, cause cauda equina syndrome.
Spondylolisthesis
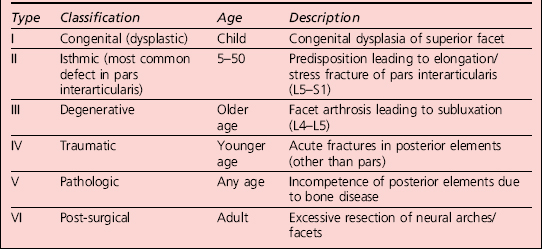
In this condition, one vertebra slips forward relative to the one below, usually L5 on S1 or less commonly L4 on L5. A classification of spondylolisthesis is shown in Table 17.2.
Cervical spondylosis
Metabolic bone disease
Paget’s disease of bone
This is a difficult disease to categorize but is included here for convenience. The aetiology is unknown. Disorderly bone resorption and replacement leads to softening, increased vascularity, painful enlargement and bowing of bones. It occurs in middle to old age and is more common in males. The skull, vertebrae, pelvis and long bones are affected. Some cases are symptomless, being picked up on routine radiograph (→ Fig. 17.19). Complications include compressive symptoms due to skull enlargement (e.g. blindness, deafness, cranial nerve entrapment), paraplegia, pathological fractures, high-output cardiac failure due to vascularity of bone. Osteogenic sarcoma may develop after many years. In mild cases no treatment is required. In severe cases, calcitonin and bisphosphonates may help.
Paediatric orthopaedics
Scoliosis
Conditions of the hip
Development dysplasia of the hip (DDH)
Irritable hip
Perthes’ disease
Symptoms and signs
Pain in the groin or referred to the knee. Otherwise well. Decreased range of joint movements.