Chapter 86 Organ Donation
1 Who governs the rules and regulations for organ donation?
 The Organ Procurement and Transplantation Network (OPTN) is a system for operating and monitoring the unbiased allocation, through established medical criteria, of organs donated for transplantation and maintaining a recipients’ waiting list (including the listing and delisting of recipients).
The Organ Procurement and Transplantation Network (OPTN) is a system for operating and monitoring the unbiased allocation, through established medical criteria, of organs donated for transplantation and maintaining a recipients’ waiting list (including the listing and delisting of recipients).
 The United Network for Organ Sharing (UNOS) is a nonprofit organization awarded the contract by the Department of Health and Human Services in 1986 to implement the OPTN.
The United Network for Organ Sharing (UNOS) is a nonprofit organization awarded the contract by the Department of Health and Human Services in 1986 to implement the OPTN.
 Organ Procurement Organizations (OPO) serve specific regions in the country for clinical services including working with hospital staff to maintain donor-organ function, working with UNOS to match donor organs with recipients, coordinating organ recovery surgery, and giving compassionate and professional support to donors’ families.
Organ Procurement Organizations (OPO) serve specific regions in the country for clinical services including working with hospital staff to maintain donor-organ function, working with UNOS to match donor organs with recipients, coordinating organ recovery surgery, and giving compassionate and professional support to donors’ families.
4 What is the current standard for organ donation?
Organ donation is possible in patients who are declared brain dead. New brain death guidelines have been published (see Box 86-1). Despite efforts to promote organ donation, an enormous shortage of available organs for transplant continues to exist. As a result, efforts have been undertaken to expand the settings in which organs may become available (i.e., donation after cardiac death (DCD); see later). See Boxes 86-2, 86-3, and 86-4 and Tables 86-1 and 86-2.
Box 86-1 Brain death criteria
 Core body temperature (≥ 32° C)
Core body temperature (≥ 32° C)
 Absence of cerebral motor responses to pain in all extremities
Absence of cerebral motor responses to pain in all extremities
 Absence of brainstem reflexes, that is, pupillary, oculocephalic (doll’s eyes), vestibuloocular (cold calorics), corneal, gag, and cough reflexes
Absence of brainstem reflexes, that is, pupillary, oculocephalic (doll’s eyes), vestibuloocular (cold calorics), corneal, gag, and cough reflexes
 Apnea test (see Boxes 86–2, 86–3, and 86–4)
Apnea test (see Boxes 86–2, 86–3, and 86–4)
 Exclusion of conditions that may confound clinical assessment of brain death, that is, metabolic or endocrine abnormality or drug intoxication
Exclusion of conditions that may confound clinical assessment of brain death, that is, metabolic or endocrine abnormality or drug intoxication
| Electroencephalography | No electrical activity for a period of 30 minutes |
|---|---|
| Cerebral angiography | No intracerebral filling at the level of the carotid bifurcation or circle of Willis Patent external carotid circulation |
| Transcranial Doppler sonography | No diastolic or reverberating flow Systolic-only or retrograde diastolic flow Small systolic peaks in early systole |
| Somatosensory evoked potential | Bilateral absence of response to medial nerve stimulation |
| Cerebral scintigraphy (technetium Tc 99m brain scan) | No uptake of radionuclide in brain parenchyma (hollow skull phenomenon) |
| Magnetic resonance imaging | Not yet determined |
Table 86-2 Comparison of donation after brain death and donation after cardiac death
| Donation after brain death | Donation after cardiac death | |
|---|---|---|
| Cause of illness (e.g., anoxic, trauma, stroke) | Severe irreversible brain injury Does meet criteria of brain death |
Severe irreversible brain injury Does not meet criteria of brain death |
| Organ procurement process | Physician (non–transplant team) declares brain death | Family elects withdrawal of life support |
| Referral to OPO | Referral to OPO | |
| Await OR time for organ procurement | Withdrawal of life support in the OR or ICU | |
| Transplant team retrieves organs | Physician (non–transplant team) declares cardiac death | |
| Heart, lungs, kidneys, liver, pancreas, and/or intestines are transplantable | Transplant team waits 5 minutes after cardiac death is declared before procuring organs | |
| Transplant team retrieves organs | ||
| Kidney, pancreas, and liver are generally transplantable |
OR, Operating room.
Modified from Organ Donation After Cardiac Death. Madison, Wis., University of Wisconsin Organ Procurement Organization, 2009.
Box 86-3 Apnea test
1. Patient is disconnected from the ventilator.
2. Oxygen cannula is placed at the level of carina, and 100% oxygen is delivered at a rate of 6 L/min.
3. Patient is observed for respiratory movements (e.g., chest or abdominal excursions).
4. Arterial PaO2, PaCO2, and pH are measured after approximately 8 minutes.
Box 86-4 Interpretation of apnea test results
Confirmatory results: No respiratory movements witnessed with resultant arterial PCO2 ≥ 60 mm Hg (or 20 mm Hg increase in PCO2 over pretest baseline)
Contradictory results: Any evidence of respiratory movements (regardless of PCO2 level)
Inconclusive results: No respiratory movements and PCO2 ≤ 60 mm Hg. Apnea test may be repeated within 10 minutes.
If cardiovascular or pulmonary instability occurs during the test (i.e., systolic blood pressure ≤ 90 mm Hg, dysrhythmia, or arterial oxygen desaturation), arterial blood gas value is immediately obtained, and the patient is reconnected to the ventilator. Alternative confirmatory testing to determine brain death (see Table 86–1) is then performed at the discretion of physician.
8 What are some of the statistics for organ donation and transplantation?
 Every 11 minutes, a patient is added to the transplant waiting list (e.g., lung, kidney, heart).
Every 11 minutes, a patient is added to the transplant waiting list (e.g., lung, kidney, heart).
 Every day, approximately 75 patients receive an organ transplant. Yet every day approximately 20 patients die waiting for a transplant.
Every day, approximately 75 patients receive an organ transplant. Yet every day approximately 20 patients die waiting for a transplant.
 As of May 4, 2009, the percentage of recipients who were still living 5 years after solid organ transplantation was as follows:
As of May 4, 2009, the percentage of recipients who were still living 5 years after solid organ transplantation was as follows:
 In 2008, 60% of living donors were women. Sixty percent of deceased donors were men.
In 2008, 60% of living donors were women. Sixty percent of deceased donors were men.
 In 2008, 67% of all deceased donors were white, 16% were black, 14% Hispanic, and 2.5% Asian.
In 2008, 67% of all deceased donors were white, 16% were black, 14% Hispanic, and 2.5% Asian.
 As of November 2010, patients on the national waiting list were 45% white, 29% black, 18% Hispanic, and 6% Asian.
As of November 2010, patients on the national waiting list were 45% white, 29% black, 18% Hispanic, and 6% Asian.
 In 2007 (the most recent data), nearly 2.5 million people died in the United States. Yet only 8085 of these people donated their organs.
In 2007 (the most recent data), nearly 2.5 million people died in the United States. Yet only 8085 of these people donated their organs.
 OPTN data show a progressive increase in the rate of organ recovery from DCD donors (844 DCD donors in 2008 compared with 268 in 2003).
OPTN data show a progressive increase in the rate of organ recovery from DCD donors (844 DCD donors in 2008 compared with 268 in 2003).
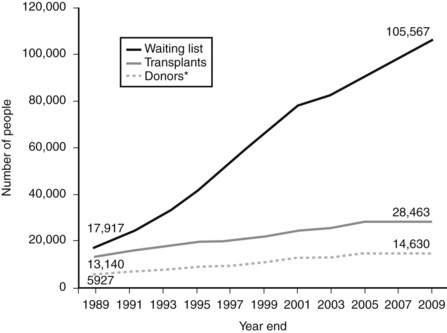
 Currently, more than 86 million people in the United States have indicated a wish to become a donor. Although impressive at first, this still will not be nearly enough to address the growing demand (see Fig. 86-1).
Currently, more than 86 million people in the United States have indicated a wish to become a donor. Although impressive at first, this still will not be nearly enough to address the growing demand (see Fig. 86-1).
Key Points Organ donation
1. All patients with impending brain death or withdrawal of care should be screened for the possibility of organ donation.
2. To diagnose brain death all confounding factors must be excluded.
3. DCD is an ethically acceptable manner in which terminally ill patients can be considered for organ donation.
4. The gap between those patients awaiting transplants and those donating organs is widening exponentially—the vast majority of those on the transplant list will die waiting.
1 Bernat J.L., D’Alessandro A.M., Port F.K., et al. Report of a national conference on donation after cardiac death. Am J Transplant. 2006;6:281–291.
2 Cypel M., Sato M., Yildirim E., et al. Initial experience with lung donation after cardiocirculatory death in Canada. J Heart Lung Transplant. 2009;28:753–758.
3 Truog R.D., Miller F.G. The dead donor rule and organ transplantation. N Engl J Med. 2008;359:674–675.
4 Wijdicks E.F., Varelas P.N., Gronseth G.S., et al. Evidence-based guideline update: determining brain death in adults. Neurology. 2010;74:1911–1918.